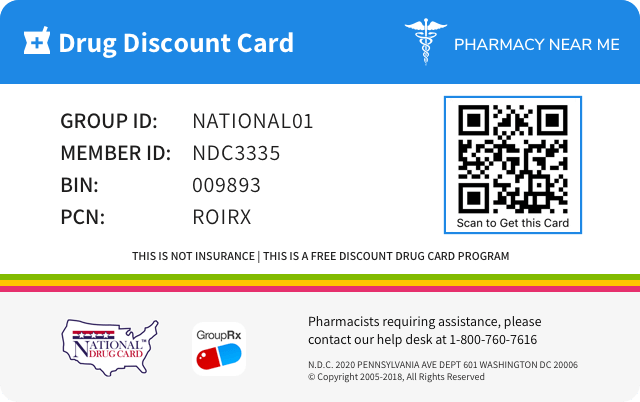
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 0480-1232 | ||||
|---|---|---|---|---|---|
| Drug Name | Risperidone |
||||
| Type | Generic | ||||
| Dosage Form | KIT | ||||
| RxCUI drug identifier | 402010, 402011, 402012, 706822 |
||||
| Application Number | ANDA214068 | ||||
| Labeler Name | Teva Pharmaceuticals, Inc. | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Drug abuse and dependence
Information about whether the drug is a controlled substance, the types of abuse that can occur with the drug, and adverse reactions pertinent to those types of abuse.9 DRUG ABUSE AND DEPENDENCE 9.1 Controlled Substance Risperidone for Extended-Release Injectable Suspension is not a controlled substance. 9.2 Abuse Risperidone for Extended-Release Injectable Suspension has not been systematically studied in animals or humans for its potential for abuse. Because Risperidone for Extended-Release Injectable Suspension is to be administered by health care professionals, the potential for misuse or abuse by patients is low. 9.3 Dependence Risperidone for Extended-Release Injectable Suspension has not been systematically studied in animals or humans for its potential for tolerance or physical dependence.
Overdosage of Risperidone
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE 10.1 Human Experience No cases of overdose were reported in premarketing studies with Risperidone for Extended-Release Injectable Suspension. Because Risperidone for Extended-Release Injectable Suspension is to be administered by health care professionals, the potential for overdosage by patients is low. In premarketing experience with oral risperidone, there were eight reports of acute risperidone overdosage, with estimated doses ranging from 20 to 300 mg and no fatalities. In general, reported signs and symptoms were those resulting from an exaggeration of the drug’s known pharmacological effects, i.e., drowsiness and sedation, tachycardia and hypotension, and extrapyramidal symptoms. One case, involving an estimated overdose of 240 mg, was associated with hyponatremia, hypokalemia, prolonged QT, and widened QRS. Another case, involving an estimated overdose of 36 mg, was associated with a seizure. Postmarketing experience with oral risperidone includes reports of acute overdose, with estimated doses of up to 360 mg. In general, the most frequently reported signs and symptoms are those resulting from an exaggeration of the drug’s known pharmacological effects, i.e., drowsiness, sedation, tachycardia, hypotension, and extrapyramidal symptoms. Other adverse reactions reported since market introduction related to oral risperidone overdose include prolonged QT interval and convulsions. Torsade de pointes has been reported in association with combined overdose of oral risperidone and paroxetine. 10.2 Management of Overdosage In case of acute overdosage, establish and maintain an airway and ensure adequate oxygenation and ventilation. Cardiovascular monitoring should commence immediately and should include continuous electrocardiographic monitoring to detect possible arrhythmias. If antiarrhythmic therapy is administered, disopyramide, procainamide, and quinidine carry a theoretical hazard of QT prolonging effects that might be additive to those of risperidone. Similarly, it is reasonable to expect that the alpha-blocking properties of bretylium might be additive to those of risperidone, resulting in problematic hypotension. There is no specific antidote to risperidone. Therefore, appropriate supportive measures should be instituted. The possibility of multiple drug involvement should be considered. Hypotension and circulatory collapse should be treated with appropriate measures, such as intravenous fluids and/or sympathomimetic agents (epinephrine and dopamine should not be used, since beta stimulation may worsen hypotension in the setting of risperidone-induced alpha blockade). In cases of severe extrapyramidal symptoms, anticholinergic medication should be administered. Close medical supervision and monitoring should continue until the patient recovers.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS The following are discussed in more detail in other sections of the labeling: Increased mortality in elderly patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions ( 5.1 )] Cerebrovascular adverse events, including stroke, in elderly patients with dementia-related psychosis [see Warnings and Precautions ( 5.2 )] Neuroleptic malignant syndrome [see Warnings and Precautions ( 5.3 )] Tardive dyskinesia [see Warnings and Precautions ( 5.4 )] Metabolic changes [see Warnings and Precautions ( 5.5 )] Hyperprolactinemia [see Warnings and Precautions ( 5.6 )] Orthostatic hypotension [see Warnings and Precautions (5.7 ) ] Falls [see Warnings and Precautions ( 5.8 )] Leukopenia/Neutropenia and Agranulocytosis [see Warnings and Precautions ( 5.9 )] Potential for cognitive and motor impairment [see Warnings and Precautions ( 5.10) ] Seizures [see Warnings and Precautions (5.11 )] Dysphagia [see Warnings and Precautions ( 5.12 )] Priapism [see Warnings and Precautions ( 5.13 )] Disruption of body temperature regulation [see Warnings and Precautions ( 5.14 )] Avoidance of inadvertent injection into a blood vessel [see Warnings and Precautions ( 5.15 )] Osteodystrophy and tumors in animals [see Warnings and Precautions ( 5.16 ) ] The most common adverse reactions in clinical trials in patients with schizophrenia (≥ 5%) were: headache, parkinsonism, dizziness, akathisia, fatigue, constipation, dyspepsia, sedation, weight increased, pain in extremity, and dry mouth. The most common adverse reactions in the double-blind, placebo-controlled periods of the bipolar disorder trials were weight increased (5% in the monotherapy trial) and tremor and parkinsonism (≥ 10% in the adjunctive treatment trial). The most common adverse reactions that were associated with discontinuation from the 12-week double-blind, placebo-controlled trial in patients with schizophrenia (causing discontinuation in ≥1% of patients) were agitation, depression, anxiety, and akathisia. Adverse reactions that were associated with discontinuation from the double-blind, placebo-controlled periods of the bipolar disorder trials were hyperglycemia (one patient in the monotherapy trial) and hypokinesia and tardive dyskinesia (one patient each in the adjunctive treatment trial). The data described in this section are derived from a clinical trial database consisting of 2392 patients exposed to one or more doses of Risperidone for Extended-Release Injectable Suspension for the treatment of schizophrenia. Of these 2392 patients, 332 were patients who received Risperidone for Extended-Release Injectable Suspension while participating in a 12-week double-blind, placebo-controlled trial. Two hundred two (202) of the 332 were schizophrenia patients who received 25 mg or 50 mg Risperidone for Extended-Release Injectable Suspension. The conditions and duration of treatment with Risperidone for Extended-Release Injectable Suspension in the other clinical trials varied greatly and included (in overlapping categories) double-blind, fixed- and flexible- dose, placebo- or active-controlled studies and open-label phases of studies, inpatients and outpatients, and short-term (up to 12 weeks) and longer-term (up to 4 years) exposures. Safety was assessed by collecting adverse events and performing physical examinations, vital signs, body weights, laboratory analyses, and ECGs. In addition to the studies in patients with schizophrenia, safety data are presented from a trial assessing the efficacy and safety of Risperidone for Extended-Release Injectable Suspension when administered as monotherapy for maintenance treatment in patients with bipolar I disorder. The subjects in this multi-center, double-blind, placebo-controlled study were adult patients who met DSM-IV criteria for Bipolar Disorder Type I and who were stable on risperidone (oral or long-acting injection), were stable on other antipsychotics or mood stabilizers, or were experiencing an acute episode. After a 3-week period of treatment with open-label oral risperidone (N=440), subjects who demonstrated an initial response to oral risperidone in this period and those who were stable on risperidone (oral or long-acting injection) at study entry entered into a 26-week stabilization period of open-label Risperidone for Extended-Release Injectable Suspension (N=501). Subjects who demonstrated a maintained response during this period were then randomized into a 24-month double-blind, placebo-controlled period in which they received Risperidone for Extended-Release Injectable Suspension (N=154) or placebo (N=149) as monotherapy. Subjects who relapsed or who completed the double-blind period could choose to enter an 8-week open-label Risperidone for Extended-Release Injectable Suspension extension period (N=160). Safety data are also presented from a trial assessing the efficacy and safety of Risperidone for Extended-Release Injectable Suspension when administered as adjunctive maintenance treatment in patients with bipolar disorder. The subjects in this multi-center, double-blind, placebo-controlled study were adult patients who met DSM-IV criteria for Bipolar Disorder Type I or Type II and who experienced at least 4 episodes of mood disorder requiring psychiatric/clinical intervention in the previous 12 months, including at least 2 episodes in the 6 months prior to the start of the study. At the start of this study, all patients (N=275) entered into a 16-week open-label treatment phase in which they received Risperidone for Extended-Release Injectable Suspension in addition to continuing their treatment as usual, which consisted of various mood stabilizers (primarily lithium and valproate), antidepressants, and/or anxiolytics. Patients who reached remission at the end of this 16-week open-label treatment phase (N=139) were then randomized into a 52-week double-blind, placebo-controlled phase in which they received Risperidone for Extended-Release Injectable Suspension (N=72) or placebo (n=67) as adjunctive treatment in addition to continuing their treatment as usual. Patients who did not reach remission at the end of the 16-week open-label treatment phase could choose to continue to receive Risperidone for Extended-Release Injectable Suspension as adjunctive therapy in an open-label manner, in addition to continuing their treatment as usual, for up to an additional 36 weeks as clinically indicated for a total period of up to 52 weeks; these patients (N=70) were also included in the evaluation of safety. Adverse events during exposure to study treatment were obtained by general inquiry and recorded by clinical investigators using their own terminology. Consequently, to provide a meaningful estimate of the proportion of individuals experiencing adverse events, events were grouped in standardized categories using MedDRA terminology. Throughout this section, adverse reactions are reported. Adverse reactions are adverse events that were considered to be reasonably associated with the use of Risperidone for Extended-Release Injectable Suspension (adverse drug reactions) based on the comprehensive assessment of the available adverse event information. A causal association for Risperidone for Extended-Release Injectable Suspension often cannot be reliably established in individual cases. Further, because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. The majority of all adverse reactions were mild to moderate in severity. The most common adverse reactions in clinical trials in patients with schizophrenia (≥ 5%) were headache, parkinsonism, dizziness, akathisia, fatigue, constipation, dyspepsia, sedation, weight increased, pain in extremity, and dry mouth. The most common adverse reactions in clinical trials in patients with bipolar disorder were weight increased (5% in monotherapy trial) and tremor and parkinsonism (≥ 10% in adjunctive therapy trial). ( 6 ) The most common adverse reactions that were associated with discontinuation from clinical trials in patients with schizophrenia were agitation, depression, anxiety, and akathisia. Adverse reactions that were associated with discontinuation from bipolar disorder trials were hyperglycemia (one subject monotherapy trial) and hypokinesia and tardive dyskinesia (one subject each in adjunctive therapy trial). (6 ) To report SUSPECTED ADVERSE REACTIONS, contact Teva at 1-888-838-2872 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. 6.1 Clinical Trials Experience Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials - Schizophrenia Table 4 lists the adverse reactions reported in 2% or more of Risperidone for Extended-Release Injectable Suspension-treated patients with schizophrenia in one 12-week double-blind, placebo-controlled trial. Table 4. Adverse Reactions in ≥2% of Risperidone for Extended-Release Injectable Suspension-Treated Patients with Schizophrenia in a 12-Week Double-Blind, Placebo-Controlled Trial Percentage of Patients Reporting Event Risperidone for Extended-Release Injectable Suspension Placebo System/Organ Class 25 mg 50 mg Adverse Reaction (N=99) (N=103) (N=98) Eye disorders Vision blurred 2 3 0 Gastrointestinal disorders Constipation Dry mouth Dyspepsia Nausea Toothache Salivary hypersecretion 5 0 6 3 1 4 7 7 6 4 3 1 1 1 0 5 0 0 General disorders and administration site conditions Fatigue* Edema peripheral Pain Pyrexia 3 2 4 2 9 3 1 1 0 1 0 0 Infections and infestations Upper respiratory tract infection 2 0 1 Investigations Weight increased Weight decreased 5 4 4 1 2 1 Musculoskeletal and connective tissue disorders Pain in extremity 6 2 1 Nervous system disorders Headache Parkinsonism* Dizziness Akathisia* Sedation* Tremor Syncope Hypoesthesia 15 8 7 4 5 0 2 2 21 15 11 11 6 3 1 0 12 9 6 6 3 0 0 0 Respiratory, thoracic and mediastinal disorders Cough Sinus congestion 4 2 2 0 3 0 Skin and subcutaneous tissue disorders Acne Dry skin 2 2 2 0 0 0 * Fatigue includes fatigue and asthenia. Parkinsonism includes extrapyramidal disorder, musculoskeletal stiffness, muscle rigidity, and bradykinesia. Akathisia includes akathisia and restlessness. Sedation includes sedation and somnolence. Commonly-Observed Adverse Reactions in Double-Blind, Placebo-Controlled Clinical Trials – Bipolar Disorder Table 5 lists the treatment-emergent adverse reactions reported in 2% or more of Risperidone for Extended-Release Injectable Suspension-treated patients in the 24-month double-blind, placebo-controlled treatment period of the trial assessing the efficacy and safety of Risperidone for Extended-Release Injectable Suspension when administered as monotherapy for maintenance treatment in patients with Bipolar I Disorder. Table 5. Adverse Reactions in ≥2% of Patients with Bipolar I Disorder Treated with Risperidone for Extended-Release Injectable Suspension as Monotherapy in a 24-Month Double-Blind, Placebo-Controlled Trial Percentage of Patients Reporting Event System/Organ Class Risperidone for Extended-Release Injectable Suspension Placebo Adverse Reaction (N=154) (N=149) Investigations Weight increased 5 1 Nervous system disorders Dizziness 3 1 Vascular disorders Hypertension 3 1 Table 6 lists the treatment-emergent adverse reactions reported in 4% or more of patients in the 52-week double-blind, placebo-controlled treatment phase of a trial assessing the efficacy and safety of Risperidone for Extended-Release Injectable Suspension when administered as adjunctive maintenance treatment in patients with bipolar disorder. Table 6. Adverse Reactions in ≥ 4% of Patients with Bipolar Disorder Treated with Risperidone for Extended-Release Injectable Suspension as Adjunctive Therapy in a 52-Week Double-Blind, Placebo-Controlled Trial Percentage of Patients Reporting Event Risperidone for Extended-Release Injectable Suspension + Placebo + System/Organ Class Treatment as Usual a Treatment as Usual a Adverse Reaction (N=72) (N=67) General disorders and administration site conditions Gait abnormal 4 0 Infections and infestations Upper respiratory tract infection 6 3 Investigations Weight increased 7 1 Metabolism and nutrition disorders Decreased appetite 6 1 Increased appetite 4 0 Musculoskeletal and connective tissue disorders Arthralgia 4 3 Nervous system disorders Tremor 24 16 Parkinsonism b 15 6 Dyskinesia b 6 3 Sedation c 7 1 Disturbance in attention 4 0 Reproductive system and breast disorders Amenorrhea 4 1 Respiratory, thoracic and mediastinal disorders Cough 4 1 a Patients received double-blind Risperidone for Extended-Release Injectable Suspension or placebo in addition to continuing their treatment as usual, which included mood stabilizers, antidepressants, and/or anxiolytics. b Parkinsonism includes muscle rigidity, hypokinesia, cogwheel rigidity, and bradykinesia. Dyskinesia includes muscle twitching and dyskinesia. c Sedation includes sedation and somnolence. Other Adverse Reactions Observed During the Clinical Trial Evaluation of Risperidone The following additional adverse reactions occurred in < 2% of the Risperidone for Extended-Release Injectable Suspension-treated patients in the above schizophrenia double-blind, placebo-controlled trial dataset, in < 2% of the Risperidone for Extended-Release Injectable Suspension-treated patients in the above double-blind, placebo-controlled period of the monotherapy bipolar disorder trial dataset, or in < 4% of the Risperidone for Extended-Release Injectable Suspension-treated patients in the above double-blind, placebo-controlled period of the adjunctive treatment bipolar disorder trial dataset. The following also includes additional adverse reactions reported at any frequency in Risperidone for Extended-Release Injectable Suspension-treated patients who participated in the open-label phases of the above bipolar disorder studies and in other studies, including double-blind, active controlled and open-label studies in schizophrenia and bipolar disorder. Blood and lymphatic system disorders: anemia, neutropenia Cardiac disorders: tachycardia, atrioventricular block first degree, palpitations, sinus bradycardia, bundle branch block left, bradycardia, sinus tachycardia, bundle branch block right Ear and labyrinth disorders: ear pain, vertigo Endocrine disorders: hyperprolactinemia Eye disorders: conjunctivitis, visual acuity reduced Gastrointestinal disorders: diarrhea, vomiting, abdominal pain upper, abdominal pain, stomach discomfort, gastritis General disorders and administration site conditions: injection site pain, chest discomfort, chest pain, influenza like illness, sluggishness, malaise, induration, injection site induration, injection site swelling, injection site reaction, face edema Immune system disorders: hypersensitivity Infections and infestations: nasopharyngitis, influenza, bronchitis, urinary tract infection, rhinitis, respiratory tract infection, ear infection, pneumonia, lower respiratory tract infection, pharyngitis, sinusitis, viral infection, infection, localized infection, cystitis, gastroenteritis, subcutaneous abscess Injury and poisoning: fall, procedural pain Investigations: blood prolactin increased, alanine aminotransferase increased, electrocardiogram abnormal, gamma-glutamyl transferase increased, blood glucose increased, hepatic enzyme increased, aspartate aminotransferase increased, electrocardiogram QT prolonged, glucose urine present Metabolism and nutritional disorders: anorexia, hyperglycemia Musculoskeletal, connective tissue and bone disorders: posture abnormal, myalgia, back pain, buttock pain, muscular weakness, neck pain, musculoskeletal chest pain Nervous system disorders: coordination abnormal, dystonia, tardive dyskinesia, drooling, paresthesia, dizziness postural, convulsion, akinesia, hypokinesia, dysarthria Psychiatric disorders: insomnia, agitation, anxiety, sleep disorder, depression, initial insomnia, libido decreased, nervousness Renal and urinary disorders: urinary incontinence Reproductive system and breast disorders: galactorrhea, oligomenorrhea, erectile dysfunction, sexual dysfunction, ejaculation disorder, gynecomastia, breast discomfort, menstruation irregular, menstruation delayed, menstrual disorder, ejaculation delayed Respiratory, thoracic and mediastinal disorders: nasal congestion, pharyngolaryngeal pain, dyspnea, rhinorrhea Skin and subcutaneous tissue disorders: rash, eczema, pruritus generalized, pruritus Vascular disorders: hypotension, orthostatic hypotension Additional Adverse Reactions Reported with Oral Risperidone The following is a list of additional adverse reactions that have been reported during the clinical trial evaluation of oral risperidone, regardless of frequency of occurrence: Blood and Lymphatic Disorders: granulocytopenia Cardiac Disorders: atrioventricular block Ear and Labyrinth Disorders: tinnitus Eye Disorders: ocular hyperemia, eye discharge, eye rolling, eyelid edema, eye swelling, eyelid margin crusting, dry eye, lacrimation increased, photophobia, glaucoma Gastrointestinal Disorders: abdominal pain upper, dysphagia, fecaloma, abdominal discomfort, fecal incontinence, lip swelling, cheilitis, aptyalism General Disorders: thirst, feeling abnormal, gait disturbance, pitting edema, edema, chills, discomfort, generalized edema, drug withdrawal syndrome, peripheral coldness Immune System Disorders: drug hypersensitivity Infections and Infestations: tonsillitis, eye infection, cellulitis, otitis media, onychomycosis, acarodermatitis, bronchopneumonia, respiratory tract infection, tracheobronchitis, otitis media chronic Investigations: body temperature increased, heart rate increased, eosinophil count increased, white blood cell count decreased, hemoglobin decreased, blood creatine phosphokinase increased, hematocrit decreased, body temperature decreased, blood pressure decreased, transaminases increased Metabolism and Nutrition Disorders: polydipsia Musculoskeletal, Connective Tissue, and Bone Disorders: joint swelling, joint stiffness, rhabdomyolysis, torticollis Nervous System Disorders: hypertonia, balance disorder, dysarthria, unresponsive to stimuli, depressed level of consciousness, movement disorder, hypokinesia, parkinsonian rest tremor, transient ischemic attack, cerebrovascular accident, masked facies, speech disorder, loss of consciousness, muscle contractions involuntary, akinesia, cerebral ischemia, cerebrovascular disorder, neuroleptic malignant syndrome, diabetic coma, head titubation Psychiatric Disorders: blunted affect, confusional state, middle insomnia, listlessness, anorgasmia Renal and Urinary Disorders: enuresis, dysuria, pollakiuria Reproductive System and Breast Disorders: vaginal discharge, retrograde ejaculation, ejaculation disorder, ejaculation failure, breast enlargement Respiratory, Thoracic, and Mediastinal Disorders: epistaxis, wheezing, pneumonia aspiration, dysphonia, productive cough, pulmonary congestion, respiratory tract congestion, rales, respiratory disorder, hyperventilation, nasal edema Skin and Subcutaneous Tissue Disorders: erythema, skin discoloration, skin lesion, skin disorder, rash erythematous, rash papular, hyperkeratosis, dandruff, seborrheic dermatitis, rash generalized, rash maculopapular Vascular Disorders: flushing Discontinuations Due to Adverse Reactions Schizophrenia Approximately 11% (22/202) of Risperidone for Extended-Release Injectable Suspension-treated patients in the 12-week double-blind, placebo-controlled schizophrenia trial discontinued treatment due to an adverse event, compared with 13% (13/98) who received placebo. The adverse reactions associated with discontinuation in two or more Risperidone for Extended-Release Injectable Suspension-treated patients were: agitation (3%), depression (2%), anxiety (1%), and akathisia (1%). Bipolar Disorder In the 24-month double-blind, placebo-controlled treatment period of the trial assessing the efficacy and safety of Risperidone for Extended-Release Injectable Suspension when administered as monotherapy for maintenance treatment in patients with bipolar I disorder, 1 (0.6%) of 154 Risperidone for Extended-Release Injectable Suspension-treated patients discontinued due to an adverse reaction (hyperglycemia). In the 52-week double-blind phase of the placebo-controlled trial in which Risperidone for Extended-Release Injectable Suspension was administered as adjunctive therapy to patients with bipolar disorder in addition to continuing with their treatment as usual, approximately 4% (3/72) of Risperidone for Extended-Release Injectable Suspension-treated patients discontinued treatment due to an adverse event, compared with 1.5% (1/67) of placebo-treated patients. Adverse reactions associated with discontinuation in Risperidone for Extended-Release Injectable Suspension-treated patients were: hypokinesia (one patient) and tardive dyskinesia (one patient). Dose Dependency of Adverse Reactions in Clinical Trials Extrapyramidal Symptoms Two methods were used to measure extrapyramidal symptoms (EPS) in the 12-week double-blind, placebo-controlled trial comparing three doses of Risperidone for Extended-Release Injectable Suspension (25 mg, 50 mg, and 75 mg) with placebo in patients with schizophrenia, including: (1) the incidence of spontaneous reports of EPS symptoms; and (2) the change from baseline to endpoint on the total score (sum of the subscale scores for parkinsonism, dystonia, and dyskinesia) of the Extrapyramidal Symptom Rating Scale (ESRS). As shown in Table 1, the overall incidence of EPS-related adverse reactions (akathisia, dystonia, parkinsonism, and tremor) in patients treated with 25 mg Risperidone for Extended-Release Injectable Suspension was comparable to that of patients treated with placebo; the incidence of EPS-related adverse reactions was higher in patients treated with 50 mg Risperidone for Extended-Release Injectable Suspension. The median change from baseline to endpoint in total ESRS score showed no worsening in patients treated with Risperidone for Extended-Release Injectable Suspension compared with patients treated with placebo: 0 (placebo group); -1 (25 mg group, significantly less than the placebo group); and 0 (50 mg group). Dystonia Class Effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups. Changes in ECG The electrocardiograms of 202 schizophrenic patients treated with 25 mg or 50 mg Risperidone for Extended-Release Injectable Suspension and 98 schizophrenic patients treated with placebo in the 12-week double-blind, placebo-controlled trial were evaluated. Compared with placebo, there were no statistically significant differences in QTc intervals (using Fridericia’s and linear correction factors) during treatment with Risperidone for Extended-Release Injectable Suspension. The electrocardiograms of 227 patients with Bipolar I Disorder were evaluated in the 24-month double-blind, placebo-controlled period. There were no clinically relevant differences in QTc intervals (using Fridericia’s and linear correction factors) during treatment with Risperidone for Extended-Release Injectable Suspension compared to placebo. The electrocardiograms of 85 patients with bipolar disorder were evaluated in the 52-week double-blind, placebo-controlled trial. There were no statistically significant differences in QTc intervals (using Fridericia’s and linear correction factors) during treatment with Risperidone for Extended-Release Injectable Suspension 25 mg, 37.5 mg, or 50 mg when administered as adjunctive treatment in addition to continuing treatment as usual compared to placebo. Pain Assessment and Local Injection Site Reactions The mean intensity of injection pain reported by patients with schizophrenia using a visual analog scale (0 = no pain to 100 = unbearably painful) decreased in all treatment groups from the first to the last injection (placebo: 16.7 to 12.6; 25 mg: 12.0 to 9.0; 50 mg: 18.2 to 11.8). After the sixth injection (Week 10), investigator ratings indicated that 1% of patients treated with 25 mg or 50 mg Risperidone for Extended-Release Injectable Suspension experienced redness, swelling, or induration at the injection site. In a separate study to observe local-site tolerability in which Risperidone for Extended-Release Injectable Suspension was administered into the deltoid muscle every 2 weeks over a period of 8 weeks, no patient discontinued treatment due to local injection site pain or reaction. Clinician ratings indicated that only mild redness, swelling, or induration at the injection site was observed in subjects treated with 37.5 mg or 50 mg Risperidone for Extended-Release Injectable Suspension at 2 hours after deltoid injection. All ratings returned to baseline at the predose assessment of the next injection 2 weeks later. No moderate or severe reactions were observed in any subject. 6.2 Postmarketing Experience The following adverse reactions have been identified during postapproval use of risperidone; because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency: agranulocytosis, alopecia, anaphylactic reaction, angioedema, atrial fibrillation, blood cholesterol increased, blood triglycerides increased, catatonia, diabetes mellitus, diabetic ketoacidosis in patients with impaired glucose metabolism, drug withdrawal syndrome neonatal, dysgeusia, hypoglycemia, hypothermia, ileus, inappropriate antidiuretic hormone secretion, intestinal obstruction, jaundice, mania, pancreatitis, priapism, QT prolongation, sleep apnea syndrome, somnambulism, Stevens-Johnson syndrome and toxic epidermal necrolysis (SJS/TEN), thrombocytopenia, thrombotic thrombocytopenic purpura, urinary retention, and water intoxication. In addition, the following adverse reactions have been observed during postapproval use of Risperidone for Extended-Release Injectable Suspension: cerebrovascular disorders, including cerebrovascular accidents, and diabetes mellitus aggravated. Retinal artery occlusion after injection of Risperidone for Extended-Release Injectable Suspension has been reported during postmarketing surveillance. This has been reported in the presence of abnormal arteriovenous anastomosis. Serious injection site reactions including abscess, cellulitis, cyst, hematoma, necrosis, nodule, and ulcer have been reported with Risperidone for Extended-Release Injectable Suspension during postmarketing surveillance. Isolated cases required surgical intervention. Very rarely, cases of anaphylactic reaction after injection with Risperidone for Extended-Release Injectable Suspension have been reported during postmarketing experience in patients who have previously tolerated oral risperidone. Postmarketing cases of extrapyramidal symptoms (dystonia and dyskinesia) have been reported in patients concomitantly taking methylphenidate and risperidone when there was an increase or decrease in dosage, initiation, or discontinuation of either or both medications.
Risperidone Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS The interactions of Risperidone for Extended-Release Injectable Suspension with coadministration of other drugs have not been systematically evaluated. The drug interaction data provided in this section is based on studies with oral risperidone. Due to CNS effects, use caution when administering with other centrally-acting drugs. Avoid alcohol. ( 7.1 ) Due to hypotensive effects, hypotensive effects of other drugs with this potential may be enhanced. ( 7.2 ) Effects of levodopa and dopamine agonists may be antagonized. ( 7.3 ) Cimetidine and ranitidine increase the bioavailability of risperidone. ( 7.5 ) Clozapine may decrease clearance of risperidone. ( 7.6 ) Fluoxetine and paroxetine increase plasma concentrations of risperidone. ( 7.11 ) Carbamazepine and other enzyme inducers decrease plasma concentrations of risperidone. ( 7.12 ) 7.1 Centrally-Acting Drugs and Alcohol Given the primary CNS effects of risperidone, caution should be used when Risperidone for Extended-Release Injectable Suspension is administered in combination with other centrally-acting drugs or alcohol. 7.2 Drugs with Hypotensive Effects Because of its potential for inducing hypotension, Risperidone for Extended-Release Injectable Suspension may enhance the hypotensive effects of other therapeutic agents with this potential. 7.3 Levodopa and Dopamine Agonists Risperidone for Extended-Release Injectable Suspension may antagonize the effects of levodopa and dopamine agonists. 7.4 Amitriptyline Amitriptyline did not affect the pharmacokinetics of risperidone or of risperidone and 9-hydroxyrisperidone combined following concomitant administration with oral risperidone. 7.5 Cimetidine and Ranitidine Cimetidine and ranitidine increased the bioavailability of oral risperidone by 64% and 26%, respectively. However, cimetidine did not affect the AUC of risperidone and 9-hydroxyrisperidone combined, whereas ranitidine increased the AUC of risperidone and 9-hydroxyrisperidone combined by 20%. 7.6 Methylphenidate Concomitant use with methylphenidate, when there is change in dosage of either medication, may increase the risk of extrapyramidal symptoms (EPS). Monitor for symptoms of EPS with concomitant use of Risperidone for Extended-Release Injectable Suspension and methylphenidate [see Adverse Reactions (6.2)] . 7.7 Clozapine Chronic administration of clozapine with risperidone may decrease the clearance of risperidone. 7.8 Lithium Repeated doses of oral risperidone (3 mg twice daily) did not affect the exposure (AUC) or peak plasma concentrations (C max ) of lithium (N=13). 7.9 Valproate Repeated doses of oral risperidone (4 mg once daily) did not affect the pre-dose or average plasma concentrations and exposure (AUC) of valproate (1000 mg/day in three divided doses) compared to placebo (N=21). However, there was a 20% increase in valproate peak plasma concentration (C max ) after concomitant administration of oral risperidone. 7.10 Digoxin Oral risperidone (0.25 mg twice daily) did not show a clinically relevant effect on the pharmacokinetics of digoxin. 7.11 Topiramate Oral risperidone administered at doses from 1 to 6 mg/day concomitantly with topiramate 400 mg/day resulted in a 23% decrease in risperidone C max and a 33% decrease in risperidone AUC 0-12 hour at steady state. Minimal reductions in the exposure to risperidone and 9-hydroxyrisperidone combined, and no change for 9-hydroxyrisperidone were observed. This interaction is unlikely to be of clinical significance. There was no clinically relevant effect of oral risperidone on the pharmacokinetics of topiramate. 7.12 Drugs That Inhibit CYP 2D6 and Other CYP Isozymes Risperidone is metabolized to 9-hydroxyrisperidone by CYP 2D6, an enzyme that is polymorphic in the population and that can be inhibited by a variety of psychotropic and other drugs [see Clinical Pharmacology ( 12.3 )] . Drug interactions that reduce the metabolism of risperidone to 9-hydroxyrisperidone would increase the plasma concentrations of risperidone and lower the concentrations of 9-hydroxyrisperidone. Analysis of clinical studies involving a modest number of poor metabolizers (n≅70 patients) does not suggest that poor and extensive metabolizers have different rates of adverse effects. No comparison of effectiveness in the two groups has been made. In vitro studies showed that drugs metabolized by other CYP isozymes, including 1A1, 1A2, 2C9, 2C19, and 3A4, are only weak inhibitors of risperidone metabolism. Fluoxetine and Paroxetine Fluoxetine (20 mg once daily) and paroxetine (20 mg once daily), CYP 2D6 inhibitors, have been shown to increase the plasma concentration of risperidone 2.5 to 2.8 fold and 3 to 9 fold respectively. Fluoxetine did not affect the plasma concentration of 9-hydroxyrisperidone. Paroxetine lowered the concentration of 9-hydroxyrisperidone by about 10%. When either concomitant fluoxetine or paroxetine is initiated or discontinued, the physician should re-evaluate the dose of Risperidone for Extended-Release Injectable Suspension. When initiation of fluoxetine or paroxetine is considered, patients may be placed on a lower dose of Risperidone for Extended-Release Injectable Suspension between 2 to 4 weeks before the planned start of fluoxetine or paroxetine therapy to adjust for the expected increase in plasma concentrations of risperidone. When fluoxetine or paroxetine is initiated in patients receiving the recommended dose of 25 mg Risperidone for Extended-Release Injectable Suspension, it is recommended to continue treatment with the 25 mg dose unless clinical judgment necessitates lowering the Risperidone for Extended-Release Injectable Suspension dose to 12.5 mg or necessitates interruption of Risperidone for Extended-Release Injectable Suspension treatment. When Risperidone for Extended-Release Injectable Suspension is initiated in patients already receiving fluoxetine or paroxetine, a starting dose of 12.5 mg can be considered. The efficacy of the 12.5 mg dose has not been investigated in clinical trials [see also Dosage and Administration ( 2.5 )] . The effects of discontinuation of concomitant fluoxetine or paroxetine therapy on the pharmacokinetics of risperidone and 9-hydroxyrisperidone have not been studied. Erythromycin There were no significant interactions between oral risperidone and erythromycin. 7.13 Carbamazepine and Other CYP 3A4 Enzyme Inducers Carbamazepine coadministration with oral risperidone decreased the steady-state plasma concentrations of risperidone and 9-hydroxyrisperidone by about 50%. Plasma concentrations of carbamazepine did not appear to be affected. Coadministration of other known CYP 3A4 enzyme inducers (e.g., phenytoin, rifampin, and phenobarbital) with risperidone may cause similar decreases in the combined plasma concentrations of risperidone and 9-hydroxyrisperidone, which could lead to decreased efficacy of Risperidone for Extended-Release Injectable Suspension treatment. At the initiation of therapy with carbamazepine or other known hepatic enzyme inducers, patients should be closely monitored during the first 4 to 8 weeks, since the dose of Risperidone for Extended-Release Injectable Suspension may need to be adjusted. A dose increase, or additional oral risperidone, may need to be considered. On discontinuation of carbamazepine or other CYP 3A4 hepatic enzyme inducers, the dosage of Risperidone for Extended-Release Injectable Suspension should be re-evaluated and, if necessary, decreased. Patients may be placed on a lower dose of Risperidone for Extended-Release Injectable Suspension between 2 to 4 weeks before the planned discontinuation of carbamazepine or other CYP 3A4 enzyme inducers to adjust for the expected increase in plasma concentrations of risperidone plus 9-hydroxyrisperidone. For patients treated with the recommended dose of 25 mg Risperidone for Extended-Release Injectable Suspension and discontinuing from carbamazepine or other CYP 3A4 enzyme inducers, it is recommended to continue treatment with the 25 mg dose unless clinical judgment necessitates lowering the Risperidone for Extended-Release Injectable Suspension dose to 12.5 mg or necessitates interruption of Risperidone for Extended-Release Injectable Suspension treatment. The efficacy of the 12.5 mg dose has not been investigated in clinical trials [see also Dosage and Administration ( 2.5 )] 7.14 Drugs Metabolized by CYP 2D6 In vitro studies indicate that risperidone is a relatively weak inhibitor of CYP 2D6. Therefore, Risperidone for Extended-Release Injectable Suspension is not expected to substantially inhibit the clearance of drugs that are metabolized by this enzymatic pathway. In drug interaction studies, oral risperidone did not significantly affect the pharmacokinetics of donepezil and galantamine, which are metabolized by CYP 2D6.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action The mechanism of action of risperidone in schizophrenia is unclear. The drug’s therapeutic activity in schizophrenia could be mediated through a combination of dopamine Type 2 (D 2 ) and serotonin Type 2 (5HT 2 ) receptor antagonism. The clinical effect from risperidone results from the combined concentrations of risperidone and its major active metabolite, 9-hydroxyrisperidone (paliperidone) [see Clinical Pharmacology ( 12.3 )] . Antagonism at receptors other than D 2 and 5HT 2 may explain some of the other effects of risperidone [see Clinical Pharmacology ( 12.1 )] . 12.2 Pharmacodynamics Risperidone is a monoaminergic antagonist with high affinity (Ki of 0.12 to 7.3 nM) for the serotonin Type 2 (5HT 2 ), dopamine Type 2 (D 2 ), α1 and α2 adrenergic, and H 1 histaminergic receptors. Risperidone showed low to moderate affinity (Ki of 47 to 253 nM) for the serotonin 5HT 1C , 5HT 1D , and 5HT 1A receptors, weak affinity (Ki of 620 to 800 nM) for the dopamine D 1 and haloperidol-sensitive sigma site, and no affinity (when tested at concentrations >10 -5 M) for cholinergic muscarinic or β1 and β2 adrenergic receptors. 12.3 Pharmacokinetics Absorption After a single intramuscular (gluteal) injection of Risperidone for Extended-Release Injectable Suspension, there is a small initial release of the drug (< 1% of the dose), followed by a lag time of 3 weeks. The main release of the drug starts from 3 weeks onward, is maintained from 4 to 6 weeks, and subsides by 7 weeks following the intramuscular injection. Therefore, oral antipsychotic supplementation should be given during the first 3 weeks of treatment with Risperidone for Extended-Release Injectable Suspension to maintain therapeutic levels until the main release of risperidone from the injection site has begun [see Dosage and Administration ( 2 )] . Following single doses of Risperidone for Extended-Release Injectable Suspension, the pharmacokinetics of risperidone, 9-hydroxyrisperidone (the major metabolite), and risperidone plus 9-hydroxyrisperidone were linear in the dosing range of 12.5 mg to 50 mg. The combination of the release profile and the dosage regimen (intramuscular injections every 2 weeks) of Risperidone for Extended-Release Injectable Suspension results in sustained therapeutic concentrations. Steady-state plasma concentrations are reached after 4 injections and are maintained for 4 to 6 weeks after the last injection. Following multiple doses of 25 mg and 50 mg Risperidone for Extended-Release Injectable Suspension, plasma concentrations of risperidone, 9-hydroxyrisperidone, and risperidone plus 9-hydroxyrisperidone were linear. Deltoid and gluteal intramuscular injections at the same doses are bioequivalent and, therefore, interchangeable. Distribution Once absorbed, risperidone is rapidly distributed. The volume of distribution is 1 to 2 L/kg. In plasma, risperidone is bound to albumin and α1-acid glycoprotein. The plasma protein binding of risperidone is approximately 90%, and that of its major metabolite, 9-hydroxyrisperidone, is 77%. Neither risperidone nor 9-hydroxyrisperidone displaces each other from plasma binding sites. High therapeutic concentrations of sulfamethazine (100 mcg/mL), warfarin (10 mcg/mL), and carbamazepine (10 mcg/mL) caused only a slight increase in the free fraction of risperidone at 10 ng/mL and of 9-hydroxyrisperidone at 50 ng/mL, changes of unknown clinical significance. Metabolism and Drug Interactions Risperidone is extensively metabolized in the liver. The main metabolic pathway is through hydroxylation of risperidone to 9-hydroxyrisperidone by the enzyme, CYP 2D6. A minor metabolic pathway is through N-dealkylation. The main metabolite, 9-hydroxyrisperidone, has similar pharmacological activity as risperidone. Consequently, the clinical effect of the drug results from the combined concentrations of risperidone plus 9-hydroxyrisperidone. CYP 2D6, also called debrisoquin hydroxylase, is the enzyme responsible for metabolism of many neuroleptics, antidepressants, antiarrhythmics, and other drugs. CYP 2D6 is subject to genetic polymorphism (about 6% to 8% of Caucasians, and a very low percentage of Asians, have little or no activity and are “poor metabolizers”) and to inhibition by a variety of substrates and some non-substrates, notably quinidine. Extensive CYP 2D6 metabolizers convert risperidone rapidly into 9-hydroxyrisperidone, whereas poor CYP 2D6 metabolizers convert it much more slowly. Although extensive metabolizers have lower risperidone and higher 9-hydroxyrisperidone concentrations than poor metabolizers, the pharmacokinetics of risperidone and 9-hydroxyrisperidone combined, after single and multiple doses, are similar in extensive and poor metabolizers. The interactions of Risperidone for Extended-Release Injectable Suspension with coadministration of other drugs have not been systematically evaluated in human subjects. Drug interactions are based primarily on experience with oral risperidone. Risperidone could be subject to two kinds of drug-drug interactions. First, inhibitors of CYP 2D6 interfere with conversion of risperidone to 9-hydroxyrisperidone [see Drug Interactions ( 7.11 )] . This occurs with quinidine, giving essentially all recipients a risperidone pharmacokinetic profile typical of poor metabolizers. The therapeutic benefits and adverse effects of risperidone in patients receiving quinidine have not been evaluated, but observations in a modest number (n≅70) of poor metabolizers given oral risperidone do not suggest important differences between poor and extensive metabolizers. Second, co-administration of carbamazepine and other known enzyme inducers (e.g., phenytoin, rifampin, and phenobarbital) with oral risperidone cause a decrease in the combined plasma concentrations of risperidone and 9-hydroxyrisperidone [see Drug Interactions ( 7.12 )] . It would also be possible for risperidone to interfere with metabolism of other drugs metabolized by CYP 2D6. Relatively weak binding of risperidone to the enzyme suggests this is unlikely [see Drug Interactions ( 7.11 )] . Excretion Risperidone and its metabolites are eliminated via the urine and, to a much lesser extent, via the feces. As illustrated by a mass balance study of a single 1 mg oral dose of 14 C-risperidone administered as solution to three healthy male volunteers, total recovery of radioactivity at 1 week was 84%, including 70% in the urine and 14% in the feces. The apparent half-life of risperidone plus 9-hydroxyrisperidone following Risperidone for Extended-Release Injectable Suspension administration is 3 to 6 days, and is associated with a monoexponential decline in plasma concentrations. This half-life of 3 to 6 days is related to the erosion of the microspheres and subsequent absorption of risperidone. The clearance of risperidone and risperidone plus 9-hydroxyrisperidone was 13.7 L/h and 5.0 L/h in extensive CYP 2D6 metabolizers, and 3.3 L/h and 3.2 L/h in poor CYP 2D6 metabolizers, respectively. No accumulation of risperidone was observed during long-term use (up to 12 months) in patients treated every 2 weeks with 25 mg or 50 mg Risperidone for Extended-Release Injectable Suspension. The elimination phase is complete approximately 7 to 8 weeks after the last injection. Renal Impairment In patients with moderate to severe renal disease treated with oral risperidone, clearance of the sum of risperidone and its active metabolite decreased by 60% compared with young healthy subjects. Although patients with renal impairment were not studied with Risperidone for Extended-Release Injectable Suspension, it is recommended that patients with renal impairment be carefully titrated on oral risperidone before treatment with Risperidone for Extended-Release Injectable Suspension is initiated at a dose of 25 mg. A lower initial dose of 12.5 mg may be appropriate when clinical factors warrant dose adjustment, such as in patients with renal impairment [see Dosage and Administration ( 2.4 )] . Hepatic Impairment While the pharmacokinetics of oral risperidone in subjects with liver disease were comparable to those in young healthy subjects, the mean free fraction of risperidone in plasma was increased by about 35% because of the diminished concentration of both albumin and α1-acid glycoprotein. Although patients with hepatic impairment were not studied with Risperidone for Extended-Release Injectable Suspension, it is recommended that patients with hepatic impairment be carefully titrated on oral risperidone before treatment with Risperidone for Extended-Release Injectable Suspension is initiated at a dose of 25 mg. A lower initial dose of 12.5 mg may be appropriate when clinical factors warrant dose adjustment, such as in patients with hepatic impairment [see Dosage and Administration ( 2.4 )] . Elderly In an open-label trial, steady-state concentrations of risperidone plus 9-hydroxyrisperidone in otherwise healthy elderly patients (≥ 65 years old) treated with Risperidone for Extended-Release Injectable Suspension for up to 12 months fell within the range of values observed in otherwise healthy nonelderly patients. Dosing recommendations are the same for otherwise healthy elderly patients and nonelderly patients [see Dosage and Administration ( 2 )] . Race and Gender Effects No specific pharmacokinetic study was conducted to investigate race and gender effects, but a population pharmacokinetic analysis did not identify important differences in the disposition of risperidone due to gender (whether or not corrected for body weight) or race.
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action The mechanism of action of risperidone in schizophrenia is unclear. The drug’s therapeutic activity in schizophrenia could be mediated through a combination of dopamine Type 2 (D 2 ) and serotonin Type 2 (5HT 2 ) receptor antagonism. The clinical effect from risperidone results from the combined concentrations of risperidone and its major active metabolite, 9-hydroxyrisperidone (paliperidone) [see Clinical Pharmacology ( 12.3 )] . Antagonism at receptors other than D 2 and 5HT 2 may explain some of the other effects of risperidone [see Clinical Pharmacology ( 12.1 )] .
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Risperidone is a monoaminergic antagonist with high affinity (Ki of 0.12 to 7.3 nM) for the serotonin Type 2 (5HT 2 ), dopamine Type 2 (D 2 ), α1 and α2 adrenergic, and H 1 histaminergic receptors. Risperidone showed low to moderate affinity (Ki of 47 to 253 nM) for the serotonin 5HT 1C , 5HT 1D , and 5HT 1A receptors, weak affinity (Ki of 620 to 800 nM) for the dopamine D 1 and haloperidol-sensitive sigma site, and no affinity (when tested at concentrations >10 -5 M) for cholinergic muscarinic or β1 and β2 adrenergic receptors.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Absorption After a single intramuscular (gluteal) injection of Risperidone for Extended-Release Injectable Suspension, there is a small initial release of the drug (< 1% of the dose), followed by a lag time of 3 weeks. The main release of the drug starts from 3 weeks onward, is maintained from 4 to 6 weeks, and subsides by 7 weeks following the intramuscular injection. Therefore, oral antipsychotic supplementation should be given during the first 3 weeks of treatment with Risperidone for Extended-Release Injectable Suspension to maintain therapeutic levels until the main release of risperidone from the injection site has begun [see Dosage and Administration ( 2 )] . Following single doses of Risperidone for Extended-Release Injectable Suspension, the pharmacokinetics of risperidone, 9-hydroxyrisperidone (the major metabolite), and risperidone plus 9-hydroxyrisperidone were linear in the dosing range of 12.5 mg to 50 mg. The combination of the release profile and the dosage regimen (intramuscular injections every 2 weeks) of Risperidone for Extended-Release Injectable Suspension results in sustained therapeutic concentrations. Steady-state plasma concentrations are reached after 4 injections and are maintained for 4 to 6 weeks after the last injection. Following multiple doses of 25 mg and 50 mg Risperidone for Extended-Release Injectable Suspension, plasma concentrations of risperidone, 9-hydroxyrisperidone, and risperidone plus 9-hydroxyrisperidone were linear. Deltoid and gluteal intramuscular injections at the same doses are bioequivalent and, therefore, interchangeable. Distribution Once absorbed, risperidone is rapidly distributed. The volume of distribution is 1 to 2 L/kg. In plasma, risperidone is bound to albumin and α1-acid glycoprotein. The plasma protein binding of risperidone is approximately 90%, and that of its major metabolite, 9-hydroxyrisperidone, is 77%. Neither risperidone nor 9-hydroxyrisperidone displaces each other from plasma binding sites. High therapeutic concentrations of sulfamethazine (100 mcg/mL), warfarin (10 mcg/mL), and carbamazepine (10 mcg/mL) caused only a slight increase in the free fraction of risperidone at 10 ng/mL and of 9-hydroxyrisperidone at 50 ng/mL, changes of unknown clinical significance. Metabolism and Drug Interactions Risperidone is extensively metabolized in the liver. The main metabolic pathway is through hydroxylation of risperidone to 9-hydroxyrisperidone by the enzyme, CYP 2D6. A minor metabolic pathway is through N-dealkylation. The main metabolite, 9-hydroxyrisperidone, has similar pharmacological activity as risperidone. Consequently, the clinical effect of the drug results from the combined concentrations of risperidone plus 9-hydroxyrisperidone. CYP 2D6, also called debrisoquin hydroxylase, is the enzyme responsible for metabolism of many neuroleptics, antidepressants, antiarrhythmics, and other drugs. CYP 2D6 is subject to genetic polymorphism (about 6% to 8% of Caucasians, and a very low percentage of Asians, have little or no activity and are “poor metabolizers”) and to inhibition by a variety of substrates and some non-substrates, notably quinidine. Extensive CYP 2D6 metabolizers convert risperidone rapidly into 9-hydroxyrisperidone, whereas poor CYP 2D6 metabolizers convert it much more slowly. Although extensive metabolizers have lower risperidone and higher 9-hydroxyrisperidone concentrations than poor metabolizers, the pharmacokinetics of risperidone and 9-hydroxyrisperidone combined, after single and multiple doses, are similar in extensive and poor metabolizers. The interactions of Risperidone for Extended-Release Injectable Suspension with coadministration of other drugs have not been systematically evaluated in human subjects. Drug interactions are based primarily on experience with oral risperidone. Risperidone could be subject to two kinds of drug-drug interactions. First, inhibitors of CYP 2D6 interfere with conversion of risperidone to 9-hydroxyrisperidone [see Drug Interactions ( 7.11 )] . This occurs with quinidine, giving essentially all recipients a risperidone pharmacokinetic profile typical of poor metabolizers. The therapeutic benefits and adverse effects of risperidone in patients receiving quinidine have not been evaluated, but observations in a modest number (n≅70) of poor metabolizers given oral risperidone do not suggest important differences between poor and extensive metabolizers. Second, co-administration of carbamazepine and other known enzyme inducers (e.g., phenytoin, rifampin, and phenobarbital) with oral risperidone cause a decrease in the combined plasma concentrations of risperidone and 9-hydroxyrisperidone [see Drug Interactions ( 7.12 )] . It would also be possible for risperidone to interfere with metabolism of other drugs metabolized by CYP 2D6. Relatively weak binding of risperidone to the enzyme suggests this is unlikely [see Drug Interactions ( 7.11 )] . Excretion Risperidone and its metabolites are eliminated via the urine and, to a much lesser extent, via the feces. As illustrated by a mass balance study of a single 1 mg oral dose of 14 C-risperidone administered as solution to three healthy male volunteers, total recovery of radioactivity at 1 week was 84%, including 70% in the urine and 14% in the feces. The apparent half-life of risperidone plus 9-hydroxyrisperidone following Risperidone for Extended-Release Injectable Suspension administration is 3 to 6 days, and is associated with a monoexponential decline in plasma concentrations. This half-life of 3 to 6 days is related to the erosion of the microspheres and subsequent absorption of risperidone. The clearance of risperidone and risperidone plus 9-hydroxyrisperidone was 13.7 L/h and 5.0 L/h in extensive CYP 2D6 metabolizers, and 3.3 L/h and 3.2 L/h in poor CYP 2D6 metabolizers, respectively. No accumulation of risperidone was observed during long-term use (up to 12 months) in patients treated every 2 weeks with 25 mg or 50 mg Risperidone for Extended-Release Injectable Suspension. The elimination phase is complete approximately 7 to 8 weeks after the last injection. Renal Impairment In patients with moderate to severe renal disease treated with oral risperidone, clearance of the sum of risperidone and its active metabolite decreased by 60% compared with young healthy subjects. Although patients with renal impairment were not studied with Risperidone for Extended-Release Injectable Suspension, it is recommended that patients with renal impairment be carefully titrated on oral risperidone before treatment with Risperidone for Extended-Release Injectable Suspension is initiated at a dose of 25 mg. A lower initial dose of 12.5 mg may be appropriate when clinical factors warrant dose adjustment, such as in patients with renal impairment [see Dosage and Administration ( 2.4 )] . Hepatic Impairment While the pharmacokinetics of oral risperidone in subjects with liver disease were comparable to those in young healthy subjects, the mean free fraction of risperidone in plasma was increased by about 35% because of the diminished concentration of both albumin and α1-acid glycoprotein. Although patients with hepatic impairment were not studied with Risperidone for Extended-Release Injectable Suspension, it is recommended that patients with hepatic impairment be carefully titrated on oral risperidone before treatment with Risperidone for Extended-Release Injectable Suspension is initiated at a dose of 25 mg. A lower initial dose of 12.5 mg may be appropriate when clinical factors warrant dose adjustment, such as in patients with hepatic impairment [see Dosage and Administration ( 2.4 )] . Elderly In an open-label trial, steady-state concentrations of risperidone plus 9-hydroxyrisperidone in otherwise healthy elderly patients (≥ 65 years old) treated with Risperidone for Extended-Release Injectable Suspension for up to 12 months fell within the range of values observed in otherwise healthy nonelderly patients. Dosing recommendations are the same for otherwise healthy elderly patients and nonelderly patients [see Dosage and Administration ( 2 )] . Race and Gender Effects No specific pharmacokinetic study was conducted to investigate race and gender effects, but a population pharmacokinetic analysis did not identify important differences in the disposition of risperidone due to gender (whether or not corrected for body weight) or race.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS Risperidone for Extended-Release Injectable Suspension is contraindicated in patients with a known hypersensitivity to either risperidone or paliperidone, or to any of the excipients in the Risperidone for Extended-Release Injectable Suspension formulation. Hypersensitivity reactions, including anaphylactic reactions and angioedema, have been reported in patients treated with risperidone and in patients treated with paliperidone. Paliperidone is a metabolite of risperidone. Known hypersensitivity to risperidone, paliperidone, or to any excipients in Risperidone for Extended-Release Injectable Suspension. ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION Risperidone for Extended-Release Injectable Suspension contains risperidone, an atypical antipsychotic belonging to the chemical class of benzisoxazole derivatives. The chemical designation is 3-[2-[4-(6-fluoro-1,2-benzisoxazol-3-yl)-1-piperidinyl]ethyl]-6,7,8,9-tetrahydro-2-methyl-4H-pyrido[1,2-a]pyrimidin-4-one. Its molecular formula is C 23 H 27 FN 4 O 2 and its molecular weight is 410.49. The structural formula is: Risperidone is practically insoluble in water, freely soluble in methylene chloride, and soluble in methanol and 0.1 N HCl. Risperidone for Extended-Release Injectable Suspension is a combination of extended-release microspheres for injection and diluent for parenteral use. The extended-release microspheres formulation is a white to off-white, sterile, free-flowing powder that is available in dosage strengths of 12.5 mg, 25 mg, 37.5 mg, or 50 mg risperidone per vial. Risperidone is microencapsulated in 75:25 polylactide-co-glycolide (PLG) at a concentration of 381 mg risperidone per gram of microspheres. The diluent for parenteral use is a clear, colorless solution. Composition of the diluent includes 1 mg/mL citric acid anhydrous, 1.27 mg/mL disodium hydrogen phosphate dihydrate, 1 mg/mL polysorbate 20, 22.5 mg/mL sodium carboxymethyl cellulose, 6 mg/mL sodium chloride, 0.54 mg/mL sodium hydroxide, and water for injection. The microspheres are suspended in the diluent prior to injection. Risperidone for Extended-Release Injectable Suspension is provided as a single-dose pack, consisting of a vial containing the microspheres, a pre-filled syringe containing the diluent, a vial adapter, and two Terumo SurGuard ® 3 Needles (a 21 G UTW 1-inch needle with needle protection device for deltoid administration and a 20 G TW 2-inch needle with needle protection device for gluteal administration). 1
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION For patients who have never taken oral risperidone, it is recommended to establish tolerability with oral risperidone prior to initiating treatment with Risperidone for Extended-Release Injectable Suspension. Risperidone for Extended-Release Injectable Suspension should be administered every 2 weeks by deep intramuscular deltoid or gluteal injection. Each injection should be administered by a health care professional using the appropriate enclosed safety needle [see Dosage and Administration ( 2.8 )] . For deltoid administration, use the 1-inch needle alternating injections between the two arms. For gluteal administration, use the 2-inch needle alternating injections between the two buttocks. Do not administer intravenously. For patients who have never taken oral risperidone, tolerability should be established with oral risperidone prior to initiating treatment with Risperidone for Extended-Release Injectable Suspension. ( 2 ) Administer by deep intramuscular deltoid or gluteal injection. Each injection should be administered by a health care professional using the appropriate enclosed safety needle (1-inch for deltoid administration alternating injections between the two arms and 2-inch for gluteal administration alternating injections between the two buttocks). Do not administer intravenously. ( 2 ) 25 mg intramuscular every 2 weeks. Patients not responding to 25 mg may benefit from a higher dose of 37.5 mg or 50 mg. The maximum dose should not exceed 50 mg every 2 weeks. ( 2 ) Oral risperidone (or another antipsychotic medication) should be given with the first injection of Risperidone for Extended-Release Injectable Suspension, and continued for 3 weeks (and then discontinued) to ensure adequate therapeutic plasma concentrations from Risperidone for Extended-Release Injectable Suspension. ( 2 ) Upward dose adjustment of Risperidone for Extended-Release Injectable Suspension should not be made more frequently than every 4 weeks. Clinical effects of each upward dose adjustment should not be anticipated earlier than 3 weeks after injection. ( 2 ) Avoid inadvertent administration into a blood vessel. ( 5.16 ) See Full Prescribing Information Section 2.8 for instructions for use. 2.1 Schizophrenia The recommended dose for the treatment of schizophrenia is 25 mg intramuscular every 2 weeks. Although dose response for effectiveness has not been established for Risperidone for Extended-Release Injectable Suspension, some patients not responding to 25 mg may benefit from a higher dose of 37.5 mg or 50 mg. The maximum dose should not exceed 50 mg Risperidone for Extended-Release Injectable Suspension every 2 weeks. No additional benefit was observed with dosages greater than 50 mg Risperidone for Extended-Release Injectable Suspension; however, a higher incidence of adverse effects was observed. The efficacy of Risperidone for Extended-Release Injectable Suspension in the treatment of schizophrenia has not been evaluated in controlled clinical trials for longer than 12 weeks. Although controlled studies have not been conducted to answer the question of how long patients with schizophrenia should be treated with Risperidone for Extended-Release Injectable Suspension, oral risperidone has been shown to be effective in delaying time to relapse in longer-term use. It is recommended that responding patients be continued on treatment with Risperidone for Extended-Release Injectable Suspension at the lowest dose needed. The physician who elects to use Risperidone for Extended-Release Injectable Suspension for extended periods should periodically re-evaluate the long-term risks and benefits of the drug for the individual patient. 2.2 Bipolar Disorder The recommended dose for monotherapy or adjunctive therapy to lithium or valproate for the maintenance treatment of Bipolar I Disorder is 25 mg intramuscular every 2 weeks. Some patients may benefit from a higher dose of 37.5 mg or 50 mg. Dosages above 50 mg have not been studied in this population. The physician who elects to use Risperidone for Extended-Release Injectable Suspension for extended periods should periodically re-evaluate the long-term risks and benefits of the drug for the individual patient. 2.3 General Dosing Information A lower initial dose of 12.5 mg may be appropriate when clinical factors warrant dose adjustment, such as in patients with hepatic or renal impairment, for certain drug interactions that increase risperidone plasma concentrations [see Drug Interactions ( 7.11 )] or in patients who have a history of poor tolerability to psychotropic medications. The efficacy of the 12.5 mg dose has not been investigated in clinical trials. Oral risperidone (or another antipsychotic medication) should be given with the first injection of Risperidone for Extended-Release Injectable Suspension and continued for 3 weeks (and then discontinued) to ensure that adequate therapeutic plasma concentrations are maintained prior to the main release phase of risperidone from the injection site [see Clinical Pharmacology ( 12.3 )] . Upward dose adjustment should not be made more frequently than every 4 weeks. The clinical effects of this dose adjustment should not be anticipated earlier than 3 weeks after the first injection with the higher dose. In patients with clinical factors such as hepatic or renal impairment or certain drug interactions that increase risperidone plasma concentrations [see Drug Interactions ( 7.11 )] , dose reduction as low as 12.5 mg may be appropriate. The efficacy of the 12.5 mg dose has not been investigated in clinical trials. Do not combine two different dose strengths of Risperidone for Extended-Release Injectable Suspension in a single administration. 2.4 Dosage in Special Populations Elderly For elderly patients treated with Risperidone for Extended-Release Injectable Suspension, the recommended dosage is 25 mg intramuscular every 2 weeks. Oral risperidone (or another antipsychotic medication) should be given with the first injection of Risperidone for Extended-Release Injectable Suspension and should be continued for 3 weeks to ensure that adequate therapeutic plasma concentrations are maintained prior to the main release phase of risperidone from the injection site [see Clinical Pharmacology ( 12.3 )] . Renal or Hepatic Impairment Patients with renal or hepatic impairment should be treated with titrated doses of oral risperidone prior to initiating treatment with Risperidone for Extended-Release Injectable Suspension. The recommended starting dose is 0.5 mg oral risperidone twice daily during the first week, which can be increased to 1 mg twice daily or 2 mg once daily during the second week. If a total daily dose of at least 2 mg oral risperidone is well tolerated, an injection of 25 mg Risperidone for Extended-Release Injectable Suspension can be administered every 2 weeks. Oral supplementation should be continued for 3 weeks after the first injection until the main release of risperidone from the injection site has begun. In some patients, slower titration may be medically appropriate. Alternatively, a starting dose of Risperidone for Extended-Release Injectable Suspension of 12.5 mg may be appropriate. The efficacy of the 12.5 mg dose has not been investigated in clinical trials. Patients with renal impairment may have less ability to eliminate risperidone than normal adults. Patients with impaired hepatic function may have an increase in the free fraction of the risperidone, possibly resulting in an enhanced effect [see Clinical Pharmacology ( 12.3 )] . Elderly patients and patients with a predisposition to hypotensive reactions or for whom such reactions would pose a particular risk should be instructed in nonpharmacologic interventions that help to reduce the occurrence of orthostatic hypotension (e.g., sitting on the edge of the bed for several minutes before attempting to stand in the morning and slowly rising from a seated position). These patients should avoid sodium depletion or dehydration, and circumstances that accentuate hypotension (alcohol intake, high ambient temperature, etc.). Monitoring of orthostatic vital signs should be considered [see Warnings and Precautions ( 5.7 )] . 2.5 Reinitiation of Treatment in Patients Previously Discontinued There are no data to specifically address reinitiation of treatment. When restarting patients who have had an interval off treatment with Risperidone for Extended-Release Injectable Suspension, supplementation with oral risperidone (or another antipsychotic medication) should be administered. 2.6 Switching from Other Antipsychotics There are no systematically collected data to specifically address switching patients from other antipsychotics to Risperidone for Extended-Release Injectable Suspension, or concerning concomitant administration with other antipsychotics. Previous antipsychotics should be continued for 3 weeks after the first injection of Risperidone for Extended-Release Injectable Suspension to ensure that therapeutic concentrations are maintained until the main release phase of risperidone from the injection site has begun [see Clinical Pharmacology ( 12.3 )] . For patients who have never taken oral risperidone, it is recommended to establish tolerability with oral risperidone prior to initiating treatment with Risperidone for Extended-Release Injectable Suspension. As recommended with other antipsychotic medications, the need for continuing existing EPS medication should be re-evaluated periodically. 2.7 Coadministration of Risperidone for Extended-Release Injectable Suspension with Certain Other Medications Coadministration of carbamazepine and other CYP 3A4 enzyme inducers (e.g., phenytoin, rifampin, phenobarbital) with risperidone would be expected to cause decreases in the plasma concentrations of the sum of risperidone and 9-hydroxyrisperidone combined, which could lead to decreased efficacy of Risperidone for Extended-Release Injectable Suspension treatment. The dose of risperidone needs to be titrated accordingly for patients receiving these enzyme inducers, especially during initiation or discontinuation of therapy with these inducers [see Drug Interactions ( 7.11 )] . At the initiation of therapy with carbamazepine or other known CYP 3A4 hepatic enzyme inducers, patients should be closely monitored during the first 4 to 8 weeks, since the dose of Risperidone for Extended-Release Injectable Suspension may need to be adjusted. A dose increase, or additional oral risperidone, may need to be considered. On discontinuation of carbamazepine or other CYP 3A4 hepatic enzyme inducers, the dosage of Risperidone for Extended-Release Injectable Suspension should be re-evaluated and, if necessary, decreased. Patients may be placed on a lower dose of Risperidone for Extended-Release Injectable Suspension between 2 to 4 weeks before the planned discontinuation of carbamazepine or other CYP 3A4 inducers to adjust for the expected increase in plasma concentrations of risperidone plus 9-hydroxyrisperidone. For patients treated with the recommended dose of 25 mg Risperidone for Extended-Release Injectable Suspension and discontinuing from carbamazepine or other CYP3A4 enzyme inducers, it is recommended to continue treatment with the 25 mg dose unless clinical judgment necessitates lowering the Risperidone for Extended-Release Injectable Suspension dose to 12.5 mg or necessitates interruption of Risperidone for Extended-Release Injectable Suspension treatment. The efficacy of the 12.5 mg dose has not been investigated in clinical trials. Fluoxetine and paroxetine, CYP 2D6 inhibitors, have been shown to increase the plasma concentration of risperidone 2.5 to 2.8 fold and 3 to 9 fold respectively. Fluoxetine did not affect the plasma concentration of 9-hydroxyrisperidone. Paroxetine lowered the concentration of 9-hydroxyrisperidone by about 10%. The dose of risperidone needs to be titrated accordingly when fluoxetine or paroxetine is coadministered. When either concomitant fluoxetine or paroxetine is initiated or discontinued, the physician should re-evaluate the dose of Risperidone for Extended-Release Injectable Suspension. When initiation of fluoxetine or paroxetine is considered, patients may be placed on a lower dose of Risperidone for Extended-Release Injectable Suspension between 2 to 4 weeks before the planned start of fluoxetine or paroxetine therapy to adjust for the expected increase in plasma concentrations of risperidone. When fluoxetine or paroxetine is initiated in patients receiving the recommended dose of 25 mg Risperidone for Extended-Release Injectable Suspension, it is recommended to continue treatment with the 25 mg dose unless clinical judgment necessitates lowering the Risperidone for Extended-Release Injectable Suspension dose to 12.5 mg or necessitates interruption of Risperidone for Extended-Release Injectable Suspension treatment. When Risperidone for Extended-Release Injectable Suspension is initiated in patients already receiving fluoxetine or paroxetine, a starting dose of 12.5 mg can be considered. The efficacy of the 12.5 mg dose has not been investigated in clinical trials. The effects of discontinuation of concomitant fluoxetine or paroxetine therapy on the pharmacokinetics of risperidone and 9-hydroxyrisperidone have not been studied [see Drug Interactions ( 7.11 )]. 2.8 Instructions for Use For deltoid or gluteal intramuscular injection only Each injection should be administered by a healthcare professional. IMPORTANT RESOURCES For additional information call Teva at 1-888-838-2872. Important Information Risperidone for Extended-Release Injectable Suspension requires close attention to these step-by-step Instructions for Use to help ensure successful administration. Use components provided The components in this dose pack are specifically designed for use with Risperidone for Extended-Release Injectable Suspension. Risperidone for Extended-Release Injectable Suspension must be reconstituted only in the diluent supplied in the dose pack. Do not substitute ANY components of the dose pack. Do not store suspension after reconstitution Administer dose as soon as possible after reconstitution to avoid settling. Proper dosing The entire contents of the vial must be administered to ensure intended dose of Risperidone for Extended-Release Injectable Suspension is delivered. SINGLE-DOSE DEVICE Do not reuse. Medical devices require specific material characteristics to perform as intended. These characteristics have been verified for single-dose only. Any attempt to re-process the device for subsequent re-use may adversely affect the integrity of the device or lead to deterioration in performance. Dose pack contents Step 1 Assemble components Take out dose pack Connect vial adapter to vial Wait 30 minutes Remove dose pack from the refrigerator and allow to sit at room temperature for at least 30 minutes before reconstituting. Do not warm any other way. Remove cap from vial Flip off colored cap from vial. Wipe top of the grey stopper with an alcohol swab . Allow to air dry. Do not remove grey rubber stopper. Prepare vial adapter Hold sterile blister as shown. Peel the blister film from backing and remove the vial adapter from its packaging by holding between the white luer cap and the skirt. Do not touch spike tip and luer tip connector of the vial adapter at any time. This will result in contamination. Connect vial adapter to vial Place vial on a hard surface and hold by the base. Center vial adapter over the grey rubber stopper. Push vial adapter straight down onto vial top until it snaps securely into place. CLEAN the luer tip of the vial adapter with an alcohol wipe Do not place vial adapter on at an angle or diluent may leak upon transfer to the vial. Do not shake. Do not touch exposed luer tip connector on vial adapter. This will result in contamination. Connect prefilled syringe to vial adapter Use proper grip Hold by white collar at the tip of the syringe. Do not hold syringe by the glass barrel during assembly. Remove cap Holding the white collar, snap off the white cap. Do not twist or cut off the white cap. Do not touch syringe tip. This will result in contamination. The broken-off cap can be discarded. Connect syringe to vial adapter Hold vial adapter by skirt to keep stationary. Hold syringe by white collar then insert tip into the luer tip connector of the vial adapter. Do not hold the glass syringe barrel. This may cause the white collar to loosen or detach. Attach the syringe to the vial adapter with a firm clockwise twisting motion until it feels snug. Do not over-tighten. Over-tightening may cause the syringe tip to break. Step 2 Reconstitute microspheres Inject diluent Inject entire amount of diluent from syringe into the vial. Suspend microspheres in diluent Continuing to hold down the plunger rod, shake vigorously for at least 10 seconds, as shown. Check the suspension. When properly mixed, the suspension appears uniform, thick and milky in color. Microspheres will be visible in the liquid. Immediately proceed to the next step so suspension does not settle. Transfer suspension to syringe Invert vial completely. Slowly pull plunger rod down to withdraw entire contents from the vial into the syringe. Remove vial adapter Hold white collar on the syringe and unscrew from vial adapter. Tear section of the vial label at the perforation. Apply detached label to the syringe for identification purposes. Discard both vial and vial adapter appropriately. Step 3 Attach needle Select appropriate needle Choose needle based on injection location (gluteal or deltoid). Attach needle Peel blister pouch open part way and use to grasp the base of the needle, as shown. Holding the white collar on the syringe , attach syringe to needle luer connection with a firm clockwise twisting motion until snug. Do not touch needle luer opening. This will result in contamination. Resuspend microspheres Fully remove the blister pouch. Just before injection, shake syringe vigorously again, as some settling will have occurred. Step 4 Inject dose Remove transparent needle protector Move the needle safety device back towards the syringe, as shown. Then hold white collar on syringe and carefully pull the transparent needle protector straight off. Do not twist transparent needle protector, as the luer connection may loosen. Remove air bubbles Hold needle upright and tap gently to make any air bubbles rise to the top. Slowly and carefully press plunger rod upward to remove air. Inject Immediately inject entire contents of syringe intramuscularly into the gluteal or deltoid muscle of the patient. Gluteal injection should be made into the upper-outer quadrant of the gluteal area. Do not administer intravenously. Secure needle in safety device Using one hand , place needle safety device at a 45-degree angle on a hard, flat surface. Press down with a firm, quick motion until needle is fully engaged in safety device. Avoid needle stick injury: Do not use two hands. Do not intentionally disengage or mishandle the needle safety device. Do not attempt to straighten the needle or engage the safety device if the needle is bent or damaged. Properly dispose of needles Check to confirm needle safety device is fully engaged. Discard in an approved sharps container. Also discard the unused needle provided in the dose pack. 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1
| |
| | | | |
| | | |
| | | |||
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Risperidone for Extended-Release Injectable Suspension is available in dosage strengths of 12.5 mg, 25 mg, 37.5 mg, and 50 mg risperidone. It is provided as a single-dose pack, consisting of a vial containing the risperidone microspheres, a pre-filled syringe containing 2 mL of diluent for Risperidone for Extended-Release Injectable Suspension, a vial adapter, and two Terumo SurGuard ® 3 Needles for intramuscular injection (a 21 G UTW 1-inch needle with needle protection device for deltoid administration and a 20 G TW 2-inch needle with needle protection device for gluteal administration). Vial kits: 12.5 mg, 25 mg, 37.5 mg, and 50 mg ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE Risperidone for Extended-Release Injectable Suspension is an atypical antipsychotic indicated: for the treatment of schizophrenia. ( 1.1 ) as monotherapy or as adjunctive therapy to lithium or valproate for the maintenance treatment of Bipolar I Disorder. ( 1.2 ) 1.1 Schizophrenia Risperidone for Extended-Release Injectable Suspension is indicated for the treatment of schizophrenia [see Clinical Studies ( 14.1 )] . 1.2 Bipolar Disorder Risperidone for Extended-Release Injectable Suspension is indicated as monotherapy or as adjunctive therapy to lithium or valproate for the maintenance treatment of Bipolar I Disorder [see Clinical Studies ( 14.2 , 14.3 )] .
Spl product data elements
Usually a list of ingredients in a drug product.Risperidone Risperidone Risperidone Risperidone RISPERIDONE RISPERIDONE POLY(DL-LACTIC-CO-GLYCOLIC ACID), (75:25; 9500 MW) diluent diluent ANHYDROUS CITRIC ACID SODIUM PHOSPHATE, DIBASIC, DIHYDRATE POLYSORBATE 20 CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM SODIUM CHLORIDE SODIUM HYDROXIDE WATER Risperidone Risperidone Risperidone Risperidone RISPERIDONE RISPERIDONE POLY(DL-LACTIC-CO-GLYCOLIC ACID), (75:25; 9500 MW) diluent diluent ANHYDROUS CITRIC ACID SODIUM PHOSPHATE, DIBASIC, DIHYDRATE POLYSORBATE 20 CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM SODIUM CHLORIDE SODIUM HYDROXIDE WATER Risperidone Risperidone Risperidone Risperidone RISPERIDONE RISPERIDONE POLY(DL-LACTIC-CO-GLYCOLIC ACID), (75:25; 9500 MW) diluent diluent ANHYDROUS CITRIC ACID SODIUM PHOSPHATE, DIBASIC, DIHYDRATE POLYSORBATE 20 CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM SODIUM CHLORIDE SODIUM HYDROXIDE WATER Risperidone Risperidone Risperidone Risperidone RISPERIDONE RISPERIDONE POLY(DL-LACTIC-CO-GLYCOLIC ACID), (75:25; 9500 MW) diluent diluent ANHYDROUS CITRIC ACID SODIUM PHOSPHATE, DIBASIC, DIHYDRATE POLYSORBATE 20 CARBOXYMETHYLCELLULOSE SODIUM, UNSPECIFIED FORM SODIUM CHLORIDE SODIUM HYDROXIDE WATER
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis - Oral Risperidone was administered in the diet at doses of 0.63, 2.5, and 10 mg/kg for 18 months to mice and for 25 months to rats. These doses are equivalent to approximately 0.2, 0.75, and 3 times (mice) and 0.4, 1.5, and 6 times (rats) the MRHD of 16 mg/day, based on mg/m 2 body surface area. A maximum tolerated dose was not achieved in male mice. There was a significant increase in pituitary gland adenomas, endocrine pancreatic adenomas, and mammary gland adenocarcinomas. The table below summarizes the multiples of the human dose on mg/m 2 (mg/kg) basis at which these tumors occurred. Multiples of Maximum Human Dose in mg/m 2 (mg/kg) Tumor Type Species Sex Lowest Effect Highest No-Effect Level Level Pituitary adenomas mouse Female 0.75 (9.4) 0.2 (2.4) Endocrine pancreas adenomas rat Male 1.5 (9.4) 0.4 (2.4) Mammary gland adenocarcinomas mouse Female 0.2 (2.4) none rat Female 0.4 (2.4) none rat Male 6.0 (37.5) 1.5 (9.4) Mammary gland neoplasm, Total rat Male 1.5 (9.4) 0.4 (2.4) Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the risperidone carcinogenicity studies; however, measurements during subchronic toxicity studies showed that risperidone elevated serum prolactin levels 5 to 6 fold in mice and rats at the same doses used in the carcinogenicity studies. An increase in mammary, pituitary, and endocrine pancreas neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin-mediated. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unclear [see Warnings and Precautions ( 5.6 )] . Carcinogenesis - Intramuscular Risperidone was evaluated in a 24-month carcinogenicity study in which SPF Wistar rats were treated every 2 weeks with intramuscular injections of either 5 mg/kg or 40 mg/kg of risperidone. These doses are 1 and 8 times the MRHD (50 mg) on a mg/m 2 basis. A control group received injections of 0.9% NaCl, and a vehicle control group was injected with placebo microspheres. There was a significant increase in pituitary gland adenomas, endocrine pancreas adenomas, and adrenomedullary pheochromocytomas at 8 times the intramuscular MRHD on a mg/m 2 basis. The incidence of mammary gland adenocarcinomas was significantly increased in female rats at both doses (1 and 8 times the intramuscular MRHD on a mg/m 2 basis). A significant increase in renal tubular tumors (adenoma, adenocarcinomas) was observed in male rats at 8 times the intramuscular MRHD on a mg/m 2 basis. Plasma exposures (AUC) in rats were 0.3 and 2 times (at 5 and 40 mg/kg, respectively) the expected plasma exposure (AUC) at the intramuscular MRHD. Dopamine D 2 receptor antagonists have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the carcinogenicity studies of oral risperidone; however, measurements taken during subchronic toxicity studies showed that oral risperidone elevated serum prolactin levels 5- to 6-fold in mice and rats at the same doses used in the oral carcinogenicity studies. Serum prolactin levels increased in a dose-dependent manner up to 6- and 1.5-fold in male and female rats, respectively, at the end of the 24-month treatment with risperidone every 2 weeks intramuscular. Increases in the incidence of pituitary gland, endocrine pancreas, and mammary gland neoplasms have been found in rodents after chronic administration of other antipsychotic drugs and may be prolactin-mediated. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unknown [see Warnings and Precautions ( 5.6 )] . Mutagenesis No evidence of mutagenic or clastogenic potential for risperidone was found in the in vitro tests of Ames gene mutation, the mouse lymphoma assay, rat hepatocyte DNA-repair assay, the chromosomal aberration test in human lymphocytes, Chinese hamster ovary cells, or in the in vivo micronucleus test in mice, and the sex-linked recessive lethal test in Drosophila . In addition, no evidence of mutagenic potential was found in the in vitro Ames reverse mutation test for Risperidone for Extended-Release Injectable Suspension. Impairment of Fertility Oral risperidone (0.16 to 5 mg/kg) impaired mating, but not fertility, in rat reproductive studies at doses 0.1 to 3 times the oral maximum recommended human dose (MRHD of 16 mg/day) based on mg/m 2 body surface area. The effect appeared to be in females, since impaired mating behavior was not noted in the male fertility study. In a subchronic study in Beagle dogs in which oral risperidone was administered at doses of 0.31 to 5 mg/kg, sperm motility and concentration were decreased at doses 0.6 to 10 times the oral MRHD on mg/m 2 basis. Dose-related decreases were also noted in serum testosterone at the same doses. Serum testosterone and sperm parameters partially recovered, but remained decreased after treatment was discontinued. A no-effect dose could not be determined in either rat or dog.
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis - Oral Risperidone was administered in the diet at doses of 0.63, 2.5, and 10 mg/kg for 18 months to mice and for 25 months to rats. These doses are equivalent to approximately 0.2, 0.75, and 3 times (mice) and 0.4, 1.5, and 6 times (rats) the MRHD of 16 mg/day, based on mg/m 2 body surface area. A maximum tolerated dose was not achieved in male mice. There was a significant increase in pituitary gland adenomas, endocrine pancreatic adenomas, and mammary gland adenocarcinomas. The table below summarizes the multiples of the human dose on mg/m 2 (mg/kg) basis at which these tumors occurred. Multiples of Maximum Human Dose in mg/m 2 (mg/kg) Tumor Type Species Sex Lowest Effect Highest No-Effect Level Level Pituitary adenomas mouse Female 0.75 (9.4) 0.2 (2.4) Endocrine pancreas adenomas rat Male 1.5 (9.4) 0.4 (2.4) Mammary gland adenocarcinomas mouse Female 0.2 (2.4) none rat Female 0.4 (2.4) none rat Male 6.0 (37.5) 1.5 (9.4) Mammary gland neoplasm, Total rat Male 1.5 (9.4) 0.4 (2.4) Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the risperidone carcinogenicity studies; however, measurements during subchronic toxicity studies showed that risperidone elevated serum prolactin levels 5 to 6 fold in mice and rats at the same doses used in the carcinogenicity studies. An increase in mammary, pituitary, and endocrine pancreas neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin-mediated. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unclear [see Warnings and Precautions ( 5.6 )] . Carcinogenesis - Intramuscular Risperidone was evaluated in a 24-month carcinogenicity study in which SPF Wistar rats were treated every 2 weeks with intramuscular injections of either 5 mg/kg or 40 mg/kg of risperidone. These doses are 1 and 8 times the MRHD (50 mg) on a mg/m 2 basis. A control group received injections of 0.9% NaCl, and a vehicle control group was injected with placebo microspheres. There was a significant increase in pituitary gland adenomas, endocrine pancreas adenomas, and adrenomedullary pheochromocytomas at 8 times the intramuscular MRHD on a mg/m 2 basis. The incidence of mammary gland adenocarcinomas was significantly increased in female rats at both doses (1 and 8 times the intramuscular MRHD on a mg/m 2 basis). A significant increase in renal tubular tumors (adenoma, adenocarcinomas) was observed in male rats at 8 times the intramuscular MRHD on a mg/m 2 basis. Plasma exposures (AUC) in rats were 0.3 and 2 times (at 5 and 40 mg/kg, respectively) the expected plasma exposure (AUC) at the intramuscular MRHD. Dopamine D 2 receptor antagonists have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the carcinogenicity studies of oral risperidone; however, measurements taken during subchronic toxicity studies showed that oral risperidone elevated serum prolactin levels 5- to 6-fold in mice and rats at the same doses used in the oral carcinogenicity studies. Serum prolactin levels increased in a dose-dependent manner up to 6- and 1.5-fold in male and female rats, respectively, at the end of the 24-month treatment with risperidone every 2 weeks intramuscular. Increases in the incidence of pituitary gland, endocrine pancreas, and mammary gland neoplasms have been found in rodents after chronic administration of other antipsychotic drugs and may be prolactin-mediated. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unknown [see Warnings and Precautions ( 5.6 )] . Mutagenesis No evidence of mutagenic or clastogenic potential for risperidone was found in the in vitro tests of Ames gene mutation, the mouse lymphoma assay, rat hepatocyte DNA-repair assay, the chromosomal aberration test in human lymphocytes, Chinese hamster ovary cells, or in the in vivo micronucleus test in mice, and the sex-linked recessive lethal test in Drosophila . In addition, no evidence of mutagenic potential was found in the in vitro Ames reverse mutation test for Risperidone for Extended-Release Injectable Suspension. Impairment of Fertility Oral risperidone (0.16 to 5 mg/kg) impaired mating, but not fertility, in rat reproductive studies at doses 0.1 to 3 times the oral maximum recommended human dose (MRHD of 16 mg/day) based on mg/m 2 body surface area. The effect appeared to be in females, since impaired mating behavior was not noted in the male fertility study. In a subchronic study in Beagle dogs in which oral risperidone was administered at doses of 0.31 to 5 mg/kg, sperm motility and concentration were decreased at doses 0.6 to 10 times the oral MRHD on mg/m 2 basis. Dose-related decreases were also noted in serum testosterone at the same doses. Serum testosterone and sperm parameters partially recovered, but remained decreased after treatment was discontinued. A no-effect dose could not be determined in either rat or dog.
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PACKAGE LABEL.PRINCIPAL DISPLAY PANEL NDC 0480-1554-08 Store Package in Refrigerator (see back panel for storage conditions) risperiDONE for Extended-Release Injectable Suspension 12.5 mg/vial Single-Dose Pack SINGLE-DOSE PACK CONTENTS: • One 12.5 mg vial of risperidone extended-release microspheres for injection • One single-dose pre-filled syringe containing 2 mL of diluent • One vial adapter • One 21-guage UTW 1" Terumo SurGuard® 3 safety needle for deltoid injection • One 20-guage TW 2" Terumo SurGuard® 3 safety needle for gluteal injection Do not substitute any components of the single-dose pack For deltoid or gluteal intramuscular injection only Each injection should be administered by a healthcare professional. PLEASE READ COMPLETE INSTRUCTIONS PRIOR TO USE. Rx only Single-Dose only carton 12.5 mg/vial
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL NDC 0480-1232-08 Store Package in Refrigerator (see back panel for storage conditions) risperiDONE for Extended-Release Injectable Suspension 25 mg/vial Single-Dose Pack SINGLE-DOSE PACK CONTENTS: • One 25 mg vial of risperidone extended-release microspheres for injection • One single-dose pre-filled syringe containing 2 mL of diluent • One vial adapter • One 21-guage UTW 1" Terumo SurGuard® 3 safety needle for deltoid injection • One 20-guage TW 2" Terumo SurGuard® 3 safety needle for gluteal injection Do not substitute any components of the single-dose pack For deltoid or gluteal intramuscular injection only Each injection should be administered by a healthcare professional. PLEASE READ COMPLETE INSTRUCTIONS PRIOR TO USE. Rx only Single-Dose only carton 25 mg/vial
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL NDC 0480-1342-08 Store Package in Refrigerator (see back panel for storage conditions) risperiDONE for Extended-Release Injectable Suspension 37.5 mg/vial Single-Dose Pack SINGLE-DOSE PACK CONTENTS: • One 37.5 mg vial of risperidone extended-release microspheres for injection • One single-dose pre-filled syringe containing 2 mL of diluent • One vial adapter • One 21-guage UTW 1" Terumo SurGuard® 3 safety needle for deltoid injection • One 20-guage TW 2" Terumo SurGuard® 3 safety needle for gluteal injection Do not substitute any components of the single-dose pack For deltoid or gluteal intramuscular injection only Each injection should be administered by a healthcare professional. PLEASE READ COMPLETE INSTRUCTIONS PRIOR TO USE. Rx only Single-Dose only carton 37.5 mg/vial
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL NDC 0480-1453-08 Store Package in Refrigerator (see back panel for storage conditions) risperiDONE for Extended-Release Injectable Suspension 50 mg/vial Single-Dose Pack SINGLE-DOSE PACK CONTENTS: • One 50 mg vial of risperidone extended-release microspheres for injection • One single-dose pre-filled syringe containing 2 mL of diluent • One vial adapter • One 21-guage UTW 1" Terumo SurGuard® 3 safety needle for deltoid injection • One 20-guage TW 2" Terumo SurGuard® 3 safety needle for gluteal injection Do not substitute any components of the single-dose pack For deltoid or gluteal intramuscular injection only Each injection should be administered by a healthcare professional. PLEASE READ COMPLETE INSTRUCTIONS PRIOR TO USE. Rx only Single-Dose only carton 50 mg/vial
Risperidone: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Physicians are advised to discuss the following issues with patients for whom they prescribe Risperidone for Extended-Release Injectable Suspension. Neuroleptic Malignant Syndrome (NMS) Counsel patients about a potentially fatal adverse reaction, Neuroleptic Malignant Syndrome (NMS), that has been reported in association with administration of antipsychotic drugs. Advise patients, family members, or caregivers to contact the healthcare provider or report to the emergency room if they experience signs and symptoms of NMS, including hyperpyrexia, muscle rigidity, altered mental status including delirium, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia) [see Warnings and Precautions ( 5.3 )] . Tardive Dyskinesia Counsel patients on the signs and symptoms of tardive dyskinesia and to contact their healthcare provider if these abnormal movements occur [see Warnings and Precautions ( 5.4 )] . Metabolic Changes Educate patients about the risk of metabolic changes, how to recognize symptoms of hyperglycemia and diabetes mellitus and the need for specific monitoring, including blood glucose, lipids, and weight [see Warnings and Precautions ( 5.5 )] . Orthostatic Hypotension Educate patients about the risk of orthostatic hypotension and syncope, particularly at the time of initiating treatment, re-initiating treatment, or increasing the dose. [see Warnings and Precautions ( 5.7 )] . Leukopenia/Neutropenia Advise patients with a pre-existing low WBC or a history of drug induced leukopenia/neutropenia that they should have their CBC monitored while being treated with Risperidone for Extended-Release Injectable Suspension [see Warnings and Precautions ( 5.9 )]. Hyperprolactinemia Counsel patients on signs and symptoms of hyperprolactinemia that may be associated with chronic use of Risperidone for Extended-Release Injectable Suspension. Advise them to seek medical attention if they experience any of the following: amenorrhea or galactorrhea in females, erectile dysfunction or gynecomastia in males. [See Warnings and Precautions ( 5.6 )] . Interference with Cognitive and Motor Performance Caution patients about performing activities requiring mental alertness, such as operating hazardous machinery, or operating a motor vehicle, until they are reasonably certain that Risperidone for Extended-Release Injectable Suspension therapy does not affect them adversely [see Warnings and Precautions ( 5.10 )] . Priapism Advise patients of the possibility of painful or prolonged penile erections (priapism). Instruct the patient to seek immediate medical attention in the event of priapism [Warnings and Precautions ( 5.13 )] . Heat Exposure and Dehydration Counsel patients regarding appropriate care in avoiding overheating and dehydration [see Warnings and Precautions ( 5.14 )] . Concomitant Medication Advise patients to inform their healthcare providers if they are taking, or plan to take any prescription or over-the-counter drugs, as there is a potential for interactions [see Drug Interactions ( 7 )] . Alcohol Advise patients to avoid alcohol during treatment with Risperidone for Extended-Release Injectable Suspension [see Drug Interactions ( 7.1 )] . Pregnancy Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with Risperidone for Extended-Release Injectable Suspension. Advise patients that Risperidone for Extended-Release Injectable Suspension may cause extrapyramidal and/or withdrawal symptoms in a neonate. Advise patients that there is a pregnancy registry that monitors pregnancy outcomes in women exposed to Risperidone for Extended-Release Injectable Suspension during pregnancy [see Use in Specific Populations ( 8.1 )] . Lactation Advise breastfeeding women using Risperidone for Extended-Release Injectable Suspension to monitor infants for somnolence, failure to thrive, jitteriness, and extrapyramidal symptoms (tremors and abnormal muscle movements) and to seek medical care if they notice these signs [see Use in Specific Populations ( 8.2 )] . Infertility Advise females of reproductive potential that Risperidone for Extended-Release Injectable Suspension may impair fertility due to an increase in serum prolactin levels. The effects on fertility are reversible [see Use in Specific Populations ( 8.3 )] . Brands listed are the trademarks of their respective owners. Manufactured In Greece By: Pharmathen International S.A. Rodopi, 69300, Greece Manufactured For: Teva Pharmaceuticals Parsippany, NJ 07054 Iss. 3/2023
Instructions for use
Information about safe handling and use of the drug product.INSTRUCTIONS FOR USE Risperidone (ris per’ i done) for Extended-Release Injectable Suspension For deltoid or gluteal intramuscular injection only Each injection should be administered by a healthcare professional. IMPORTANT RESOURCES For additional information call Teva at 1-888-838-2872. Risperidone for Extended-Release Injectable Suspension requires close attention to these step-by-step Instructions for Use to help ensure successful administration. SINGLE-DOSE DEVICE Do not reuse. Medical devices require specific material characteristics to perform as intended. These characteristics have been verified for single-dose only. Any attempt to re-process the device for subsequent re-use may adversely affect the integrity of the device or lead to deterioration in performance. Important Information Use components provided The components in this dose pack are specifically designed for use with Risperidone for Extended-Release Injectable Suspension. Risperidone for Extended-Release Injectable Suspension must be reconstituted only in the diluent supplied in the dose pack. Do not substitute ANY components of the dose pack. Do not store suspension after reconstitution Administer dose as soon as possible after reconstitution to avoid settling. Proper dosing The entire contents of the vial must be administered to ensure intended dose of Risperidone for Extended-Release Injectable Suspension is delivered. Dose pack contents Step 1 Assemble components Take out dose pack Connect vial adapter to vial Wait 30 minutes Remove dose pack from the refrigerator and allow to sit at room temperature for at least 30 minutes before reconstituting. Do not warm any other way. Remove cap from vial Flip off colored cap from vial. Wipe top of the grey stopper with an alcohol swab . Allow to air dry. Do not remove grey rubber stopper. Prepare vial adapter Hold sterile blister as shown. Peel the blister film from backing and remove the vial adapter from its packaging by holding between the white luer cap and the skirt. Do not touch spike tip and luer tip connector of the vial adapter at any time. This will result in contamination. Connect vial adapter to vial Place vial on a hard surface and hold by the base. Center vial adapter over the grey rubber stopper. Push vial adapter straight down onto vial top until it snaps securely into place. CLEAN the luer tip of the vial adapter with an alcohol wipe Do not place vial adapter on at an angle or diluent may leak upon transfer to the vial. Do not shake. Do not touch exposed luer tip connector on vial adapter. This will result in contamination. Connect prefilled syringe to vial adapter Use proper grip Hold by white collar at the tip of the syringe. Do not hold syringe by the glass barrel during assembly. Remove cap Holding the white collar, snap off the white cap. Do not twist or cut off the white cap. Do not touch syringe tip. This will result in contamination. The broken-off cap can be discarded. Connect syringe to vial adapter Hold vial adapter by skirt to keep stationary. Hold syringe by white collar then insert tip into the luer tip connector of the vial adapter. Do not hold the glass syringe barrel. This may cause the white collar to loosen or detach. Attach the syringe to the vial adapter with a firm clockwise twisting motion until it feels snug. Do not over-tighten. Over-tightening may cause the syringe tip to break. Step 2 Reconstitute microspheres Inject diluent Inject entire amount of diluent from syringe into the vial. Suspend microspheres in diluent Continuing to hold down the plunger rod, shake vigorously for at least 10 seconds , as shown. Check the suspension. When properly mixed, the suspension appears uniform, thick and milky in color. Microspheres will be visible in the liquid. Immediately proceed to the next step so suspension does not settle. Transfer suspension to syringe Invert vial completely. Slowly pull plunger rod down to withdraw entire contents from the vial into the syringe. Remove vial adapter Hold white collar on the syringe and unscrew from vial adapter. Tear section of the vial label at the perforation. Apply detached label to the syringe for identification purposes. Discard both vial and vial adapter appropriately. Step 3 Attach needle Select appropriate needle Choose needle based on injection location (gluteal or deltoid). Attach needle Peel blister pouch open part way and use to grasp the base of the needle, as shown. Holding the white collar on the syringe , attach syringe to needle luer connection with a firm clockwise twisting motion until snug. Do not touch needle luer opening. This will result in contamination. Resuspend microspheres Fully remove the blister pouch. Just before injection, shake syringe vigorously again, as some settling will have occurred. Step 4 Inject dose Remove transparent needle protector Move the needle safety device back towards the syringe, as shown. Then hold white collar on syringe and carefully pull the transparent needle protector straight off. Do not twist transparent needle protector, as the luer connection may loosen. Remove air bubbles Hold needle upright and tap gently to make any air bubbles rise to the top. Slowly and carefully press plunger rod upward to remove air. Inject Immediately inject entire contents of syringe intramuscularly (IM) into the gluteal or deltoid muscle of the patient. Gluteal injection should be made into the upper-outer quadrant of the gluteal area. Do not administer intravenously. Secure needle in safety device Using one hand , place needle safety device at a 45-degree angle on a hard, flat surface. Press down with a firm, quick motion until needle is fully engaged in safety device. Avoid needle stick injury: Do not use two hands. Do not intentionally disengage or mishandle the needle safety device. Do not attempt to straighten the needle or engage the safety device if the needle is bent or damaged. Properly dispose of needles Check to confirm needle safety device is fully engaged. Discard in an approved sharps container. Also discard the unused needle provided in the dose pack. Manufactured In Greece By: Pharmathen International S.A. Rodopi, 69300, Greece Manufactured For: Teva Pharmaceuticals Parsippany, NJ 07054 Iss. 3/2023 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES 14.1 Schizophrenia The effectiveness of Risperidone for Extended-Release Injectable Suspension in the treatment of schizophrenia was established, in part, on the basis of extrapolation from the established effectiveness of the oral formulation of risperidone. In addition, the effectiveness of Risperidone for Extended-Release Injectable Suspension in the treatment of schizophrenia was established in a 12-week, placebo-controlled trial in adult psychotic inpatients and outpatients who met the DSM-IV criteria for schizophrenia. Efficacy data were obtained from 400 patients with schizophrenia who were randomized to receive injections of 25 mg, 50 mg, or 75 mg Risperidone for Extended-Release Injectable Suspension or placebo every 2 weeks. During a 1-week run-in period, patients were discontinued from other antipsychotics and were titrated to a dose of 4 mg oral risperidone. Patients who received Risperidone for Extended-Release Injectable Suspension were given doses of oral risperidone (2 mg for patients in the 25 mg group, 4 mg for patients in the 50 mg group, and 6 mg for patients in the 75 mg group) for the 3 weeks after the first injection to provide therapeutic plasma concentrations until the main release phase of risperidone from the injection site had begun. Patients who received placebo injections were given placebo tablets. Efficacy was evaluated using the Positive and Negative Syndrome Scale (PANSS), a validated, multi-item inventory, composed of five subscales to evaluate positive symptoms, negative symptoms, disorganized thoughts, uncontrolled hostility/excitement, and anxiety/depression. The primary efficacy variable in this trial was change from baseline to endpoint in the total PANSS score. The mean total PANSS score at baseline for schizophrenic patients in this study was 81.5. Total PANSS scores showed significant improvement in the change from baseline to endpoint in schizophrenic patients treated with each dose of Risperidone for Extended-Release Injectable Suspension (25 mg, 50 mg, or 75 mg) compared with patients treated with placebo. While there were no statistically significant differences between the treatment effects for the three dose groups, the effect size for the 75 mg dose group was actually numerically less than that observed for the 50 mg dose group. Subgroup analyses did not indicate any differences in treatment outcome as a function of age, race, or gender. 14.2 Bipolar Disorder - Monotherapy The effectiveness of Risperidone for Extended-Release Injectable Suspension for the maintenance treatment of Bipolar I Disorder was established in a multicenter, double-blind, placebo-controlled study of adult patients who met DSM-IV criteria for Bipolar Disorder Type I, who were stable on medications or experiencing an acute manic or mixed episode. A total of 501 patients were treated during a 26-week open-label period with Risperidone for Extended-Release Injectable Suspension (starting dose of 25 mg, and titrated, if deemed clinically desirable, to 37.5 mg or 50 mg; in patients not tolerating the 25 mg dose, the dose could be reduced to 12.5 mg). In the open-label phase, 303 (60%) patients were judged to be stable and were randomized to double-blind treatment with either the same dose of Risperidone for Extended-Release Injectable Suspension or placebo and monitored for relapse. The primary endpoint was time to relapse to any mood episode (depression, mania, hypomania, or mixed). Time to relapse was delayed in patients receiving Risperidone for Extended-Release Injectable Suspension monotherapy as compared to placebo. The majority of relapses were due to manic rather than depressive symptoms. Based on their bipolar disorder history, subjects entering this study had had, on average, more manic episodes than depressive episodes. 14.3 Bipolar Disorder - Adjunctive Therapy The effectiveness of Risperidone for Extended-Release Injectable Suspension as an adjunct to treatment with lithium or valproate for the maintenance treatment of Bipolar Disorder was established in a multi-center, randomized, double-blind, placebo-controlled study of adult patients who met DSM-IV criteria for Bipolar Disorder Type I and who experienced at least 4 episodes of mood disorder requiring psychiatric/clinical intervention in the previous 12 months, including at least 2 episodes in the 6 months prior to the start of the study. A total of 240 patients were treated during a 16-week open-label period with Risperidone for Extended-Release Injectable Suspension (starting dose of 25 mg, and titrated, if deemed clinically desirable, to 37.5 mg or 50 mg), as adjunctive therapy in addition to continuing their treatment as usual for their bipolar disorder, which consisted of mood stabilizers (primarily lithium and valproate), antidepressants, and/or anxiolytics. All oral antipsychotics were discontinued after the first three weeks of the initial Risperidone for Extended-Release Injectable Suspension injection. In the open-label phase, 124 (51.7%) were judged to be stable for at least the last 4 weeks and were randomized to double-blind treatment with either the same dose of Risperidone for Extended-Release Injectable Suspension or placebo in addition to continuing their treatment as usual and monitored for relapse during a 52-week period. The primary endpoint was time to relapse to any new mood episode (depression, mania, hypomania, or mixed). Time to relapse was delayed in patients receiving adjunctive therapy with Risperidone for Extended-Release Injectable Suspension as compared to placebo. The relapse types were about half depressive and half manic or mixed episodes.
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use In an open-label study, 57 clinically stable, elderly patients (≥ 65 years old) with schizophrenia or schizoaffective disorder received Risperidone for Extended-Release Injectable Suspension every 2 weeks for up to 12 months. In general, no differences in the tolerability of Risperidone for Extended-Release Injectable Suspension were observed between otherwise healthy elderly and nonelderly patients. Therefore, dosing recommendations for otherwise healthy elderly patients are the same as for nonelderly patients. Because elderly patients exhibit a greater tendency to orthostatic hypotension than nonelderly patients, elderly patients should be instructed in nonpharmacologic interventions that help to reduce the occurrence of orthostatic hypotension (e.g., sitting on the edge of the bed for several minutes before attempting to stand in the morning and slowly rising from a seated position). In addition, monitoring of orthostatic vital signs should be considered in elderly patients for whom orthostatic hypotension is of concern [see Warnings and Precautions (5.7 )] . Concomitant use with Furosemide in Elderly Patients with Dementia-Related Psychosis In two of four placebo-controlled trials in elderly patients with dementia-related psychosis, a higher incidence of mortality was observed in patients treated with furosemide plus oral risperidone when compared to patients treated with oral risperidone alone or with oral placebo plus furosemide. No pathological mechanism has been identified to explain this finding, and no consistent pattern for cause of death was observed. An increase of mortality in elderly patients with dementia-related psychosis was seen with the use of oral risperidone regardless of concomitant use with furosemide. Risperidone for Extended-Release Injectable Suspension is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions ( 5.1 )].
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use Safety and effectiveness of Risperidone for Extended-Release Injectable Suspension in pediatric patients have not been established. However, juvenile animal toxicology studies have been conducted with oral risperidone. Juvenile Animal Studies Juvenile dogs were treated with oral risperidone from weeks 10 to 50 of age (equivalent to the period of childhood through adolescence in humans), at doses of 0.31, 1.25, or 5 mg/kg/day, which are 1.2, 3.4 and 13.5 times the MRHD of 6 mg/day for children, based on mg/m 2 body surface area. Bone length and density were decreased with a no-effect dose of 0.31 mg/kg/day; this dose produced plasma AUC of risperidone plus its active metabolite paliperidone (9-hydroxy-risperidone) that were similar to those in children and adolescents receiving the MRHD of 6 mg/day. In addition, sexual maturation was delayed at all doses in both males and females. The above effects showed little or no reversibility in females after a 12 week drug-free recovery period. Juvenile rats, treated with oral risperidone from days 12 to 50 of age (equivalent to the period of infancy through adolescence in humans) showed impaired learning and memory performance (reversible only in females), with a no-effect dose of 0.63 mg/kg/day which is 0.5 times the MRHD of 6 mg/day for children, based on mg/m 2 body surface area. This dose produced plasma AUC of risperidone plus paliperidone about half the exposure observed in humans at the MRHD. No other consistent effects on neurobehavioral or reproductive development were seen up to the highest tested dose of 1.25 mg/kg/day which is 1 time the MRHD and produced plasma AUC of risperidone plus paliperidone that were about two thirds of those observed in humans at the MRHD of 6 mg/day for children.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Pregnancy Exposure Registry There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to atypical antipsychotics, including Risperidone for Extended-Release Injectable Suspension, during pregnancy. Healthcare providers are encouraged to register patients by contacting the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or online at http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/ . Risk Summary Neonates exposed to antipsychotic drugs during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery (see Clinical Considerations) . Overall, available data from published epidemiologic studies of pregnant women exposed to risperidone have not established a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data) . There are risks to the mother associated with untreated schizophrenia or bipolar I disorder and with exposure to antipsychotics, including Risperidone for Extended-Release Injectable Suspension, during pregnancy (see Clinical Considerations) . Risperidone has been detected in plasma in adult subjects up to 8 weeks after a single-dose administration of Risperidone for Extended-Release Injectable Suspension [see Clinical Pharmacology ( 12.3 )] . The clinical significance of Risperidone for Extended-Release Injectable Suspension administered before pregnancy or anytime during pregnancy is not known. Oral administration of risperidone to pregnant mice caused cleft palate at doses 3 to 4 times the maximum recommended human dose (MRHD) with maternal toxicity observed at 4-times the MRHD based on mg/m 2 body surface area. Risperidone was not teratogenic in rats or rabbits at doses up to 6-times the MRHD based on mg/m 2 body surface area. Increased stillbirths and decreased birth weight occurred after oral risperidone administration to pregnant rats at 1.5-times the MRHD based on mg/m 2 body surface area. Learning was impaired in offspring of rats when the dams were dosed at 0.6-times the MRHD and offspring mortality increased at doses 0.1 to 3 times the MRHD based on mg/m 2 body surface area. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Clinical Considerations Disease-Associated Maternal and/or Embryo/Fetal Risk There is a risk to the mother from untreated schizophrenia or bipolar I disorder, including increased risk of relapse, hospitalization, and suicide. Schizophrenia and bipolar I disorder are associated with increased adverse perinatal outcomes, including preterm birth. It is not known if this is a direct result of the illness or other comorbid factors. Fetal/Neonatal Adverse Reactions Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, and feeding disorder have been reported in neonates who were exposed to antipsychotic drugs, including Risperidone for Extended-Release Injectable Suspension, during the third trimester of pregnancy. These symptoms have varied in severity. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization. Data Human Data Published data from observational studies, birth registries, and case reports on the use of atypical antipsychotics during pregnancy do not report a clear association with antipsychotics and major birth defects. A prospective observational study including 6 women treated with risperidone demonstrated placental passage of risperidone. A retrospective cohort study from a Medicaid database of 9258 women exposed to antipsychotics during pregnancy did not indicate an overall increased risk for major birth defects. There was a small increase in the risk major of birth defects (RR=1.26, 95% CI 1.02 to 1.56) and of cardiac malformations (RR=1.26, 95% CI 0.88 to 1.81) in a subgroup of 1566 women exposed to risperidone during the first trimester of pregnancy; however, there is no mechanism of action to explain the difference in malformation rates. Animal Data Oral administration of risperidone to pregnant mice during organogenesis caused cleft palate at 10 mg/kg/day which is 3 times the MRHD of 16 mg/day based on mg/m 2 body surface area; maternal toxicity occurred at 4 times the MRHD. Risperidone was not teratogenic when administered orally to rats at 0.6 to 10 mg/kg/day and rabbits at 0.3 to 5 mg/kg/day, which are up to 6 times the MRHD of 16 mg/day risperidone based on mg/m 2 body surface area. Learning was impaired in offspring of rats dosed orally throughout pregnancy at 1 mg/kg/day which is 0.6 times the MRHD and neuronal cell death increased in fetal brains of offspring of rats dosed during pregnancy at 1 and 2 mg/kg/day which are 0.6 and 1.2 times the MRHD based on mg/m 2 body surface area; postnatal development and growth of the offspring were also delayed. Rat offspring mortality increased during the first 4 days of lactation when pregnant rats were dosed throughout gestation at 0.16 to 5 mg/kg/day which are 0.1 to 3 times the MRHD of 16 mg/day based on mg/m 2 body surface area. It is not known whether these deaths were due to a direct effect on the fetuses or pups or to effects on the dams; a no-effect dose could not be determined. The rate of stillbirths was increased at 2.5 mg/kg or 1.5 times the MRHD based on mg/m 2 body surface area. In a rat cross-fostering study the number of live offspring was decreased, the number of stillbirths increased, and the birth weight was decreased in offspring of drug-treated pregnant rats. In addition, the number of deaths increased by Day 1 among offspring of drug-treated pregnant rats, regardless of whether or not the offspring were cross-fostered. Risperidone also appeared to impair maternal behavior in that offspring body weight gain and survival (from Day 1 to 4 of lactation) were reduced in offspring born to control but reared by drug-treated dams. All of these effects occurred at 5 mg/kg which is 3 times the MRHD based on mg/m 2 and the only dose tested in the study.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS Pregnancy: May cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure. ( 8.1 ) Renal or Hepatic Impairment: dose appropriately with oral risperidone prior to initiating treatment with Risperidone for Extended-Release Injectable Suspension. A lower starting dose of Risperidone for Extended-Release Injectable Suspension of 12.5 mg may be appropriate in some patients. ( 2.4 ) Pediatric Use: safety and effectiveness not established in patients less than 18 years of age. ( 8.4 ) Elderly: dosing for otherwise healthy elderly patients is the same as for healthy nonelderly. Elderly may be more predisposed to orthostatic effects than nonelderly. ( 8.5 ) 8.1 Pregnancy Pregnancy Exposure Registry There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to atypical antipsychotics, including Risperidone for Extended-Release Injectable Suspension, during pregnancy. Healthcare providers are encouraged to register patients by contacting the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or online at http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/ . Risk Summary Neonates exposed to antipsychotic drugs during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery (see Clinical Considerations) . Overall, available data from published epidemiologic studies of pregnant women exposed to risperidone have not established a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data) . There are risks to the mother associated with untreated schizophrenia or bipolar I disorder and with exposure to antipsychotics, including Risperidone for Extended-Release Injectable Suspension, during pregnancy (see Clinical Considerations) . Risperidone has been detected in plasma in adult subjects up to 8 weeks after a single-dose administration of Risperidone for Extended-Release Injectable Suspension [see Clinical Pharmacology ( 12.3 )] . The clinical significance of Risperidone for Extended-Release Injectable Suspension administered before pregnancy or anytime during pregnancy is not known. Oral administration of risperidone to pregnant mice caused cleft palate at doses 3 to 4 times the maximum recommended human dose (MRHD) with maternal toxicity observed at 4-times the MRHD based on mg/m 2 body surface area. Risperidone was not teratogenic in rats or rabbits at doses up to 6-times the MRHD based on mg/m 2 body surface area. Increased stillbirths and decreased birth weight occurred after oral risperidone administration to pregnant rats at 1.5-times the MRHD based on mg/m 2 body surface area. Learning was impaired in offspring of rats when the dams were dosed at 0.6-times the MRHD and offspring mortality increased at doses 0.1 to 3 times the MRHD based on mg/m 2 body surface area. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Clinical Considerations Disease-Associated Maternal and/or Embryo/Fetal Risk There is a risk to the mother from untreated schizophrenia or bipolar I disorder, including increased risk of relapse, hospitalization, and suicide. Schizophrenia and bipolar I disorder are associated with increased adverse perinatal outcomes, including preterm birth. It is not known if this is a direct result of the illness or other comorbid factors. Fetal/Neonatal Adverse Reactions Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress, and feeding disorder have been reported in neonates who were exposed to antipsychotic drugs, including Risperidone for Extended-Release Injectable Suspension, during the third trimester of pregnancy. These symptoms have varied in severity. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately. Some neonates recovered within hours or days without specific treatment; others required prolonged hospitalization. Data Human Data Published data from observational studies, birth registries, and case reports on the use of atypical antipsychotics during pregnancy do not report a clear association with antipsychotics and major birth defects. A prospective observational study including 6 women treated with risperidone demonstrated placental passage of risperidone. A retrospective cohort study from a Medicaid database of 9258 women exposed to antipsychotics during pregnancy did not indicate an overall increased risk for major birth defects. There was a small increase in the risk major of birth defects (RR=1.26, 95% CI 1.02 to 1.56) and of cardiac malformations (RR=1.26, 95% CI 0.88 to 1.81) in a subgroup of 1566 women exposed to risperidone during the first trimester of pregnancy; however, there is no mechanism of action to explain the difference in malformation rates. Animal Data Oral administration of risperidone to pregnant mice during organogenesis caused cleft palate at 10 mg/kg/day which is 3 times the MRHD of 16 mg/day based on mg/m 2 body surface area; maternal toxicity occurred at 4 times the MRHD. Risperidone was not teratogenic when administered orally to rats at 0.6 to 10 mg/kg/day and rabbits at 0.3 to 5 mg/kg/day, which are up to 6 times the MRHD of 16 mg/day risperidone based on mg/m 2 body surface area. Learning was impaired in offspring of rats dosed orally throughout pregnancy at 1 mg/kg/day which is 0.6 times the MRHD and neuronal cell death increased in fetal brains of offspring of rats dosed during pregnancy at 1 and 2 mg/kg/day which are 0.6 and 1.2 times the MRHD based on mg/m 2 body surface area; postnatal development and growth of the offspring were also delayed. Rat offspring mortality increased during the first 4 days of lactation when pregnant rats were dosed throughout gestation at 0.16 to 5 mg/kg/day which are 0.1 to 3 times the MRHD of 16 mg/day based on mg/m 2 body surface area. It is not known whether these deaths were due to a direct effect on the fetuses or pups or to effects on the dams; a no-effect dose could not be determined. The rate of stillbirths was increased at 2.5 mg/kg or 1.5 times the MRHD based on mg/m 2 body surface area. In a rat cross-fostering study the number of live offspring was decreased, the number of stillbirths increased, and the birth weight was decreased in offspring of drug-treated pregnant rats. In addition, the number of deaths increased by Day 1 among offspring of drug-treated pregnant rats, regardless of whether or not the offspring were cross-fostered. Risperidone also appeared to impair maternal behavior in that offspring body weight gain and survival (from Day 1 to 4 of lactation) were reduced in offspring born to control but reared by drug-treated dams. All of these effects occurred at 5 mg/kg which is 3 times the MRHD based on mg/m 2 and the only dose tested in the study. 8.2 Lactation Risk Summary Limited data from published literature reports the presence of risperidone and its metabolite, 9-hydroxyrisperidone, in human breast milk at relative infant dose ranging between 2.3% and 4.7% of the maternal weight-adjusted dosage. There are reports of sedation, failure to thrive, jitteriness, and extrapyramidal symptoms (tremors and abnormal muscle movements) in breastfed infants exposed to risperidone (see Clinical Considerations) . Risperidone has been detected in plasma in adult subjects up to 8 weeks after a single-dose administration of Risperidone for Extended-Release Injectable Suspension [see Clinical Pharmacology ( 12.3 )] , and the clinical significance on the breastfed infant is not known. There is no information on the effects of risperidone on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for Risperidone for Extended-Release Injectable Suspension and any potential adverse effects on the breastfed child from Risperidone for Extended-Release Injectable Suspension or from the mother’s underlying condition. Clinical Considerations Infants exposed to Risperidone for Extended-Release Injectable Suspension through breastmilk should be monitored for excess sedation, failure to thrive, jitteriness, and extrapyramidal symptoms (tremors and abnormal muscle movements). 8.3 Females and Males of Reproductive Potential Infertility Females Based on the pharmacologic action of risperidone (D2 receptor antagonism), treatment with Risperidone for Extended-Release Injectable Suspension may result in an increase in serum prolactin levels, which may lead to a reversible reduction in fertility in females of reproductive potential [see Warnings and Precautions ( 5.6 )] . 8.4 Pediatric Use Safety and effectiveness of Risperidone for Extended-Release Injectable Suspension in pediatric patients have not been established. However, juvenile animal toxicology studies have been conducted with oral risperidone. Juvenile Animal Studies Juvenile dogs were treated with oral risperidone from weeks 10 to 50 of age (equivalent to the period of childhood through adolescence in humans), at doses of 0.31, 1.25, or 5 mg/kg/day, which are 1.2, 3.4 and 13.5 times the MRHD of 6 mg/day for children, based on mg/m 2 body surface area. Bone length and density were decreased with a no-effect dose of 0.31 mg/kg/day; this dose produced plasma AUC of risperidone plus its active metabolite paliperidone (9-hydroxy-risperidone) that were similar to those in children and adolescents receiving the MRHD of 6 mg/day. In addition, sexual maturation was delayed at all doses in both males and females. The above effects showed little or no reversibility in females after a 12 week drug-free recovery period. Juvenile rats, treated with oral risperidone from days 12 to 50 of age (equivalent to the period of infancy through adolescence in humans) showed impaired learning and memory performance (reversible only in females), with a no-effect dose of 0.63 mg/kg/day which is 0.5 times the MRHD of 6 mg/day for children, based on mg/m 2 body surface area. This dose produced plasma AUC of risperidone plus paliperidone about half the exposure observed in humans at the MRHD. No other consistent effects on neurobehavioral or reproductive development were seen up to the highest tested dose of 1.25 mg/kg/day which is 1 time the MRHD and produced plasma AUC of risperidone plus paliperidone that were about two thirds of those observed in humans at the MRHD of 6 mg/day for children. 8.5 Geriatric Use In an open-label study, 57 clinically stable, elderly patients (≥ 65 years old) with schizophrenia or schizoaffective disorder received Risperidone for Extended-Release Injectable Suspension every 2 weeks for up to 12 months. In general, no differences in the tolerability of Risperidone for Extended-Release Injectable Suspension were observed between otherwise healthy elderly and nonelderly patients. Therefore, dosing recommendations for otherwise healthy elderly patients are the same as for nonelderly patients. Because elderly patients exhibit a greater tendency to orthostatic hypotension than nonelderly patients, elderly patients should be instructed in nonpharmacologic interventions that help to reduce the occurrence of orthostatic hypotension (e.g., sitting on the edge of the bed for several minutes before attempting to stand in the morning and slowly rising from a seated position). In addition, monitoring of orthostatic vital signs should be considered in elderly patients for whom orthostatic hypotension is of concern [see Warnings and Precautions (5.7 )] . Concomitant use with Furosemide in Elderly Patients with Dementia-Related Psychosis In two of four placebo-controlled trials in elderly patients with dementia-related psychosis, a higher incidence of mortality was observed in patients treated with furosemide plus oral risperidone when compared to patients treated with oral risperidone alone or with oral placebo plus furosemide. No pathological mechanism has been identified to explain this finding, and no consistent pattern for cause of death was observed. An increase of mortality in elderly patients with dementia-related psychosis was seen with the use of oral risperidone regardless of concomitant use with furosemide. Risperidone for Extended-Release Injectable Suspension is not approved for the treatment of patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions ( 5.1 )]. 8.6 Renal or Hepatic Impairment In patients with renal or hepatic impairment, carefully titrate with oral risperidone prior to initiating treatment with Risperidone for Extended-Release Injectable Suspension [see Dosage and Administration (2.4)] . Patients with renal impairment may have less ability to eliminate risperidone than patients with normal renal function. Patients with impaired hepatic function may have an increase in the free fraction of risperidone, possibly resulting in an enhanced effect [see Clinical Pharmacology (12.3)] . 8.7 Patients with Parkinson’s Disease or Lewy Body Dementia Patients with Parkinson’s Disease or Dementia with Lewy Bodies can experience increased sensitivity to Risperidone for Extended-Release Injectable Suspension. Manifestations can include confusion, obtundation, postural instability with frequent falls, extrapyramidal symptoms, and clinical features consistent with neuroleptic malignant syndrome.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING Risperidone for Extended-Release Injectable Suspension is available in dosage strengths of 12.5 mg, 25 mg, 37.5 mg, or 50 mg risperidone. It is provided as a single-dose pack, consisting of a vial containing the risperidone microspheres, a pre-filled syringe containing 2 mL of diluent for Risperidone for Extended-Release Injectable Suspension, a vial adapter, and two Terumo SurGuard ® 3 Needles for intramuscular injection (a 21 G UTW 1-inch needle with needle protection device for deltoid administration and a 20 G TW 2-inch needle with needle protection device for gluteal administration). 12.5 mg vial/kit (NDC 0480-1554-08): 43 mg (equivalent to 12.5 mg of risperidone) of a white to off-white powder provided in a vial with a violet flip-off cap (NDC 0480-9732-01). 25 mg vial/kit (NDC 0480-1232-08): 81 mg (equivalent to 25 mg of risperidone) of a white to off-white powder provided in a vial with a pink flip-off cap (NDC 0480-9733-01). 37.5 mg vial/kit (NDC 0480-1342-08): 120 mg (equivalent to 37.5 mg of risperidone) of a white to off-white powder provided in a vial with a green flip-off cap (NDC 0480-9734-01). 50 mg vial/kit (NDC 0480-1453-08): 156 mg (equivalent to 50 mg of risperidone) of a white to off-white powder provided in a vial with a blue flip-off cap (NDC 0480-9735-01). Storage and Handling The entire dose pack should be stored in the refrigerator (36° to 46°F; 2° to 8°C) and protected from light. If refrigeration is unavailable, Risperidone for Extended-Release Injectable Suspension can be stored at temperatures not exceeding 77°F (25°C) for no more than 7 days prior to administration. Do not expose unrefrigerated product to temperatures above 77°F (25°C). Keep out of reach of children.
Boxed warning
Information about contraindications or serious warnings, particularly those that may lead to death or serious injury.WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Risperidone for Extended-Release Injectable Suspension is not approved for the treatment of patients with dementia-related psychosis [see Warnings and Precautions ( 5.1 )]. WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS See full prescribing information for complete boxed warning. Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Risperidone for Extended-Release Injectable Suspension is not approved for use in patients with dementia-related psychosis. ( 5.1 )
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API