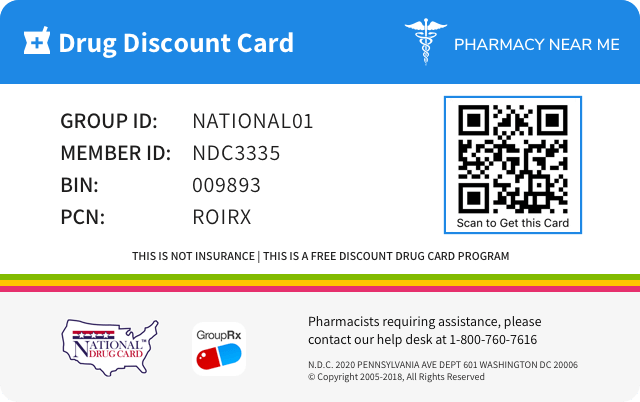
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 99207-525 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug Name | Vanos |
||||||||
| Type | Brand | ||||||||
| Pharm Class | Corticosteroid Hormone Receptor Agonists [MoA], Corticosteroid [EPC] |
||||||||
| Active Ingredients |
|
||||||||
| Route | TOPICAL | ||||||||
| Dosage Form | CREAM | ||||||||
| RxCUI drug identifier | 485647, 543484 |
||||||||
| Application Number | NDA021758 | ||||||||
| Labeler Name | Bausch Health US, LLC | ||||||||
| Packages |
|
||||||||
| Check if available Online | Get Medication Prices online with Discount |
Overdosage of Vanos
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE Topically applied VANOS Cream can be absorbed in sufficient amounts to produce systemic effects [see Warnings and Precautions (5.1) ] .
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS The most commonly reported adverse reactions (≥1%) were headache, application site burning, nasopharyngitis, and nasal congestion. ( 6 ) To report SUSPECTED ADVERSE REACTIONS, contact Valeant Pharmaceuticals North America LLC at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. 6.1 Clinical Trials Experience Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice. In clinical trials, a total of 443 adult subjects with atopic dermatitis or plaque-type psoriasis were treated once daily or twice daily with VANOS Cream for 2 weeks. The most commonly observed adverse reactions in these clinical trials were as follows: Table 1: Most Commonly Observed Adverse Reactions (≥1%) in Adult Clinical Trials Adverse Reaction VANOS Cream, once daily (n=216) VANOS Cream, twice daily (n=227) Vehicle Cream, once or twice daily (n=211) Headache 8 (3.7%) 9 (4.0%) 6 (2.8%) Application Site Burning 5 (2.3%) 4 (1.8%) 14 (6.6%) Nasopharyngitis 2 (0.9%) 3 (1.3%) 3 (1.4%) Nasal Congestion 3 (1.4%) 1 (0.4%) 0 Safety in patients 12 to 17 years of age was similar to that observed in adults. 6.2 Postmarketing Experience The following adverse reactions have been identified during postapproval use of VANOS Cream: Administration Site Conditions: discoloration, erythema, irritation, pruritus, swelling, pain, and condition aggravated. Immune System Disorders: hypersensitivity. Nervous System Disorders: headache and dizziness. Skin and Subcutaneous Tissue Disorders: acne, dry skin, rash, skin exfoliation, and skin tightness. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Corticosteroids play a role in cellular signaling, immune function, inflammation, and protein regulation; however, the precise mechanism of action of VANOS Cream in corticosteroid responsive dermatoses is unknown. 12.2 Pharmacodynamics Vasoconstrictor studies performed with VANOS Cream in healthy subjects indicate that it is in the super-high range of potency as compared with other topical corticosteroids; however, similar blanching scores do not necessarily imply therapeutic equivalence. Application of VANOS Cream twice daily for 14 days in 18 adult subjects with plaque-type psoriasis (10–50% BSA, mean 19.6% BSA) and 31 adult subjects (17 treated once daily; 14 treated twice daily) with atopic dermatitis (2–10% BSA, mean 5% BSA) showed demonstrable HPA-axis suppression in 2 subjects with psoriasis (with 12% and 25% BSA) and 1 subject with atopic dermatitis (treated once daily, 4% BSA) where the criterion for HPA-axis suppression is a serum cortisol level of less than or equal to 18 micrograms per deciliter 30 minutes after stimulation with cosyntropin (ACTH 1-24 ) [see Warnings and Precautions (5.1) ] . HPA-axis suppression following application of VANOS Cream, 0.1% (once or twice daily) was also evaluated in 123 pediatric patients from 3 months to <18 years of age with atopic dermatitis (mean BSA range 34.6%-40.0%). HPA-axis suppression was observed in 4 patients in the twice-daily groups. Follow-up testing 14 days after treatment discontinuation demonstrated a normally responsive HPA axis in all 4 suppressed patients [see Warnings and Precautions (5.1) and Use in Specific Populations (8.4) ] . 12.3 Pharmacokinetics The extent of percutaneous absorption of topical corticosteroids is determined by many factors including the vehicle and the integrity of the epidermal barrier. Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin may increase percutaneous absorption.
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action Corticosteroids play a role in cellular signaling, immune function, inflammation, and protein regulation; however, the precise mechanism of action of VANOS Cream in corticosteroid responsive dermatoses is unknown.
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Vasoconstrictor studies performed with VANOS Cream in healthy subjects indicate that it is in the super-high range of potency as compared with other topical corticosteroids; however, similar blanching scores do not necessarily imply therapeutic equivalence. Application of VANOS Cream twice daily for 14 days in 18 adult subjects with plaque-type psoriasis (10–50% BSA, mean 19.6% BSA) and 31 adult subjects (17 treated once daily; 14 treated twice daily) with atopic dermatitis (2–10% BSA, mean 5% BSA) showed demonstrable HPA-axis suppression in 2 subjects with psoriasis (with 12% and 25% BSA) and 1 subject with atopic dermatitis (treated once daily, 4% BSA) where the criterion for HPA-axis suppression is a serum cortisol level of less than or equal to 18 micrograms per deciliter 30 minutes after stimulation with cosyntropin (ACTH 1-24 ) [see Warnings and Precautions (5.1) ] . HPA-axis suppression following application of VANOS Cream, 0.1% (once or twice daily) was also evaluated in 123 pediatric patients from 3 months to <18 years of age with atopic dermatitis (mean BSA range 34.6%-40.0%). HPA-axis suppression was observed in 4 patients in the twice-daily groups. Follow-up testing 14 days after treatment discontinuation demonstrated a normally responsive HPA axis in all 4 suppressed patients [see Warnings and Precautions (5.1) and Use in Specific Populations (8.4) ] .
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics The extent of percutaneous absorption of topical corticosteroids is determined by many factors including the vehicle and the integrity of the epidermal barrier. Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin may increase percutaneous absorption.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS None. None ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION VANOS (fluocinonide) Cream, 0.1% contains fluocinonide, a synthetic corticosteroid for topical dermatologic use. The corticosteroids constitute a class of primarily synthetic steroids used topically as anti-inflammatory and antipruritic agents. Fluocinonide has the chemical name 6 alpha, 9 alpha-difluoro-11 beta, 21-dihydroxy-16 alpha, 17 alpha-isopropylidenedioxypregna-1, 4-diene-3,20-dione 21-acetate. Its chemical formula is C 26 H 32 F 2 O 7 and it has a molecular weight of 494.58. It has the following chemical structure: Fluocinonide is an almost odorless white to creamy white crystalline powder. It is practically insoluble in water and slightly soluble in ethanol. Each gram of VANOS Cream contains 1 mg micronized fluocinonide in a cream base of anhydrous citric acid USP, carbopol 980 NF, diisopropanolamine, dimethyl isosorbide, glyceryl monostearate NF, glyceryl stearate (and) PEG-100 stearate, propylene glycol USP, and purified water USP. Chemical Structure
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION For topical use only. VANOS Cream is not for ophthalmic, oral, or intravaginal use. For psoriasis, apply a thin layer of VANOS Cream once or twice daily to the affected skin areas as directed by a physician. Twice-daily application for the treatment of psoriasis has been shown to be more effective in achieving treatment success during 2 weeks of treatment. For atopic dermatitis, apply a thin layer of VANOS Cream once daily to the affected skin areas as directed by a physician. Once-daily application for the treatment of atopic dermatitis has been shown to be as effective as twice daily treatment in achieving treatment success during 2 weeks of treatment [see Clinical Studies (14) ] . For corticosteroid responsive dermatoses, other than psoriasis or atopic dermatitis, apply a thin layer of VANOS Cream once or twice daily to the affected areas as directed by a physician. For topical use only. VANOS Cream is not for ophthalmic, oral, or intravaginal use. ( 2 ) Psoriasis: apply a thin layer once or twice daily to the affected skin areas. ( 2 ) Atopic Dermatitis: apply a thin layer once daily to the affected skin areas. ( 2 ) Corticosteroid Responsive Dermatoses, other than psoriasis or atopic dermatitis: apply a thin layer once or twice daily to the affected areas. ( 2 )
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Cream, 0.1%. Each gram of VANOS Cream contains 1 mg of fluocinonide in a white to off-white cream base. Cream, 0.1% ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE VANOS Cream is a corticosteroid indicated for the relief of the inflammatory and pruritic manifestations of corticosteroid responsive dermatoses in patients 12 years of age or older. ( 1 ) Limitation of Use: Treatment beyond 2 consecutive weeks is not recommended, and the total dosage should not exceed 60 g per week because of the potential for the drug to suppress the hypothalamic-pituitary-adrenal (HPA) axis. ( 1 ) Avoid use on the face, groin, or axillae. ( 1.2 ) Avoid use in perioral dermatitis or rosacea. ( 1.2 ) 1.1 Indications VANOS ® (fluocinonide) Cream, 0.1% is indicated for the relief of the inflammatory and pruritic manifestations of corticosteroid responsive dermatoses in patients 12 years of age or older [see Use in Specific Populations (8.4) ] . 1.2 Limitation of Use Treatment beyond 2 consecutive weeks is not recommended and the total dosage should not exceed 60 g per week because the safety of VANOS Cream for longer than 2 weeks has not been established and because of the potential for the drug to suppress the hypothalamic-pituitary-adrenal (HPA) axis. Therapy should be discontinued when control of the disease is achieved. If no improvement is seen within 2 weeks, reassessment of the diagnosis may be necessary. Do not use more than half of the 120 g tube per week. VANOS Cream should not be used in the treatment of rosacea or perioral dermatitis, and should not be used on the face, groin, or axillae.
Spl product data elements
Usually a list of ingredients in a drug product.Vanos fluocinonide ANHYDROUS CITRIC ACID CARBOMER HOMOPOLYMER TYPE C (ALLYL PENTAERYTHRITOL CROSSLINKED) DIISOPROPANOLAMINE DIMETHYL ISOSORBIDE GLYCERYL MONOSTEARATE PEG-100 STEARATE PROPYLENE GLYCOL WATER FLUOCINONIDE FLUOCINONIDE
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Long-term animal studies have not been performed to evaluate the carcinogenic potential of VANOS Cream because of severe immunosuppression induced in a 13-week dermal rat study. The effects of fluocinonide on fertility have not been evaluated. Fluocinonide revealed no evidence of mutagenic or clastogenic potential based on the results of two in vitro genotoxicity tests (Ames test and chromosomal aberration assay using human lymphocytes). However, fluocinonide was positive for clastogenic potential when tested in the in vivo mouse micronucleus assay. Topical (dermal) application of 0.0003%–0.03% fluocinonide cream to rats once daily for 13 weeks resulted in a toxicity profile generally associated with long-term exposure to corticosteroids including decreased skin thickness, adrenal atrophy, and severe immunosuppression. A NOAEL could not be determined in this study. In addition, topical (dermal) application of 0.1% fluocinonide cream plus ultraviolet radiation (UVR) exposure to hairless mice for 13 weeks and 150–900 mg/kg/day of 0.1% fluocinonide cream to minipigs (a model which more closely approximates human skin) for 13 weeks produced glucocorticoid-related suppression of the HPA axis, with some signs of immunosuppression noted in the dermal minipig study. Although the clinical relevance of the findings in animals to humans is not clear, sustained glucocorticoid-related immune suppression may increase the risk of infection and possibly the risk for carcinogenesis. Topical doses of 0% (fluocinonide cream vehicle), 0.0001%, 0.005%, and 0.001% fluocinonide cream were evaluated in a 52-week dermal photocarcinogenicity study (40 weeks of treatment followed by 12 weeks of observation) conducted in hairless albino mice with concurrent exposure to low level ultraviolet radiation. Topical treatment with increasing concentrations of fluocinonide cream did not have an adverse effect in this study. The results of this study suggest that topical treatment with VANOS Cream would not enhance photocarcinogenesis.
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Long-term animal studies have not been performed to evaluate the carcinogenic potential of VANOS Cream because of severe immunosuppression induced in a 13-week dermal rat study. The effects of fluocinonide on fertility have not been evaluated. Fluocinonide revealed no evidence of mutagenic or clastogenic potential based on the results of two in vitro genotoxicity tests (Ames test and chromosomal aberration assay using human lymphocytes). However, fluocinonide was positive for clastogenic potential when tested in the in vivo mouse micronucleus assay. Topical (dermal) application of 0.0003%–0.03% fluocinonide cream to rats once daily for 13 weeks resulted in a toxicity profile generally associated with long-term exposure to corticosteroids including decreased skin thickness, adrenal atrophy, and severe immunosuppression. A NOAEL could not be determined in this study. In addition, topical (dermal) application of 0.1% fluocinonide cream plus ultraviolet radiation (UVR) exposure to hairless mice for 13 weeks and 150–900 mg/kg/day of 0.1% fluocinonide cream to minipigs (a model which more closely approximates human skin) for 13 weeks produced glucocorticoid-related suppression of the HPA axis, with some signs of immunosuppression noted in the dermal minipig study. Although the clinical relevance of the findings in animals to humans is not clear, sustained glucocorticoid-related immune suppression may increase the risk of infection and possibly the risk for carcinogenesis. Topical doses of 0% (fluocinonide cream vehicle), 0.0001%, 0.005%, and 0.001% fluocinonide cream were evaluated in a 52-week dermal photocarcinogenicity study (40 weeks of treatment followed by 12 weeks of observation) conducted in hairless albino mice with concurrent exposure to low level ultraviolet radiation. Topical treatment with increasing concentrations of fluocinonide cream did not have an adverse effect in this study. The results of this study suggest that topical treatment with VANOS Cream would not enhance photocarcinogenesis.
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PRINCIPAL DISPLAY PANEL - 120 g Tube Carton NDC 99207-525-10 Vanos ® (fluocinonide) Cream, 0.1% FOR TOPICAL USE ONLY NOT FOR OPHTHALMIC, ORAL, OR INTRAVAGINAL USE Rx only Net. Wt. 120 g VALEANT 9481503 carton
Vanos: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Advise the patient to read the FDA-approved patient labeling (Patient Information). Patients using VANOS Cream should receive the following information and instructions. This information is intended to aid in the safe and effective use of this medication. It is not a disclosure of all possible adverse or unintended effects: VANOS Cream is to be used as directed by the physician. It is for external use only. Avoid contact with the eyes. It should not be used on the face, groin, and underarms. VANOS Cream should not be used for any disorder other than that for which it was prescribed. The treated skin area should not be bandaged or otherwise covered or wrapped, so as to be occlusive unless directed by the physician. Patients should report to their physician any signs of local adverse reactions. Other corticosteroid-containing products should not be used with VANOS Cream without first talking to the physician. As with other corticosteroids, therapy should be discontinued when control is achieved. If no improvement is seen in 2 weeks, the patient should be instructed to contact a physician. The safety of the use of VANOS Cream for longer than 2 weeks has not been established. Patients should be informed to not use more than 60 g per week of VANOS Cream. Do not use more than half of the 120 g tube per week. Patients should inform their physicians that they are using VANOS Cream if surgery is contemplated. Patients should wash their hands after applying medication. Manufactured for: Valeant Pharmaceuticals North America LLC Bridgewater, NJ 08807 USA By: Valeant Pharmaceuticals International, Inc. Laval, Quebec H7L 4A8, Canada U.S. Patent Numbers 6,765,001; 7,217,422; 7,220,424; 7,771,733; 7,794,738 and 8,232,264 Vanos is a trademark of Valeant Pharmaceuticals International, Inc. or its affiliates. ©Valeant Pharmaceuticals North America LLC 9481801
Spl patient package insert
Information necessary for patients to use the drug safely and effectively.Patient Information VANOS ® (VAN-ōs) (fluocinonide) Cream, 0.1% IMPORTANT: For skin use only. Do not get VANOS Cream in your eyes, mouth, or vagina. Not for use on the face, groin, or underarms. Read the Patient Information that comes with VANOS Cream before you start using it and each time you get a refill. There may be new information. This leaflet does not take the place of talking to your doctor about your condition or treatment. What is VANOS Cream? VANOS Cream is a prescription corticosteroid medicine used on the skin (topical) to treat adults and children 12 years and older with certain skin conditions that cause red, flaky, and itchy skin. You should not use VANOS Cream for longer than 2 weeks in a row. You should not use more than 60 grams of VANOS Cream or more than half of the 120 gram tube in 1 week. VANOS Cream should not be used: if you have skin swelling or redness on the nose or face (rosacea) for a scaly or bumpy rash around your mouth (perioral dermatitis) on your face, underarms, or groin area It is not known if VANOS Cream is safe and effective in children under 12 years of age. What should I tell my doctor before using VANOS Cream? Before using VANOS Cream, tell your doctor if you: have had irritation or other skin reaction to a steroid medicine in the past adrenal gland problems plan to have surgery are pregnant or plan to become pregnant. It is not known if VANOS Cream will harm your unborn baby. Talk to your doctor if you are pregnant or plan to become pregnant. are breast-feeding or plan to breastfeed. It is not known if VANOS Cream passes into your breast milk. Talk to your doctor about the best way to feed your baby if you use VANOS Cream. Tell your doctor about all the medicine you take including prescription and nonprescription medicines, vitamins, and herbal supplements. Especially tell your doctor if you take a corticosteroid medicine by mouth or use other products on your skin that contain corticosteroids. Ask your doctor or pharmacist if you are not sure. Know the medicines you take. Keep a list of your medicines with you to show your doctor and pharmacist when you get a new medicine. How should I use VANOS Cream? See “What is VANOS Cream?” Use VANOS Cream exactly as your doctor tells you. This medicine is for use on the skin only. Do not use VANOS Cream in your eyes, mouth, or vagina. Wash your hands after you use VANOS Cream. Do not use VANOS Cream for longer than 2 weeks in a row. Talk to your doctor if your skin does not get better after 2 weeks of treatment with VANOS Cream. Do not bandage or cover the skin treated with VANOS Cream unless your doctor tells you to. What are the possible side effects with VANOS Cream? VANOS Cream may cause side effects, including: Symptoms of a disorder where the adrenal gland does not make enough of certain hormones (adrenal insufficiency) during treatment or after stopping treatment. Your doctor may do blood tests to check you for adrenal insufficiency while you are using VANOS Cream. Tell your doctor if you have any of these symptoms of adrenal insufficiency: tiredness that worsens and does not go away nausea or vomiting dizziness or fainting muscle weakness irritability and depression loss of appetite weight loss Cushing’s syndrome, when the body is exposed to too much of the hormone cortisol. Your doctor may do tests to check for this. Symptoms can include: weight gain, especially around your upper back and midsection slow healing of cuts, insect bites, and infections tiredness and muscle weakness depression, anxiety, and irritability roundness of your face (moon face) new or worsening high blood pressure The most common side effect of VANOS Cream is burning of your skin treated with VANOS Cream. Talk to your doctor about any side effect that bothers you or that does not go away. These are not all the side effects with VANOS Cream. Ask your doctor or pharmacist for more information. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. You may also report side effects to Valeant Pharmaceuticals North America LLC at 1-800-321-4576. How should I store VANOS Cream? Store VANOS Cream at room temperature, between 59° to 86°F (15° to 30°C). Keep the tube tightly closed. Keep VANOS Cream and all medicines out of reach of children. General information about VANOS Cream Medicines are sometimes prescribed for purposes other than those listed in the Patient Information leaflet. Do not use VANOS Cream for a condition for which it was not prescribed. Do not give VANOS Cream to other people, even if they have the same symptoms you have. It may harm them. This Patient Information leaflet summarizes the most important information about VANOS Cream. If you would like more information, talk with your doctor. You can also ask your pharmacist or doctor for information about VANOS Cream that is written for healthcare professionals. What are the ingredients in VANOS Cream? Active ingredient: fluocinonide 0.1% Inactive ingredients: anhydrous citric acid USP, carbopol 980 NF, diisopropanolamine, dimethyl isosorbide, glyceryl monostearate NF, glyceryl stearate (and) PEG-100 stearate, propylene glycol USP, and purified water USP. This Patient Information has been approved by the U.S. Food and Drug Administration. Manufactured for: Valeant Pharmaceuticals North America LLC Bridgewater, NJ 08807 USA By: Valeant Pharmaceuticals International, Inc. Laval, Quebec H7L 4A8, Canada U.S. Patent Numbers 6,765,001; 7,217,422; 7,220,424; 7,771,733; 7,794,738 and 8,232,264 Vanos is a trademark of Valeant Pharmaceuticals International, Inc. or its affiliates. ©Valeant Pharmaceuticals North America LLC Rev. 05/2017 9481801
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES Two adequate and well-controlled efficacy and safety studies of VANOS Cream have been completed, one in adult subjects with plaque-type psoriasis (Table 2), and one in adult subjects with atopic dermatitis (Table 3). In each of these studies, subjects with between 2% and 10% body surface area involvement at baseline treated all affected areas either once daily or twice daily with VANOS Cream for 14 consecutive days. The primary measure of efficacy was the proportion of subjects whose condition was cleared or almost cleared at the end of treatment. The results of these studies are presented in the tables below as percent and number of patients achieving treatment success at Week 2. Table 2: Plaque-type Psoriasis in Adults VANOS Cream, once daily (n=107) Vehicle, once daily (n=54) VANOS Cream, twice daily (n=107) Vehicle, twice daily (n=55) Subjects cleared 0 (0) 0 (0) 6 (6%) 0 (0) Subjects achieving treatment success Cleared or almost cleared 19 (18%) 4 (7%) 33 (31%) 3 (5%) Table 3: Atopic Dermatitis in Adults VANOS Cream, once daily (n=109) Vehicle, once daily (n=50) VANOS Cream, twice daily (n=102) Vehicle, twice daily (n=52) Subjects cleared 11 (10%) 0 (0) 17 (17%) 0 (0) Subjects achieving treatment success Cleared or almost cleared 64 (59%) 6 (12%) 58 (57%) 10 (19%) No efficacy studies have been conducted to compare VANOS (fluocinonide) Cream, 0.1% with any other topical corticosteroid product, including fluocinonide cream 0.05%.
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use Clinical studies of VANOS Cream did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Nursing mothers
Information about excretion of the drug in human milk and effects on the nursing infant, including pertinent adverse effects observed in animal offspring.8.3 Nursing Mothers Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in breast milk. Nevertheless, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use Safety and efficacy of VANOS Cream in pediatric patients younger than 12 years of age have not been established; therefore, use in pediatric patients younger than 12 years of age is not recommended. HPA-axis suppression was studied in four sequential cohorts of pediatric patients with atopic dermatitis covering at least 20% of the body surface area (BSA), treated once daily or twice daily with VANOS Cream. The first cohort of 31 patients (mean 36.3% BSA) 12 to <18 years old; the second cohort included 31 patients (mean 39.0% BSA) 6 to <12 years old; the third cohort included 30 patients (mean 34.6% BSA) 2 to <6 years old; the fourth cohort included 31 patients (mean 40.0% BSA) 3 months to <2 years old. VANOS Cream caused HPA-axis suppression in 1 patient in the twice-daily group in Cohort 1, 2 patients in the twice-daily group in Cohort 2, and 1 patient in the twice-daily group in Cohort 3. Follow-up testing 14 days after treatment discontinuation, available for all 4 suppressed patients, demonstrated a normally responsive HPA axis. Signs of skin atrophy were present at baseline and severity was not determined, making it difficult to assess local skin safety. Therefore, the safety of VANOS Cream in patients younger than 12 years of age has not been demonstrated [see Warnings and Precautions (5.2) ] . HPA-axis suppression has not been evaluated in patients with psoriasis who are less than 18 years of age. Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of HPA-axis suppression and Cushing’s syndrome when they are treated with topical corticosteroids. They are therefore also at greater risk of adrenal insufficiency during or after withdrawal of treatment. Adverse effects including striae have been reported with inappropriate use of topical corticosteroids in infants and children. HPA-axis suppression, Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in children receiving topical corticosteroids. Manifestations of adrenal suppression in children include low plasma cortisol levels and absence of response to cosyntropin (ACTH 1-24 ) stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Teratogenic Effects: Pregnancy Category C There are no adequate and well-controlled studies in pregnant women. Therefore, VANOS Cream should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Some corticosteroids have been shown to be teratogenic after dermal application in laboratory animals.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Teratogenic Effects: Pregnancy Category C There are no adequate and well-controlled studies in pregnant women. Therefore, VANOS Cream should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Corticosteroids have been shown to be teratogenic in laboratory animals when administered systemically at relatively low dosage levels. Some corticosteroids have been shown to be teratogenic after dermal application in laboratory animals. 8.3 Nursing Mothers Systemically administered corticosteroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in breast milk. Nevertheless, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. 8.4 Pediatric Use Safety and efficacy of VANOS Cream in pediatric patients younger than 12 years of age have not been established; therefore, use in pediatric patients younger than 12 years of age is not recommended. HPA-axis suppression was studied in four sequential cohorts of pediatric patients with atopic dermatitis covering at least 20% of the body surface area (BSA), treated once daily or twice daily with VANOS Cream. The first cohort of 31 patients (mean 36.3% BSA) 12 to <18 years old; the second cohort included 31 patients (mean 39.0% BSA) 6 to <12 years old; the third cohort included 30 patients (mean 34.6% BSA) 2 to <6 years old; the fourth cohort included 31 patients (mean 40.0% BSA) 3 months to <2 years old. VANOS Cream caused HPA-axis suppression in 1 patient in the twice-daily group in Cohort 1, 2 patients in the twice-daily group in Cohort 2, and 1 patient in the twice-daily group in Cohort 3. Follow-up testing 14 days after treatment discontinuation, available for all 4 suppressed patients, demonstrated a normally responsive HPA axis. Signs of skin atrophy were present at baseline and severity was not determined, making it difficult to assess local skin safety. Therefore, the safety of VANOS Cream in patients younger than 12 years of age has not been demonstrated [see Warnings and Precautions (5.2) ] . HPA-axis suppression has not been evaluated in patients with psoriasis who are less than 18 years of age. Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of HPA-axis suppression and Cushing’s syndrome when they are treated with topical corticosteroids. They are therefore also at greater risk of adrenal insufficiency during or after withdrawal of treatment. Adverse effects including striae have been reported with inappropriate use of topical corticosteroids in infants and children. HPA-axis suppression, Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in children receiving topical corticosteroids. Manifestations of adrenal suppression in children include low plasma cortisol levels and absence of response to cosyntropin (ACTH 1-24 ) stimulation. Manifestations of intracranial hypertension include bulging fontanelles, headaches, and bilateral papilledema. 8.5 Geriatric Use Clinical studies of VANOS Cream did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING VANOS ® (fluocinonide) Cream, 0.1% is white to off-white in color and is supplied in tubes as follows: 30 g NDC 99207-525-30 60 g NDC 99207-525-60 120 g NDC 99207-525-10 Store at controlled room temperature 15° to 30°C (59° to 86°F). Keep the tube tightly closed.
Storage and handling
Information about safe storage and handling of the drug product.Store at controlled room temperature 15° to 30°C (59° to 86°F). Keep the tube tightly closed.
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API