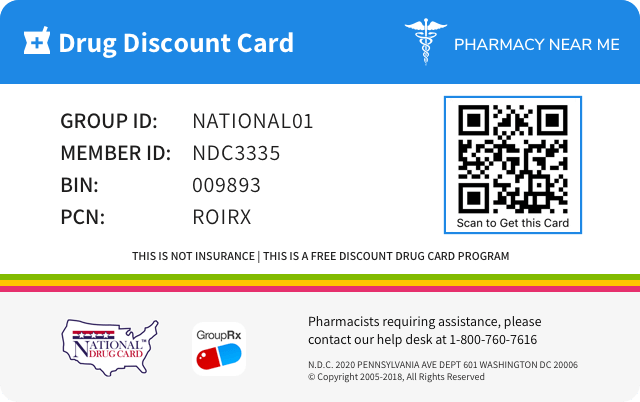
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 80425-0328 | ||||
|---|---|---|---|---|---|
| Drug Name | Dexamethasone |
||||
| Type | Generic | ||||
| Pharm Class | Corticosteroid Hormone Receptor Agonists [MoA], Corticosteroid [EPC] |
||||
| Active Ingredients |
|
||||
| Route | ORAL | ||||
| Dosage Form | TABLET | ||||
| RxCUI drug identifier | 197582 | ||||
| Application Number | ANDA088481 | ||||
| Labeler Name | Advanced Rx Pharmacy of Tennessee, LLC | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Overdosage of Dexamethasone
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.Treatment of overdosage is by supportive and symptomatic therapy. In the case of acute overdosage, according to the patient's condition, supportive therapy may include gastric lavage or emesis.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.(listed alphabetically, under each subsection) The following adverse reactions have been reported with dexamethasone or other corticosteroids: Allergic Reactions: Anaphylactoid reaction, anaphylaxis, angioedema. Cardiovascular: Bradycardia, cardiac arrest, cardiac arrhythmias, cardiac enlargement, circulatory collapse, congestive heart failure, fat embolism, hypertension, hypertrophic cardiomyopathy in premature infants, myocardial rupture following recent myocardial infarction (see WARNINGS:Cardio-renal), edema, pulmonary edema, syncope, tachycardia, thromboembolism, thrombophlebitis, vasculitis. Dermatologic: Acne, allergic dermatitis, dry scaly skin, ecchymoses and petechiae, erythema, impaired wound healing, increased sweating, rash, striae, suppression of reactions to skin tests, thin fragile skin, thinning scalp hair, urticaria. Endocrine: Decreased carbohydrate and glucose tolerance, development of cushingoid state, hyperglycemia, glycosuria, hirsutism, hypertrichosis, increased requirements for insulin or oral hypoglycemic agents in diabetes, manifestations of latent diabetes mellitus, menstrual irregularities, secondary adrenocortical and pituitary unresponsiveness (particularly in times of stress, as in trauma, surgery, or illness), suppression of growth in pediatric patients. Fluid and Electrolyte Disturbances: Congestive heart failure in susceptible patients, fluid retention, hypokalemic alkalosis, potassium loss, sodium retention, tumor lysis syndrome. Gastrointestinal: Abdominal distention, elevation in serum liver enzyme levels (usually reversible upon discontinuation), hepatomegaly, increased appetite, nausea, pancreatitis, peptic ulcer with possible perforation and hemorrhage, perforation of the small and large intestine (particularly in patients with inflammatory bowel disease), ulcerative esophagitis. Metabolic: Negative nitrogen balance due to protein catabolism. Musculoskeletal: Aseptic necrosis of femoral and humeral heads, loss of muscle mass, muscle weakness, osteoporosis, pathologic fracture of long bones, steroid myopathy, tendon rupture, vertebral compression fractures. Neurological/Psychiatric: Convulsions, depression, emotional instability, euphoria, headache, increased intracranial pressure with papilledema (pseudotumor cerebri) usually following discontinuation of treatment, insomnia, mood swings, neuritis, neuropathy, paresthesia, personality changes, psychic disorders, vertigo. Ophthalmic: Exophthalmos, glaucoma, increased intraocular pressure, posterior subcapsular cataracts, vision blurred. Other: Abnormal fat deposits, decreased resistance to infection, hiccups, increased or decreased motility and number of spermatozoa, malaise, moon face, weight gain. To report SUSPECTED ADVERSE REACTIONS, contact Alvogen, Inc. at 1-866-770-3024 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch for voluntary reporting of adverse reactions.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.Glucocorticoids, naturally occurring and synthetic, are adrenocortical steroids that are readily absorbed from the gastrointestinal tract. Glucocorticoids cause varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli. Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have sodium-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs including dexamethasone are primarily used for their anti-inflammatory effects in disorders of many organ systems. At equipotent anti-inflammatory doses, dexamethasone almost completely lacks the sodium-retaining property of hydrocortisone and closely related derivatives of hydrocortisone.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.Systemic fungal infections (see WARNINGS: Fungal Infections). Dexamethasone tablets are contraindicated in patients who are hypersensitive to any components of this product.
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.Dexamethasone Tablets 0.5 mg, 0.75 mg, 4 mg and 6 mg are for oral administration. Each tablet contains 0.5 mg, 0.75 mg, 4 mg or 6 mg of dexamethasone. Dexamethasone, a synthetic adrenocortical steroid, is a white to practically white, odorless, crystalline powder. It is stable in air. It is practically insoluble in water. It is designated chemically as 9-fluoro-11β, 17, 21-trihydroxy-16α-methylpregna-1,4-diene-3,20-dione. The structural formula is represented below: C22H29FO5 MW 392.47 Each tablet contains anhydrous lactose, croscarmellose sodium, magnesium stearate, microcrystalline cellulose and stearic acid. In addition, the 0.5 mg tablet contains D&C Yellow #10. The 0.75 mg tablet contains D&C Yellow #10 and FD&C Blue #1. Description
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.For Oral Administration: The initial dose varies from 0.75 to 9 mg a day depending on the disease being treated. IT SHOULD BE EMPHASIZED THAT DOSAGE REQUIREMENTS ARE VARIABLE AND MUST BE INDIVIDUALIZED ON THE BASIS OF THE DISEASE UNDER TREATMENT AND THE RESPONSE OF THE PATIENT. After a favorable response is noted, the proper maintenance dosage should be determined by decreasing the initial dosage in small decrements at appropriate time intervals until the lowest dosage that maintains an adequate clinical response is reached. Situations which may make dosage adjustments necessary are changes in clinical status secondary to remissions or exacerbations in the disease process, the patient's individual drug responsiveness, and the effect of patient exposure to stressful situations not directly related to the disease entity under treatment. In this latter situation it may be necessary to increase the dosage of the corticosteroid for a period of time consistent with the patient's condition. If after long-term therapy the drug is to be stopped, it is recommended that it be withdrawn gradually rather than abruptly. In the treatment of acute exacerbations of multiple sclerosis, daily doses of 30 mg of dexamethasone for a week followed by 4 to 12 mg every other day for one month have been shown to be effective (see PRECAUTIONS:Neuro-Psychiatric). In pediatric patients, the initial dose of dexamethasone may vary depending on the specific disease entity being treated. The range of initial doses is 0.02 to 0.3 mg/kg/day in three or four divided doses (0.6 to 9 mg/m2bsa/day). For the purpose of comparison, the following is the equivalent milligram dosage of the various corticosteroids: Cortisone, 25 Hydrocortisone, 20 Prednisolone, 5 Prednisone, 5 Methylprednisolone, 4 Triamcinolone, 4 Paramethasone, 2 Betamethasone, 0.75 Dexamethasone, 0.75 These dose relationships apply only to oral or intravenous administration of these compounds. When these substances or their derivatives are injected intramuscularly or into joint spaces, their relative properties may be greatly altered. In acute, self-limited allergic disorders or acute exacerbations of chronic allergic disorders, the following dosage schedule combining parenteral and oral therapy is suggested: Dexamethasone Sodium Phosphate injection, 4 mg per mL: First Day 1 or 2 mL, intramuscularly Dexamethasone tablets, 0.75 mg: Second Day 4 tablets in two divided doses Third Day 4 tablets in two divided doses Fourth Day 2 tablets in two divided doses Fifth Day 1 tablet Sixth Day 1 tablet Seventh Day No treatment Eighth Day Follow-up visit This schedule is designed to ensure adequate therapy during acute episodes, while minimizing the risk of overdosage in chronic cases. In cerebral edema, dexamethasone sodium phosphate injection is generally administered initially in a dosage of 10 mg intravenously followed by 4 mg every six hours intramuscularly until the symptoms of cerebral edema subside. Response is usually noted within 12 to 24 hours and dosage may be reduced after two to four days and gradually discontinued over a period of five to seven days. For palliative management of patients with recurrent or inoperable brain tumors, maintenance therapy with either dexamethasone sodium phosphate injection or dexamethasone tablets in a dosage of 2 mg two or three times daily may be effective. Dexamethasone Suppression Tests 1. Tests for Cushing’s syndrome Give 1.0 mg of dexamethasone orally at 11:00 p.m. Blood is drawn for plasma cortisol determination at 8:00 a.m. the following morning. For greater accuracy, give 0.5 mg of dexamethasone orally every 6 hours for 48 hours. Twenty-four hour urine collections are made for determination of 17-hydroxycorticosteroid excretion. 2. Test to distinguish Cushing’s syndrome due to pituitary ACTH excess from Cushing’s syndrome due to other causes. Give 2.0 mg of dexamethasone orally every 6 hours for 48 hours. Twenty-four hour urine collections are made for determination of 17-hydroxycorticosteroid excretion.
| Cortisone, 25 Hydrocortisone, 20 Prednisolone, 5 Prednisone, 5 Methylprednisolone, 4 | Triamcinolone, 4 Paramethasone, 2 Betamethasone, 0.75 Dexamethasone, 0.75 |
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.Allergic States Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in asthma, atopic dermatitis, contact dermatitis, drug hypersensitivity reactions, seasonal or perennial allergic rhinitis and serum sickness. Dermatologic Diseases Bullous dermatitis herpetiformis, exfoliative erythroderma, mycosis fungoides, pemphigus, and severe erythema multiforme (Stevens-Johnson syndrome). Endocrine Disorders Primary or secondary adrenocortical insufficiency (hydrocortisone or cortisone is the drug of choice; may be used in conjunction with synthetic mineralocorticoid analogs where applicable; in infancy mineralocorticoid supplementation is of particular importance), congenital adrenal hyperplasia, hypercalcemia associated with cancer, and nonsuppurative thyroiditis. Gastrointestinal Diseases To tide the patient over a critical period of the disease in regional enteritis and ulcerative colitis. Hematologic Disorders Acquired (autoimmune) hemolytic anemia, congenital (erythroid) hypoplastic anemia (Diamond-Blackfan anemia), idiopathic thrombocytopenic purpura in adults, pure red cell aplasia, and selected cases of secondary thrombocytopenia. Miscellaneous Diagnostic testing of adrenocortical hyperfunction, trichinosis with neurologic or myocardial involvement, tuberculous meningitis with subarachnoid block or impending block when used with appropriate antituberculous chemotherapy. Neoplastic Diseases For palliative management of leukemias and lymphomas. Nervous System Acute exacerbations of multiple sclerosis, cerebral edema associated with primary or metastatic brain tumor, craniotomy, or head injury. Ophthalmic Diseases Sympathetic ophthalmia, temporal arteritis, uveitis, and ocular inflammatory conditions unresponsive to topical corticosteroids. Renal Diseases To induce a diuresis or remission of proteinuria in idiopathic nephrotic syndrome or that due to lupus erythematosus. Respiratory Diseases Berylliosis, fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate antituberculous chemotherapy, idiopathic eosinophilic pneumonias, symptomatic sarcoidosis. Rheumatic Disorders As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in acute gouty arthritis, acute rheumatic carditis, ankylosing spondylitis, psoriatic arthritis, rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low-dose maintenance therapy). For the treatment of dermatomyositis, polymyositis, and systemic lupus erythematosus.
Spl product data elements
Usually a list of ingredients in a drug product.Dexamethasone Dexamethasone DEXAMETHASONE DEXAMETHASONE F;087
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.label 1
Spl unclassified section
Information not classified as belonging to one of the other fields. Approximately 40% of labeling with effective_time between June 2009 and August 2014 have information in this field.Rx Only
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.How Supplied/Storage and Handling Dexamethasone tablets are available as: 4 mg tablets scored (white), debossed “F 087” and supplied in: Bottles of 12 NDC: 80425-0328-01 Store at 20°C to 25°C (68°F to 77°F) [See USP Controlled Room Temperature]. Dispense in a tight, light resistant container as defined in the USP/NF. Product of USA Distributed by: Alvogen, Inc. Morristown, NJ 07960 USA PI905-00 Revised: June 2021
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API