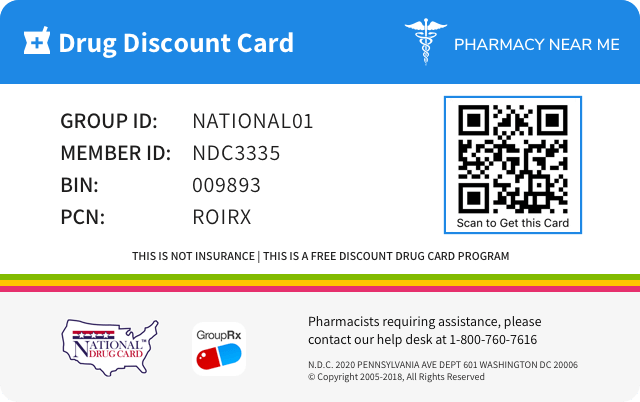
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 0003-5200 | ||||
|---|---|---|---|---|---|
| Drug Name | Cobenfy |
||||
| Type | Brand | ||||
| Dosage Form | KIT | ||||
| RxCUI drug identifier | 2694843, 2694850, 2694853, 2694855, 2694989, 2694991, 2694992, 2694993, 2695671, 2695672 |
||||
| Application Number | NDA216158 | ||||
| Labeler Name | E.R. Squibb & Sons, L.L.C. | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Overdosage of Cobenfy
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE Overdose of COBENFY may produce cholinergic, anticholinergic or a combination of cholinergic and anticholinergic signs and symptoms: • Cholinergic Signs and Symptoms: seizures, vomiting, diarrhea, abdominal pain, hyperhidrosis, salivary hypersecretion, and hypotension possibly preceded by hypertension. • Anticholinergic Signs and Symptoms (geriatric patients may be more susceptible): delirium, agitation, garbled speech, dizziness, hypertension, tachycardia, dry mouth and eyes, ileus, blurred vision, and urinary retention. Consider calling the Poison Help Line 1-800-222-1222 or a medical toxicologist for specific treatment recommendations.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS The following clinically significant adverse reactions are described elsewhere in the labeling: • Risk of Urinary Retention [see Warnings and Precautions (5.1) ] • Risk of Use in Patients with Hepatic Impairment [see Warnings and Precautions (5.2) ] • Risk of Use in Patients with Biliary Disease [see Warnings and Precautions (5.3) ] • Decreased Gastrointestinal Motility [see Warnings and Precautions (5.4) ] • Risk of Angioedema [see Warnings and Precautions (5.5) ] • Risk of Use in Patients with Narrow-angle Glaucoma [see Warnings and Precautions (5.6) ] • Increases in Heart Rate [see Warnings and Precautions (5.7) ] • Anticholinergic Adverse Reactions in Patients with Renal Impairment [see Warnings and Precautions (5.8) ] • Central Nervous System Effects [see Warnings and Precautions (5.9) ] Most common adverse reactions (incidence ≥ 5% and at least twice placebo) were nausea, dyspepsia, constipation, vomiting, hypertension, abdominal pain, diarrhea, tachycardia, dizziness, and gastrointestinal reflux disease. ( 6.1 ) To report SUSPECTED ADVERSE REACTIONS, contact Bristol Myers-Squibb at 1-800-721-5072 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. COBENFY was evaluated for safety in a total of 1,594 subjects exposed to one or more doses, including 1,135 adult patients with schizophrenia and 389 healthy subjects. A total of 347 COBENFY-treated patients had at least 6 months of exposure and 150 patients had at least 1 year of exposure (defined as ≥ 50 weeks) from open-label studies. The adverse reaction findings are based on two pooled 5-week, placebo-controlled, flexible-dose studies in 504 adult patients with schizophrenia in which COBENFY or placebo was started at an initial dose of 50 mg/20 mg twice daily for the first 2 days followed by 100 mg/20 mg twice daily for the remainder of Week 1 (Days 3 to 7). On Day 8, dosing was titrated to 125 mg/30 mg twice daily unless the patient could not tolerate it. All patients had the option to return to 100 mg/20 mg twice daily for the remainder of the treatment period [see Clinical Studies (14) ] . In the 5-week placebo-controlled studies, 6% of patients treated with COBENFY and 4% of placebo-treated patients discontinued participation due to adverse reactions. Adverse reactions that led to study discontinuation in ≥1% of patients treated with COBENFY include nausea (2%) and vomiting (1%). The most common adverse reactions (≥5% and at least twice placebo) were nausea, dyspepsia, constipation, vomiting, hypertension, abdominal pain, diarrhea, tachycardia, dizziness, and gastroesophageal reflux disease. Adverse reactions reported with COBENFY at an incidence of at least 2% in patients exposed to COBENFY and greater than the rate of placebo are shown in Table 1. Table 1: Adverse Reactions Reported in ≥2% of COBENFY-Treated Patients and Greater than Rate of Placebo in Two 5-week Schizophrenia Trials a Dyspepsia includes dyspepsia, esophageal discomfort b Hypertension includes hypertension, blood pressure increased, labile hypertension, orthostatic hypertension c Abdominal Pain includes abdominal discomfort, abdominal pain upper, abdominal pain, abdominal pain lower, abdominal tenderness d Tachycardia includes tachycardia, heart rate increased, sinus tachycardia e Cough: includes cough, productive cough f EPS (non-akathisia) includes dyskinesia, drooling, dystonia, extrapyramidal disorder, muscle contraction involuntary, muscle spasms COBENFY (N=251) Placebo (N=253) Nausea 19% 4% Dyspepsia a 18% 5% Constipation 17% 7% Vomiting 15% 1% Hypertension b 11% 2% Abdominal Pain c 8% 4% Diarrhea 6% 2% Tachycardia d 5% 2% Dizziness 5% 2% Gastroesophageal reflux disease 5% <1% Dry mouth 4% 2% Somnolence 3% 2% Vision blurred 3% 0% Salivary hypersecretion 2% 0% Orthostatic hypotension 2% 1% Cough e 2% 1% Extrapyramidal symptoms (EPS), non-akathisia f 2% <1% Increases in Heart Rate In a dedicated 8-week clinical study, 24-hour ambulatory blood pressure monitoring (ABPM) was conducted in 133 patients with schizophrenia. A total of 95 patients had acceptable ABPM recordings at both baseline and Week 8. In that group, there was a mean change in 24-hour heart rate of 9.8 beats per minute (bpm) (95% CI 7.5, 12.2) from baseline to Week 8. In the two placebo-controlled schizophrenia studies, COBENFY was associated with increases in heart rate compared to placebo, with peak elevation occurring on Day 8 of study treatment (13.5 bpm in the COBENFY group and 4.0 bpm in the placebo group), partially attenuating with continued dosing (11.4 bpm in the COBENFY group and 5.5 bpm in the placebo group at Week 5). Liver Enzyme Elevations In the 5-week, placebo-controlled schizophrenia studies, the proportions of patients with ALT or AST elevations of ≥3 times the upper limits of the normal reference range were 2.8% (6/214) for COBENFY-treated patients compared to 0.4% (1/224) of placebo-treated patients. Twenty-five (1.6%) of the total 1,594 subjects exposed to COBENFY had elevated liver enzymes. The majority of liver enzyme elevations occurred within the first month of treatment and resolved with continued COBENFY use, suggestive of liver adaptation; some cases required treatment interruption, and one was associated with an increase in bilirubin. Urinary Retention In the 5-week, placebo-controlled studies, urinary retention (urinary hesitation, dysuria, and urinary retention) was reported in 0.8% of COBENFY-treated patients and 0.4% on placebo. In the long-term, open-label studies, urinary retention was reported in 3.5% of COBENFY-treated patients. Urinary retention was more common in males, geriatric patients, and those with certain risk factors [see Warnings and Precautions (5.1) ] . Urinary retention occurred at all doses but was predominately observed at the maximum COBENFY dose. In the long-term, open-label studies, urinary tract infections were reported in 2.3% of COBENFY-treated patients and were more commonly reported in females than males. Of the total 1,594 subjects exposed to COBENFY (including healthy volunteers and patients with schizophrenia or other conditions), four subjects required a Foley catheter, including one with elevated serum creatinine and one with urinary tract infections. Four subjects with urinary retention required reduction of COBENFY dose, four discontinued COBENFY, and four received medications for the treatment of benign prostatic hyperplasia (BPH). 6.2 Postmarketing Experience The following adverse reactions have been identified during post-approval use of trospium chloride, one of the components of COBENFY. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. • Cardiovascular – chest pain, hypertensive crisis, palpitations, supraventricular tachycardia, syncope • Gastrointestinal – gastritis • General – rash • Musculoskeletal – rhabdomyolysis • Nervous System – confusion, delirium, dizziness, hallucinations, somnolence, vision abnormal • Skin and subcutaneous tissue disorders – angioedema, anaphylactic reaction, Stevens-Johnson syndrome
| a Dyspepsia includes | ||
| b Hypertension includes hypertension, blood pressure increased, labile hypertension, orthostatic hypertension | ||
| c Abdominal Pain includes | ||
| d Tachycardia includes | ||
| e Cough: includes cough, productive cough | ||
| f EPS (non-akathisia) includes dyskinesia, drooling, dystonia, extrapyramidal disorder, muscle contraction involuntary, muscle spasms | ||
Cobenfy Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS • Drugs Eliminated by Active Tubular Secretion: Monitor for increased frequency and/or severity of adverse reactions related to COBENFY and to drugs eliminated by active tubular secretion. ( 7.1 ) • Strong CYP2D6 Inhibitors: Monitor for increased frequency and/or severity of COBENFY-related adverse reactions. ( 7.1 ) • Sensitive Substrates of CYP3A4 or P-glycoprotein: Monitor for increased frequency and/or severity of adverse reactions from these substrates. ( 7.1 ) • Antimuscarinic Drugs: Monitor for increased frequency or severity of anticholinergic adverse reactions. ( 7.2 ) 7.1 Clinically Significant Drug Interactions with COBENFY Table 2 displays clinically significant drug interactions with COBENFY. Table 2: Clinically Significant Drug Interactions with COBENFY Strong Inhibitors of CYP2D6 Clinical Implication: CYP2D6 contributes significantly to the metabolism of xanomeline, a component of COBENFY. Concomitant use of COBENFY with strong CYP2D6 inhibitors may increase plasma concentrations of xanomeline, which may increase the frequency and/or severity of adverse reactions from COBENFY [see Clinical Pharmacology (12.3)] . Prevention or Management: Monitor patients for increased frequency and/or severity of adverse reactions related to COBENFY in patients taking COBENFY with strong inhibitors of CYP2D6. Drugs Eliminated by Active Tubular Secretion Clinical Implication: Concomitant use of COBENFY with drugs that are eliminated by active tubular secretion may increase plasma concentrations of trospium a component of COBENFY, and/or the concomitantly used drug due to competition for this elimination pathway, which may increase the frequency and/or severity of adverse reactions from COBENFY or the drug eliminated by active tubular secretion [see Clinical Pharmacology (12.3)] . Prevention or Management: Monitor patients for increased frequency and/or severity of adverse reactions related to COBENFY and adverse reactions related to drugs eliminated by active tubular secretion in patients concomitantly receiving such drugs. Oral Drugs That Are Sensitive Substrates of CYP3A4 Clinical Implication: Xanomeline, a component of COBENFY, transiently inhibits CYP3A4 locally in the gut but not systemically. Concomitant use of COBENFY with oral drugs that are sensitive substrates of CYP3A4 may result in increased plasma concentrations of the oral drugs that are sensitive substrates of CYP3A4. This may increase the frequency and/or severity of adverse reactions from such substrates [see Clinical Pharmacology (12.3)] . Prevention or Management: Monitor patients for increased frequency and/or severity of adverse reactions related to oral drugs that are sensitive substrates of CYP3A4 in patients taking COBENFY with such substrates. Oral Drugs That Are Substrates of P-glycoprotein Clinical Implication: Xanomeline, a component of COBENFY, transiently inhibits P-glycoprotein locally in the gut but not systemically. Concomitant use of COBENFY with oral drugs that are substrates of P-glycoprotein may result in increased plasma concentrations of the oral drugs that are substrates of P-glycoprotein, which may increase the frequency and/or severity of adverse reactions from such substrates [see Clinical Pharmacology (12.3)] . Prevention or Management: Monitor patients for increased frequency and/or severity of adverse reactions related to oral drugs that are narrow therapeutic index substrates of P-glycoprotein in patients taking COBENFY with such substrates. 7.2 Other Antimuscarinic Drugs Concomitant use of COBENFY with other antimuscarinic drugs that produce anticholinergic adverse reactions (e.g., dry mouth, constipation) may increase the frequency and/or severity of such effects. Monitor patients for increased frequency and/or severity of anticholinergic adverse reactions when COBENFY is used concomitantly with other antimuscarinic drugs. 7.3 Effects on Absorption of Drugs COBENFY may potentially alter the absorption of some concomitantly administered drugs due to anticholinergic effects on gastrointestinal motility. Dosage adjustment of concomitant medications may be necessary based on clinical response and tolerability.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action The mechanism of action of xanomeline in the treatment of schizophrenia is unclear; however, its efficacy is thought to be due to its agonist activity at M1 and M4 muscarinic acetylcholine receptors in the central nervous system. Trospium chloride is a muscarinic antagonist. Trospium chloride antagonizes the muscarinic receptors primarily in the peripheral tissues. 12.2 Pharmacodynamics Xanomeline binds to muscarinic receptors M1 to M5 with comparable affinity (Ki=10, 12, 17, 7, and 22 nM for the M1, M2, M3, M4, and M5 receptors, respectively) and exhibits higher agonist activity at the M1 and M4 receptors. Trospium chloride antagonizes the muscarinic receptors primarily in peripheral tissues. Cardiac Electrophysiology At the maximum recommended dosage of 125 mg/30 mg twice daily, COBENFY does not prolong the QT interval to any clinically relevant extent. 12.3 Pharmacokinetics Following COBENFY administration, xanomeline area under the plasma concentration-time curve during a 12-hour dosing interval (AUC0-12) at steady state and maximum concentration (Cmax) increased 50% when the COBENFY dose increased from 100 mg/20 mg twice daily to 125 mg/30 mg twice daily. Trospium exposures increase dose-proportionally over the COBENFY dosage range of 100 mg/20 mg twice daily to 125 mg/30 mg twice daily. Pharmacokinetic properties of COBENFY are provided in Table 3. Table 3: Pharmacokinetic Properties of COBENFY Parameter Xanomeline Trospium General Information Dose proportionality Greater than proportional Proportional Accumulation a 2 to 3-fold 2 to 3-fold Time to steady state 3 to 5 days 3 to 5 days Absorption T max 2 hours 1 hour Effect of food: PK in fed state (compared to fasted state) High fat meal b C max Unchanged Reduced 70% to 75% AUC Increased 30% Reduced 85% to 90% Low fat meal b C max Unchanged Reduced 70% to 75% AUC Unchanged Reduced 85% to 90% Distribution Central volume of distribution (oral) 10,800 Liters 531 Liters Plasma protein binding Approximately 95% Approximately 80% Elimination Half-life (t 1/2 ) 5 hours 6 hours Apparent clearance 1950 Liters/hour 796 Liters/hour Renal clearance 0.085 Liters/hour 21 Liters/hour Metabolism Primary metabolic pathways CYP450 2D6, 2B6, 1A2, 2C9, and 2C19 Unlikely Other Flavin monooxygenases (FMO1 and FMO3) Ester hydrolysis and glucuronic acid conjugation (not fully characterized) Excretion Urine Total 78% Unknown Unchanged Less than 0.01% 85-90% Tubular secretion Unknown Yes Feces Total 12% Unknown Unchanged Unknown Unknown Abbreviations: AUC = Area under the time-concentration curve; C max = Maximum concentration; T max =Time to C max a Dose-normalized accumulation at steady state b High-fat high-calorie meal is 800-1000 calories, 50% from fat; a low-fat meal is 400-500 calories, 25% from fat Specific Populations Geriatric Patients Population pharmacokinetic analysis suggests that AUC0-12h and Cmax of trospium at steady state were 60% higher and 36% higher, respectively, in subjects 65 years and older compared to subjects younger than 65 years old. The exposures (AUC0-12h and Cmax) of xanomeline at steady state were not different between subjects 65 years and older and subjects younger than 65 years old [see Dosage and Administration (2.3) and Use in Specific Populations (8.5) ] . Male and Female Patients Plasma concentrations of xanomeline and trospium are similar between females and males. Racial or Ethnic Groups Most subjects in clinical studies were Black. Xanomeline and trospium exposure did not differ between Black and non-Black subjects. Studies have included too few subjects of Asian descent to evaluate comparisons. Patients with Renal Impairment The effect of renal impairment on xanomeline and trospium exposure was assessed in a dedicated study that enrolled healthy subjects and subjects with mild, moderate, or severe renal impairment. Estimated glomerular filtration rate (eGFR) was determined by the MDRD equation. Plasma concentrations of xanomeline and trospium increased with increasing renal dysfunction [see Use in Specific Populations (8.6) ] . For xanomeline, compared to subjects with normal renal function (eGFR: ≥90 mL/min), the steady-state Cmax and AUC0-12h were 2.1 and 1.9 times higher in subjects with mild renal impairment (eGFR: 60 to <90 mL/min), 2.4 and 2.1 times higher in subjects with moderate renal impairment (eGFR: 30 to <60 mL/min), and 2.6 and 2.4 times higher in subjects with severe renal impairment (eGFR: <30 mL/min). For trospium, compared to subjects with normal renal function, the steady-state Cmax and AUC0-12h were 1.6 and 1.6 times higher in subjects with mild renal impairment, 2.7 and 2.2 times higher in subjects with moderate renal impairment, and 2.9 and 2.9 times higher in subjects with severe renal impairment. Patients with Hepatic Impairment The effect of hepatic impairment on xanomeline and trospium in combination was assessed in a dedicated study that enrolled healthy subjects and subjects with mild or moderate hepatic impairment as determined by their Child-Pugh score. Plasma concentrations of xanomeline increased with increasing hepatic dysfunction [see Use in Specific Populations (8.7) ] . In subjects with mild hepatic impairment (Child-Pugh Class A), the steady-state Cmax and AUC0-12h of xanomeline was 2.8 and 2.6 times that in subjects with normal hepatic function. Mild and moderate hepatic impairment did not substantially affect trospium exposure, but significantly impacted xanomeline exposures. In subjects with moderate hepatic impairment (Child-Pugh Class B), the steady-state Cmax and AUC0-12h of xanomeline was at least 7 times that in subjects with normal hepatic function [see Contraindications (4) and Warnings and Precautions (5.2) ] . The effect of severe hepatic impairment on xanomeline and trospium exposure was not evaluated. Body Weight Compared to subjects weighing 70 kg, xanomeline exposures were 30 to 35% lower and trospium exposures were 20 to 35% lower in subjects weighing 120 kg. The lower exposures observed in subjects weighing 120 kg are expected to be clinically not meaningful. Drug Interaction Studies Drugs Eliminated by Active Tubular Secretion Active tubular excretion is a major elimination pathway for trospium. Trospium has the potential for pharmacokinetic interactions with other drugs that are eliminated by active tubular secretion. Coadministration of COBENFY with these drugs may increase plasma concentrations of trospium and/or the coadministered drug due to competition for this elimination pathway [see Drug Interactions (7.1) ] . Metformin A drug interaction study was conducted in which extended-release trospium chloride 60 mg once daily was coadministered with metformin hydrochloride 500 mg twice daily under steady-state conditions in 44 healthy subjects. Co-administration of 500 mg metformin immediate-release tablets twice daily reduced the steady-state systemic exposure of trospium by approximately 29% for mean AUC0-24 and by 34% for mean Cmax. The steady-state pharmacokinetics of metformin were comparable when administered with or without 60 mg extended-release trospium chloride once daily under fasted conditions. The effect of metformin at higher doses on trospium pharmacokinetics is unknown. Drugs That Inhibit CYP2D6 CYP2D6 is a significant contributor to the metabolism of xanomeline. Drugs that are inhibitors of CYP2D6 may increase xanomeline concentrations in plasma [see Drug Interactions (7.1) ] . Drugs That Are Substrates of P-glycoprotein In vitro data suggest that xanomeline does not inhibit P-glycoprotein systemically, but it may transiently inhibit P-glycoprotein locally in the intestine after dosing. COBENFY may increase plasma concentrations of coadministered P-gp substrates [see Drug Interactions (7.1) ] . Drugs That Are Substrates of CYP3A4 In vitro data suggest that xanomeline does not inhibit CYP3A4 systemically, but it may transiently inhibit CYP3A4 locally in the intestine after dosing. COBENFY may increase plasma concentrations of coadministered CYP3A4 substrates [see Drug Interactions (7.1) ] . 12.5 Pharmacogenomics CYP2D6 is a significant contributor to the metabolism of xanomeline. The gene encoding CYP2D6 has polymorphisms that impact protein function. Based on a population pharmacokinetic analysis, compared to subjects with normal CYP2D6 function, the median Cmax and median AUC0-12h of xanomeline were estimated to increase by 28% and 15% in CYP2D6 intermediate metabolizers (N=84) and decrease by 43% in both parameters for ultrarapid metabolizers (N=12). The pharmacokinetics of xanomeline have not been adequately characterized in subjects who are poor metabolizers.
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action The mechanism of action of xanomeline in the treatment of schizophrenia is unclear; however, its efficacy is thought to be due to its agonist activity at M1 and M4 muscarinic acetylcholine receptors in the central nervous system. Trospium chloride is a muscarinic antagonist. Trospium chloride antagonizes the muscarinic receptors primarily in the peripheral tissues.
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Xanomeline binds to muscarinic receptors M1 to M5 with comparable affinity (Ki=10, 12, 17, 7, and 22 nM for the M1, M2, M3, M4, and M5 receptors, respectively) and exhibits higher agonist activity at the M1 and M4 receptors. Trospium chloride antagonizes the muscarinic receptors primarily in peripheral tissues. Cardiac Electrophysiology At the maximum recommended dosage of 125 mg/30 mg twice daily, COBENFY does not prolong the QT interval to any clinically relevant extent.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Following COBENFY administration, xanomeline area under the plasma concentration-time curve during a 12-hour dosing interval (AUC0-12) at steady state and maximum concentration (Cmax) increased 50% when the COBENFY dose increased from 100 mg/20 mg twice daily to 125 mg/30 mg twice daily. Trospium exposures increase dose-proportionally over the COBENFY dosage range of 100 mg/20 mg twice daily to 125 mg/30 mg twice daily. Pharmacokinetic properties of COBENFY are provided in Table 3. Table 3: Pharmacokinetic Properties of COBENFY Parameter Xanomeline Trospium General Information Dose proportionality Greater than proportional Proportional Accumulation a 2 to 3-fold 2 to 3-fold Time to steady state 3 to 5 days 3 to 5 days Absorption T max 2 hours 1 hour Effect of food: PK in fed state (compared to fasted state) High fat meal b C max Unchanged Reduced 70% to 75% AUC Increased 30% Reduced 85% to 90% Low fat meal b C max Unchanged Reduced 70% to 75% AUC Unchanged Reduced 85% to 90% Distribution Central volume of distribution (oral) 10,800 Liters 531 Liters Plasma protein binding Approximately 95% Approximately 80% Elimination Half-life (t 1/2 ) 5 hours 6 hours Apparent clearance 1950 Liters/hour 796 Liters/hour Renal clearance 0.085 Liters/hour 21 Liters/hour Metabolism Primary metabolic pathways CYP450 2D6, 2B6, 1A2, 2C9, and 2C19 Unlikely Other Flavin monooxygenases (FMO1 and FMO3) Ester hydrolysis and glucuronic acid conjugation (not fully characterized) Excretion Urine Total 78% Unknown Unchanged Less than 0.01% 85-90% Tubular secretion Unknown Yes Feces Total 12% Unknown Unchanged Unknown Unknown Abbreviations: AUC = Area under the time-concentration curve; C max = Maximum concentration; T max =Time to C max a Dose-normalized accumulation at steady state b High-fat high-calorie meal is 800-1000 calories, 50% from fat; a low-fat meal is 400-500 calories, 25% from fat Specific Populations Geriatric Patients Population pharmacokinetic analysis suggests that AUC0-12h and Cmax of trospium at steady state were 60% higher and 36% higher, respectively, in subjects 65 years and older compared to subjects younger than 65 years old. The exposures (AUC0-12h and Cmax) of xanomeline at steady state were not different between subjects 65 years and older and subjects younger than 65 years old [see Dosage and Administration (2.3) and Use in Specific Populations (8.5) ] . Male and Female Patients Plasma concentrations of xanomeline and trospium are similar between females and males. Racial or Ethnic Groups Most subjects in clinical studies were Black. Xanomeline and trospium exposure did not differ between Black and non-Black subjects. Studies have included too few subjects of Asian descent to evaluate comparisons. Patients with Renal Impairment The effect of renal impairment on xanomeline and trospium exposure was assessed in a dedicated study that enrolled healthy subjects and subjects with mild, moderate, or severe renal impairment. Estimated glomerular filtration rate (eGFR) was determined by the MDRD equation. Plasma concentrations of xanomeline and trospium increased with increasing renal dysfunction [see Use in Specific Populations (8.6) ] . For xanomeline, compared to subjects with normal renal function (eGFR: ≥90 mL/min), the steady-state Cmax and AUC0-12h were 2.1 and 1.9 times higher in subjects with mild renal impairment (eGFR: 60 to <90 mL/min), 2.4 and 2.1 times higher in subjects with moderate renal impairment (eGFR: 30 to <60 mL/min), and 2.6 and 2.4 times higher in subjects with severe renal impairment (eGFR: <30 mL/min). For trospium, compared to subjects with normal renal function, the steady-state Cmax and AUC0-12h were 1.6 and 1.6 times higher in subjects with mild renal impairment, 2.7 and 2.2 times higher in subjects with moderate renal impairment, and 2.9 and 2.9 times higher in subjects with severe renal impairment. Patients with Hepatic Impairment The effect of hepatic impairment on xanomeline and trospium in combination was assessed in a dedicated study that enrolled healthy subjects and subjects with mild or moderate hepatic impairment as determined by their Child-Pugh score. Plasma concentrations of xanomeline increased with increasing hepatic dysfunction [see Use in Specific Populations (8.7) ] . In subjects with mild hepatic impairment (Child-Pugh Class A), the steady-state Cmax and AUC0-12h of xanomeline was 2.8 and 2.6 times that in subjects with normal hepatic function. Mild and moderate hepatic impairment did not substantially affect trospium exposure, but significantly impacted xanomeline exposures. In subjects with moderate hepatic impairment (Child-Pugh Class B), the steady-state Cmax and AUC0-12h of xanomeline was at least 7 times that in subjects with normal hepatic function [see Contraindications (4) and Warnings and Precautions (5.2) ] . The effect of severe hepatic impairment on xanomeline and trospium exposure was not evaluated. Body Weight Compared to subjects weighing 70 kg, xanomeline exposures were 30 to 35% lower and trospium exposures were 20 to 35% lower in subjects weighing 120 kg. The lower exposures observed in subjects weighing 120 kg are expected to be clinically not meaningful. Drug Interaction Studies Drugs Eliminated by Active Tubular Secretion Active tubular excretion is a major elimination pathway for trospium. Trospium has the potential for pharmacokinetic interactions with other drugs that are eliminated by active tubular secretion. Coadministration of COBENFY with these drugs may increase plasma concentrations of trospium and/or the coadministered drug due to competition for this elimination pathway [see Drug Interactions (7.1) ] . Metformin A drug interaction study was conducted in which extended-release trospium chloride 60 mg once daily was coadministered with metformin hydrochloride 500 mg twice daily under steady-state conditions in 44 healthy subjects. Co-administration of 500 mg metformin immediate-release tablets twice daily reduced the steady-state systemic exposure of trospium by approximately 29% for mean AUC0-24 and by 34% for mean Cmax. The steady-state pharmacokinetics of metformin were comparable when administered with or without 60 mg extended-release trospium chloride once daily under fasted conditions. The effect of metformin at higher doses on trospium pharmacokinetics is unknown. Drugs That Inhibit CYP2D6 CYP2D6 is a significant contributor to the metabolism of xanomeline. Drugs that are inhibitors of CYP2D6 may increase xanomeline concentrations in plasma [see Drug Interactions (7.1) ] . Drugs That Are Substrates of P-glycoprotein In vitro data suggest that xanomeline does not inhibit P-glycoprotein systemically, but it may transiently inhibit P-glycoprotein locally in the intestine after dosing. COBENFY may increase plasma concentrations of coadministered P-gp substrates [see Drug Interactions (7.1) ] . Drugs That Are Substrates of CYP3A4 In vitro data suggest that xanomeline does not inhibit CYP3A4 systemically, but it may transiently inhibit CYP3A4 locally in the intestine after dosing. COBENFY may increase plasma concentrations of coadministered CYP3A4 substrates [see Drug Interactions (7.1) ] .
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS COBENFY is contraindicated in patients with: • urinary retention [see Warnings and Precautions (5.1) ] . • moderate (Child-Pugh Class B) or severe (Child-Pugh Class C) hepatic impairment [see Warnings and Precautions (5.2) ] . • gastric retention [see Warnings and Precautions (5.4) ] . • history of hypersensitivity to COBENFY or trospium chloride. Angioedema has been reported with COBENFY and trospium chloride [see Warnings and Precautions (5.5) ] . • untreated narrow-angle glaucoma [see Warnings and Precautions (5.6) ] . COBENFY is contraindicated in: • urinary retention ( 4 ) • moderate or severe hepatic impairment ( 4 ) • gastric retention ( 4 ) • history of hypersensitivity to COBENFY or trospium chloride ( 4 ) • untreated narrow-angle glaucoma ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION COBENFY is a combination of xanomeline, a muscarinic agonist, and trospium chloride, a muscarinic antagonist. The chemical name of xanomeline tartrate is pyridine, 3-[4-(hexyloxy)-1,2,5-thiadiazol-3-yl]-1,2,5,6-tetrahydro-1-methyl-, (2R,3R)-2,3-dihydroxybutanedioate (1:1). Its molecular formula is C14H23N3OS.C4H6O6 and its molecular weight is 431.51 g/mol. Xanomeline tartrate is a white to slightly tan crystalline solid. Xanomeline tartrate is highly soluble in protic solvents, such as methanol and water, and in polar organic solvents such as DMF and dimethyl sulfoxide (DMSO). It is poorly soluble in lipophilic organic solvents, such as hexane or octanol. The chemical structure of xanomeline tartrate is: Trospium chloride is a quaternary ammonium compound with the chemical name of spiro[8-azoniabicyclo[3.2.1]octane-8,1′-pyrrolidinium], 3-[(2-hydroxy-2,2-diphenylacetyl)oxy]-, chloride (1:1), (1α,3β,5α). The molecular formula of trospium chloride is C25H30NO3.Cl and its molecular weight is 427.96 g/mol. Trospium chloride is a fine, colorless to slightly yellow, crystalline solid. Trospium chloride is highly soluble in water, freely soluble in methanol, and practically insoluble in methylene chloride. The chemical structure of trospium chloride is: COBENFY (xanomeline and trospium chloride) is for oral administration and is available in capsules in the following strengths: • 50 mg/20 mg (equivalent to 76.7 mg xanomeline tartrate and 18.3 mg trospium). • 100 mg/20 mg (equivalent to 153.3 mg xanomeline tartrate and 18.3 mg trospium). • 125 mg/30 mg (equivalent to 191.7 mg xanomeline tartrate and 27.5 mg trospium). COBENFY capsules contain a combination of pellets of xanomeline and pellets of trospium chloride. Inactive ingredients: The xanomeline tartrate pellets contain ascorbic acid, microcrystalline cellulose, and talc. The trospium chloride pellets contain lactose monohydrate, microcrystalline cellulose, and talc. The capsules, printed with black ink, contain black iron oxide (only 100 mg/20 mg), hypromellose, red iron oxide, titanium dioxide, and yellow iron oxide (only 50 mg/20 mg and 100 mg/20 mg). Chemical Structure Chemical Structure
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION • Assess liver enzymes and bilirubin prior to initiating treatment with COBENFY and as clinically indicated during treatment. ( 2.1 ) • Assess heart rate at baseline and as clinically indicated during treatment with COBENFY. ( 2.1 ) • Recommended starting dosage of COBENFY is 50 mg/20 mg orally twice daily for at least two days, then increase the dosage to 100 mg/20 mg twice daily for at least five days. ( 2.2 ) • Dosage may be increased to 125 mg/30 mg orally twice daily based on patient tolerability and response. ( 2.2 ) • See the full prescribing information for the recommended titration and maximum recommended dosage. ( 2.2 ) • Take at least 1 hour before a meal or at least 2 hours after a meal. Do not open capsules. ( 2.2 ) • Geriatric patients: Recommended starting dosage of COBENFY is 50 mg/20 mg orally twice daily. Consider a slower titration. The maximum recommended dosage is 100 mg/20 mg twice daily. ( 2.3 ) 2.1 Recommended Testing and Monitoring Prior to Initiation and During Treatment with COBENFY • Assess liver enzymes and bilirubin prior to initiating COBENFY and as clinically indicated during treatment [see Contraindications (4) and Warnings and Precautions (5.2 , 5.3) ] . • Assess heart rate at baseline and as clinically indicated during treatment [see Warnings and Precautions (5.7) ] . 2.2 Recommended Dosage and Administration The recommended dosage of COBENFY is as follows: • The recommended starting dosage is one 50 mg/20 mg capsule (contains 50 mg of xanomeline and 20 mg of trospium chloride) orally twice daily for at least two days. • Increase the dosage to one 100 mg/20 mg capsule (contains 100 mg of xanomeline and 20 mg of trospium chloride) orally twice daily for at least five days. • The dosage may be increased to one 125 mg/30 mg capsule (contains 125 mg of xanomeline and 30 mg of trospium chloride) orally twice daily based on patient tolerability and response [see Clinical Studies (14) ] . • Maximum recommended dosage is 125 mg/30 mg orally twice daily. Administer COBENFY orally at least one hour before a meal or at least two hours after a meal [see Clinical Pharmacology (12.3) ] . Do not open the capsules. 2.3 Dosage Recommendations in Geriatric Patients The recommended starting dosage of COBENFY in geriatric patients is one 50 mg/20 mg capsule orally twice daily. Consider a slower titration for geriatric patients. The maximum recommended dosage in geriatric patients is one 100 mg/20 mg capsule twice daily [see Warnings and Precautions (5.1 , 5.8) and Use in Specific Populations (8.5) ] .
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS COBENFY is available as: • 50 mg/20 mg (xanomeline/trospium chloride): Buff capsules imprinted with Karuna 50/20 mg • 100 mg/20 mg (xanomeline/trospium chloride): Brown capsules imprinted with Karuna 100/20 mg • 125 mg/30 mg (xanomeline/trospium chloride): Swedish Orange capsules imprinted with Karuna 125/30 mg Capsules (xanomeline/trospium chloride): 50 mg/20 mg, 100 mg/20 mg, 125 mg/30 mg ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE COBENFY is indicated for the treatment of schizophrenia in adults. COBENFY is a combination of xanomeline, a muscarinic agonist, and trospium chloride, a muscarinic antagonist, indicated for the treatment of schizophrenia in adults. ( 1 )
Spl product data elements
Usually a list of ingredients in a drug product.Cobenfy xanomeline and trospium chloride xanomeline xanomeline trospium chloride trospium microcrystalline cellulose ascorbic acid talc lactose monohydrate hypromellose, unspecified titanium dioxide ferric oxide red ferric oxide yellow Light Tan Karuna;50;20 Cobenfy xanomeline and trospium chloride xanomeline xanomeline trospium chloride trospium microcrystalline cellulose ascorbic acid talc lactose monohydrate hypromellose, unspecified titanium dioxide ferric oxide red ferric oxide yellow ferrosoferric oxide Karuna;100;20 Cobenfy xanomeline and trospium chloride xanomeline xanomeline trospium chloride trospium microcrystalline cellulose ascorbic acid talc lactose monohydrate hypromellose, unspecified titanium dioxide ferric oxide red Dark Orange Karuna;125;30 Cobenfy xanomeline and trospium chloride Cobenfy xanomeline and trospium chloride xanomeline xanomeline trospium chloride trospium microcrystalline cellulose ascorbic acid talc lactose monohydrate hypromellose, unspecified titanium dioxide ferric oxide red ferric oxide yellow Light Tan Karuna;50;20 Cobenfy xanomeline and trospium chloride xanomeline xanomeline trospium chloride trospium microcrystalline cellulose ascorbic acid talc lactose monohydrate hypromellose, unspecified titanium dioxide ferric oxide red ferric oxide yellow ferrosoferric oxide Karuna;100;20 Cobenfy xanomeline and trospium chloride Cobenfy xanomeline and trospium chloride xanomeline xanomeline trospium chloride trospium microcrystalline cellulose ascorbic acid talc lactose monohydrate hypromellose, unspecified titanium dioxide ferric oxide red ferric oxide yellow Light Tan Karuna;50;20 Cobenfy xanomeline and trospium chloride xanomeline xanomeline trospium chloride trospium microcrystalline cellulose ascorbic acid talc lactose monohydrate hypromellose, unspecified titanium dioxide ferric oxide red ferric oxide yellow ferrosoferric oxide Karuna;100;20
Animal pharmacology and or toxicology
Information from studies of the drug in animals, if the data were not relevant to nor included in other parts of the labeling. Most labels do not contain this field.13.2 Animal Toxicology and/or Pharmacology In the 2-year dietary study in rats, biliary cysts and/or biliary/biliary ductule dilatation were observed at xanomeline doses equal to or greater than the MRHD of 250/60 mg xanomeline/trospium chloride, based on BSA.
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis Xanomeline Xanomeline was administered to rats in the diet at doses of 9, 37, and 134 mg/kg/day in males and 11, 46, and 170 mg/kg/day in females, respectively, for two years. Biliary hyperplasia was observed in all groups with increased incidence and/or severity at ≥ 37 and 46 mg/kg/day in males and females, respectively, relative to controls. There was no increase in the incidence of tumors at doses up to 37 and 46/mg/kg/day in males and females, respectively; these doses are 1.4 to 1.8 times higher than the xanomeline dose at the MRHD of 250/60 mg xanomeline/trospium, based on mg/m2 BSA. The high doses of 134 and 170 mg/kg/day in males and females exceeded the maximum tolerated dose (MTD), precluding an adequate assessment for carcinogenic effect at this dose. Xanomeline was administered to mice in the diet at doses of 52, 174, and 559 mg/kg/day for 21 months in both sexes. Xanomeline did not increase the incidence of tumors in mice at doses up to 174 mg/kg/day, which is approximately 3 times the xanomeline dose at the MRHD, based on BSA. The high dose of 559 mg/kg/day exceeded the MTD, precluding an adequate assessment for carcinogenic effect at this dose. Trospium chloride Trospium chloride did not increase the incidence of tumors in rats treated for 104 weeks at doses up to 200 mg/kg/day, which is approximately 32 times the trospium chloride dose at the MRHD, based on BSA. Trospium chloride did not increase the incidence of tumors in mice treated for 78 weeks at doses up to 200 mg/kg/day, which is approximately 16 times the trospium chloride dose at the MRHD, based on BSA. Mutagenesis Xanomeline Xanomeline was not mutagenic in the in vitro bacterial reverse mutation (Ames assay) or mouse lymphoma assay. Xanomeline did not induce unscheduled DNA synthesis in rat hepatocytes and was not clastogenic in the in vitro chromosome aberration assay or in the in vivo mouse bone marrow micronucleus assay. Trospium chloride Trospium chloride was not mutagenic nor genotoxic in tests in vitro in bacteria (Ames assay) and mammalian cells (L5178Y mouse lymphoma and CHO cells) or in vivo in the rat micronucleus test. Impairment of Fertility Xanomeline Xanomeline did not affect fertility when orally administered to male rats via the diet at doses of 15, 44, and 150 mg/kg/day. The NOAEL for male fertility is 150 mg/kg/day, which is approximately 6 times the xanomeline dose at the MRHD of 250/60 mg xanomeline/trospium, based on BSA. Xanomeline did not affect fertility when administered subcutaneously to male and female rats at doses of 1, 5, and 25 mg/kg/day. The NOAEL for male and female fertility is 25 mg/kg/day, which is equal to the xanomeline dose at the MRHD, based on BSA. Trospium chloride Trospium chloride did not affect fertility in rats at doses up to 200 mg/kg/day which is approximately 32 times the trospium chloride dose at the MRHD, based on BSA.
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis Xanomeline Xanomeline was administered to rats in the diet at doses of 9, 37, and 134 mg/kg/day in males and 11, 46, and 170 mg/kg/day in females, respectively, for two years. Biliary hyperplasia was observed in all groups with increased incidence and/or severity at ≥ 37 and 46 mg/kg/day in males and females, respectively, relative to controls. There was no increase in the incidence of tumors at doses up to 37 and 46/mg/kg/day in males and females, respectively; these doses are 1.4 to 1.8 times higher than the xanomeline dose at the MRHD of 250/60 mg xanomeline/trospium, based on mg/m2 BSA. The high doses of 134 and 170 mg/kg/day in males and females exceeded the maximum tolerated dose (MTD), precluding an adequate assessment for carcinogenic effect at this dose. Xanomeline was administered to mice in the diet at doses of 52, 174, and 559 mg/kg/day for 21 months in both sexes. Xanomeline did not increase the incidence of tumors in mice at doses up to 174 mg/kg/day, which is approximately 3 times the xanomeline dose at the MRHD, based on BSA. The high dose of 559 mg/kg/day exceeded the MTD, precluding an adequate assessment for carcinogenic effect at this dose. Trospium chloride Trospium chloride did not increase the incidence of tumors in rats treated for 104 weeks at doses up to 200 mg/kg/day, which is approximately 32 times the trospium chloride dose at the MRHD, based on BSA. Trospium chloride did not increase the incidence of tumors in mice treated for 78 weeks at doses up to 200 mg/kg/day, which is approximately 16 times the trospium chloride dose at the MRHD, based on BSA. Mutagenesis Xanomeline Xanomeline was not mutagenic in the in vitro bacterial reverse mutation (Ames assay) or mouse lymphoma assay. Xanomeline did not induce unscheduled DNA synthesis in rat hepatocytes and was not clastogenic in the in vitro chromosome aberration assay or in the in vivo mouse bone marrow micronucleus assay. Trospium chloride Trospium chloride was not mutagenic nor genotoxic in tests in vitro in bacteria (Ames assay) and mammalian cells (L5178Y mouse lymphoma and CHO cells) or in vivo in the rat micronucleus test. Impairment of Fertility Xanomeline Xanomeline did not affect fertility when orally administered to male rats via the diet at doses of 15, 44, and 150 mg/kg/day. The NOAEL for male fertility is 150 mg/kg/day, which is approximately 6 times the xanomeline dose at the MRHD of 250/60 mg xanomeline/trospium, based on BSA. Xanomeline did not affect fertility when administered subcutaneously to male and female rats at doses of 1, 5, and 25 mg/kg/day. The NOAEL for male and female fertility is 25 mg/kg/day, which is equal to the xanomeline dose at the MRHD, based on BSA. Trospium chloride Trospium chloride did not affect fertility in rats at doses up to 200 mg/kg/day which is approximately 32 times the trospium chloride dose at the MRHD, based on BSA. 13.2 Animal Toxicology and/or Pharmacology In the 2-year dietary study in rats, biliary cysts and/or biliary/biliary ductule dilatation were observed at xanomeline doses equal to or greater than the MRHD of 250/60 mg xanomeline/trospium chloride, based on BSA.
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PRINCIPAL DISPLAY PANEL - 50 mg/20 mg Capsule Bottle Label NDC 0003-0050-60 Rx Only COBENFY™ (xanomeline and trospium chloride) capsules Recommended Dosage: Take one capsule twice daily. See Prescribing Information 50 mg/20 mg 60 Capsules 50 mg/20 mg Bottle Labels
PRINCIPAL DISPLAY PANEL - 100 mg/20 mg Capsule Bottle Label NDC 0003-1100-60 COBENFY™ (xanomeline and trospium chloride) capsules 100 mg/20 mg Rx Only 60 CAPSULES Recommended Dosage: Take one capsule twice daily. See Prescribing Information 100 mg/20 mg Bottle Labels
PRINCIPAL DISPLAY PANEL - 125 mg/30 mg Capsule Bottle Label NDC 0003-0125-60 Rx Only COBENFY™ (xanomeline and trospium chloride) capsules 125 mg/30 mg Rx Only 60 Capsules Recommended Dosage: Take on capsule twice daily. See Prescribing Information 125 mg/30 mg Capsule Bottle Label
PRINCIPAL DISPLAY PANEL - Kit Carton NDC 0003-5200-56 Rx Only COBENFY™ (xanomeline and trospium chloride) capsules 50 mg/20 mg per capsule 100 mg/20 mg per capsule Starter Pack FOR ORAL USE This Starter Pack contains 56 capsules for dosing over 28 days. The contents of this pack are as follows: Four - 50 mg/20 mg capsules Fifty-two - 100 mg/20 mg capsules Starter Pack Carton
PRINCIPAL DISPLAY PANEL - Sample Titration Wallet PROFESSIONAL SAMPLE NOT FOR RESALE NDC 0003-5150-14 Rx Only COBENFY™ (xanomeline and trospium chloride) capsules 50 mg/20 mg per capsule 100 mg/20 mg per capsule TITRATION PACK Days 1-2: Take one capsule (50 mg/20 mg) twice daily Days 3-7: Take one capsule (100 mg/20 mg) twice daily Contains 14 capsules: Four - 50 mg/20 mg capsules Ten - 100 mg/20 mg capsules Sample Titration Pack
Cobenfy: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Advise the patient to read the FDA-approved patient labeling (Patient Information). Risk of Urinary Retention Inform patients that COBENFY may cause urinary retention and that the risk of urinary retention is greater in some patients, including geriatric patients and those with bladder outlet obstruction (e.g., due to BPH) and patients with other causes of reduced bladder emptying (e.g., diabetic cystopathy). Urinary retention may occur at any time during treatment with COBENFY and is more likely when taking higher doses. Advise patients to monitor for symptoms of urinary retention, such as urinary hesitancy, weak urinary stream, incomplete bladder emptying and pain with urination, and to promptly report these symptoms to their healthcare provider. Inform patients that urinary retention may increase the risk of urinary tract infection. Advise patients to seek immediate medical attention if they are unable to urinate [see Warnings and Precautions (5.1) ] . Risk of Use in Patients with Hepatic Impairment Instruct patients to report signs of hepatic impairment (e.g., skin and eyes that appear yellowish, abdominal pain and swelling, itchy skin, dark urine color) and symptoms of hepatic injury (e.g., biliary spasm, pancreatitis, and cholangitis) to their healthcare provider [see Warnings and Precautions (5.2) ] . Risk of Use in Patients with Biliary Disease Inform patients that COBENFY can increase liver enzymes and about the need for specific monitoring, including liver enzymes and bilirubin levels. Inform patients to report symptoms such as dyspepsia, nausea, vomiting, or upper abdominal pain to their healthcare provider [see Warnings and Precautions (5.3) ] . Decreased Gastrointestinal Motility Inform patients that COBENFY can delay or slow emptying of food in their stomach. Advise patients to inform their healthcare provider about the presence of or symptoms of gastrointestinal obstructive disorders and conditions such as ulcerative colitis, intestinal atony, and myasthenia gravis [see Warnings and Precautions (5.4) ] . Risk of Angioedema Advise patients that hypersensitivity reactions to COBENFY could and occur and result in life-threatening airway obstruction. Instruct patients to seek medical attention if they experience edema of the tongue, edema of the laryngopharynx, or difficulty breathing occurs, discontinue COBENFY, and seek immediate medical attention [see Warnings and Precautions (5.5) ] . Risk of Use in Patients with Narrow-angle Glaucoma Inform patients pupillary dilation may occur with COBENFY use and in susceptible individuals, can lead to an episode of angle closure glaucoma [see Warnings and Precautions (5.6) ] . Increases in Heart Rate Inform patients that COBENFY can increase heart rate [see Warnings and Precautions (5.7) ] . Anticholinergic Adverse Reactions in Patients with Renal Impairment Inform patients that COBENFY is associated with anticholinergic adverse reactions such as dry mouth, constipation, dyspepsia, urinary tract infection, and urinary retention and the effects are expected to be greater in patients with renal impairment [see Warnings and Precautions (5.8) ] . Central Nervous System Effects Advise patients that COBENFY is associated with central nervous system effects such as dizziness, confusion, hallucinations, and somnolence. Caution patients about performing activities requiring mental alertness, such as operating hazardous machinery or operating a motor vehicle, until they are reasonably certain that COBENFY therapy does not adversely affect their ability to engage in such activities [see Warnings and Precautions (5.9) ] . Administration Information Instruct patients to take COBENFY twice daily at least one hour before a meal or at least 2 hours after a meal and not to open the capsules [see Dosage and Administration (2.2) ] . Concomitant Medications Advise patients to inform their health care providers of any changes to their current prescription or over-the-counter medications because there may be a potential for interactions [see Drug Interactions (7) ] . Pregnancy Advise patients to notify their healthcare provider with a known or suspected pregnancy. Advise pregnant women that there is a pregnancy exposure registry that monitors outcomes in females exposed to COBENFY during pregnancy [see Use in Specific Populations (8.1) ] . Marketed by: Bristol-Myers Squibb Company Princeton, NJ 08543 USA COBENFY is a trademark of Karuna Therapeutics, Inc., a Bristol Myers Squibb company.
Spl patient package insert
Information necessary for patients to use the drug safely and effectively.PATIENT INFORMATION COBENFY™ (co-BEN-fee) (xanomeline and trospium chloride) capsules What is COBENFY? COBENFY is a prescription medicine used to treat schizophrenia in adults. It is not known if COBENFY is safe and effective in children. Do not take COBENFY if you: • have urinary retention problems that cause your bladder to not empty completely or not empty at all • have moderate or severe liver problems (impairment) • have gastric retention problems that cause your stomach to empty slowly • are allergic to COBENFY, xanomeline, or trospium chloride, or any of the ingredients in COBENFY. See the end of this Patient Information leaflet for a complete list of ingredients in COBENFY. • have an eye problem called untreated narrow-angle glaucoma Before taking COBENFY, tell your healthcare provider about all of your medical conditions, including if you : • have an enlarged prostate, problems passing urine, or a blockage in your urinary bladder • have liver problems • have or had gallstones or problems with your bile ducts or pancreas • have stomach or intestinal problems including constipation, ulcerative colitis, slow emptying of your stomach, or myasthenia gravis • have an eye condition called narrow-angle glaucoma • have kidney problems • are pregnant or plan to become pregnant. It is not known if COBENFY may harm your unborn baby. Tell your healthcare provider if you become pregnant or think you are pregnant during treatment with COBENFY. o There is a pregnancy exposure registry for women who take COBENFY during pregnancy. The purpose of this registry is to collect information about the health of women exposed to COBENFY and their baby. If you become pregnant during treatment with COBENFY, your healthcare provider will register you by calling 1-866-961-2388 or online at https://womensmentalhealth.org/research/pregnancyregistry/atypicalantipsychotic/. • are breastfeeding or plan to breastfeed. It is not known if COBENFY passes into your breast milk or if it can harm your baby. Tell your healthcare provider about all the medicines you take , including prescription and over-the-counter medicines, vitamins, and herbal supplements. Taking COBENFY with certain other medicines may increase your risk of side effects from COBENFY or the other medicine and may affect the way COBENFY or the other medicine works. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine. How should I take COBENFY? • Take COBENFY exactly as your healthcare provider tells you. Do not change the dose or stop taking COBENFY without first talking to your healthcare provider. • Take 1 COBENFY capsule 2 times each day. • Take COBENFY by mouth at least 1 hour before a meal or at least 2 hours after a meal. • Do not open the capsules. • If you take too much COBENFY, call your healthcare provider or Poison Help Line at 1-800-222-1222, or go to the nearest hospital emergency room right away. What should I avoid while taking COBENFY? Do not drive, operate heavy machinery, or do other dangerous activities until you know how COBENFY affects you. COBENFY may cause dizziness, confusion, seeing or hearing things that are not real (hallucinations), and sleepiness. What are the possible side effects of COBENFY? COBENFY may cause serious side effects, including: • Problems with emptying your bladder (urinary retention). See “Do not take COBENFY if you:” COBENFY may cause your bladder to not empty completely or not empty at all. You are at increased risk for urinary retention if you are elderly, have a blockage in your bladder, have an enlarged prostate called benign prostatic hyperplasia (BPH), have bladder emptying problems from diabetes, or are taking higher doses of COBENFY. Urinary retention may increase your risk for getting a urinary tract infection. Call your healthcare provider or get emergency help right away if you get any signs or symptoms of urinary retention during treatment with COBENFY, including: o difficulty urinating o urination in a weak stream or drips o urinating frequently o full bladder and difficulty emptying your bladder o pain when you urinate • Risks in people with liver problems . See “Do not take COBENFY if you:” It is not recommended that people with mild liver problems (impairment) take COBENFY because they have an increased risk of getting side effects from COBENFY. Your healthcare provider will check the liver enzyme levels in your blood before starting treatment and as needed during treatment with COBENFY. Tell your healthcare provider if you get any signs or symptoms of liver problems during treatment with COBENFY, including: o yellowing of your skin or the white part of your eyes o dark urine o pain and swelling in the upper right part of your stomach (abdomen) o stomach pain that spreads to your back or to below your right shoulder o itching o nausea or vomiting o loss of appetite o fever o chills o light colored stools o tiredness • Risks in people with bile duct and gallbladder problems (biliary disease). COBENFY may cause a blockage in your bile ducts that could lead to gallstones, pancreatitis, and increases in your liver enzymes. Your healthcare provider will check your liver enzyme and bilirubin levels in your blood before starting treatment and as needed during treatment with COBENFY. Tell your healthcare provider if you get any signs or symptoms of biliary disorders during treatment with COBENFY, including: o stomach upset or burning (dyspepsia) o nausea o vomiting o pain in the upper right part of your stomach • Slow emptying of your stomach (decreased gastrointestinal motility). See “Do not take COBENFY if you:” You are at increased risk for getting decreased gastrointestinal motility if you have ulcerative colitis, already have problems with slow stomach emptying, and have myasthenia gravis. Tell your healthcare provider if you get any signs and symptoms of decreased gastrointestinal motility during treatment with COBENFY, including: o constipation o vomiting o nausea o stomach (abdominal) bloating o stomach (abdominal) pain o a feeling of fullness after eating just a few bites o acid reflux • Serious allergic reactions (angioedema). Angioedema may happen during treatment with COBENFY and can be life threatening. Stop taking COBENFY and call your healthcare provider or get emergency help right away if you get any of the following signs or symptoms of a serious allergic reaction during treatment with COBENFY, including: o hives o swelling of your face, lips, mouth, or tongue o swelling of your throat o hoarseness or difficulty speaking o breathing problems • An eye problem called narrow-angle glaucoma. See “Do not take COBENFY if you:” If you already have narrow angles in your eyes, COBENFY may cause a sudden attack (acute angle closure) of glaucoma. Tell your healthcare provider if you get any signs or symptoms of narrow-angle glaucoma during treatment with COBENFY, including: o red eyes o blurred vision o seeing halos or bright colors around lights o eye pain or discomfort o nausea or vomiting o severe headache • Increases in heart rate. COBENFY may increase your heart (pulse) rate. Your healthcare provider should check your heart rate before you start treatment and during treatment as needed. Tell your healthcare provider if you get a racing or pounding feeling in your chest during treatment with COBENFY. • Side effects in people with kidney problems. People with kidney problems may have an increased risk of getting dry mouth, constipation, stomach upset or burning, urinary tract infection, and urinary retention during treatment with COBENFY. • Central nervous system problems. See “What should I avoid while taking COBENFY?” The most common side effects of COBENFY include: • nausea • stomach upset or burning (dyspepsia) • constipation • vomiting • high blood pressure • stomach (abdominal) pain • diarrhea • increased heart rate • dizziness • heartburn (gastrointestinal reflux disease) Your healthcare provider may lower your dose or stop treatment with COBENFY if you get certain side effects. These are not all of the possible side effects of COBENFY. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store COBENFY? • Store COBENFY at room temperature between 68°F to 77°F (20°C to 25°C). Keep COBENFY and all medicines out of the reach of children. General information about the safe and effective use of COBENFY. Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use COBENFY for a condition for which it was not prescribed. Do not give your COBENFY to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about COBENFY that is written for health professionals. What are the ingredients in COBENFY? Active ingredients : xanomeline and trospium chloride Inactive ingredients : ascorbic acid, lactose monohydrate, microcrystalline cellulose, and talc The capsule shell contains black iron oxide (only 100 mg/20 mg), hypromellose, red iron oxide, titanium dioxide, and yellow iron oxide (only 50 mg/20 mg and 100 mg/20 mg). Marketed by: Bristol-Myers Squibb Company Princeton, NJ 08543 USA COBENFY is a trademark of Karuna Therapeutics, Inc., a Bristol Myers Squibb company. For more information, go to www.COBENFY.com or call 1-800-721-5072. This Patient Information has been approved by the U.S. Food and Drug Administration. Issued: 9/2024
| |||
| |||
| |||
| |||
|
| ||
| |||
|
| ||
| |||
|
| ||
| |||
|
| ||
| |||
|
| ||
| |||
|
| ||
| |||
|
| ||
| |||
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES The efficacy of COBENFY for the treatment of schizophrenia in adults was evaluated in two placebo-controlled studies with identical designs (N = 470). Study 1 (NCT04659161) and Study 2 (NCT04738123) were five-week, randomized, double-blind, placebo-controlled, multi-center studies in adult patients with a diagnosis of schizophrenia according to the DSM-5 criteria. In Study 1 and Study 2, patients randomized to COBENFY were started on an initial dose of 50 mg/20 mg orally twice daily for the first 2 days and if tolerated, followed by 100 mg/20 mg orally twice daily for the remainder of Week 1 (Days 3 to 7). On Day 8, dosing was titrated upwards to 125 mg/30 mg orally twice daily unless the patient could not tolerate it. All patients could return to 100 mg/20 mg orally twice daily for the remainder of the treatment period. Demographic and baseline disease characteristics were similar for the COBENFY and placebo groups. Median age was 46 years (range 19 to 65 years). Twenty-five percent of patients were female, 31% were White, 68% were Black or African American, and 1% were Other (or not reported). The primary efficacy measure was the change from baseline in the Positive and Negative Syndrome Scale (PANSS) total score at Week 5. The PANSS is a 30-item scale that measures symptoms of schizophrenia. Each item is rated by a clinician on a seven-point scale. A score of 1 indicates the absence of symptoms, and a score of 7 indicates extremely severe symptoms. The PANSS total score may range from 30 to 210 with higher scores reflecting greater overall symptom severity. In Study 1 and Study 2, patients randomized to COBENFY showed a statistically significant reduction from baseline to Week 5 in the PANSS Total Score compared to the placebo group. The results of Studies 1 and 2 are shown in Table 4. A secondary endpoint, the change from baseline to Week 5 on the Clinical Global Impression‒Severity (CGI-S) score, was statistically significant for COBENFY compared to placebo in Study 1. The CGI-S is a validated clinician-rated scale that measures the patient’s current illness state and overall clinical state on a 1 (normal, not at all ill) to 7-point (extremely ill) scale. Examination of subgroups by age, sex, and race did not suggest differences in response in the study (there were no patients over 65 years of age). Table 4: Primary Efficacy Results for Change from Baseline in PANSS Total Score at Week 5 in Adults with Schizophrenia (Studies 1 and 2) Primary Efficacy Endpoint: PANSS Total Score Study Number Treatment Group N Mean Baseline Score (SD) LS Mean Change from Baseline (SE) Placebo-subtracted Difference (95% CI) a 1 COBENFY 117 98.2 (8.9) -21.2 (1.7) -9.6 (-13.9, -5.2)* Placebo 119 97.7 (9.4) -11.6 (1.6) 2 COBENFY 114 96.9 (8.8) -20.6 (1.6) -8.4 (-12.4, -4.3)* Placebo 120 96.5 (8.8) -12.2 (1.6) The PANSS Total Score may range from 30 to 210; higher scores reflect greater symptom severity. SD: standard deviation; SE: standard error; LS Mean: least-squares mean; CI: confidence interval. a Difference (drug minus placebo) in LS mean change from baseline. * Statistically significantly superior to placebo. The change from baseline in PANSS total score to Week 5 is summarized in Figure 1. Figure 1: Change from Baseline in PANSS Total Score by Week in Adults with Schizophrenia (Study 1) Error bars represent standard error. LS=least squares; SE=standard error Change from baseline PANSS
| Error bars represent standard error. LS=least squares; SE=standard error |
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use Controlled clinical studies of COBENFY did not include patients older than 65 years of age to determine whether they respond differently from younger adult patients. Because COBENFY can increase the risk of urinary retention in geriatric patients, including older males with bladder outlet obstruction due to benign prostatic hyperplasia (BPH), a slower titration and lower maximum dosage is recommended in geriatric patients [see Dosage and Administration (2.3) and Warnings and Precautions (5.1) ] .
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use The safety and effectiveness of COBENFY in pediatric patients have not been established.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Pregnancy Exposure Registry There is a pregnancy exposure registry that monitors outcomes in women exposed to psychiatric medications, including COBENFY, during pregnancy. Healthcare providers are encouraged to advise patients to register by calling 1-866-961-2388 or visiting online at https://womensmentalhealth.org/research/pregnancyregistry/atypicalantipsychotic/ . Risk Summary There are no available data on COBENFY use in pregnant women to evaluate for a drug-associated risk of major birth defects, miscarriage or other adverse maternal or fetal outcomes. There are risks to the mother associated with untreated schizophrenia (see Clinical Considerations). In animal reproduction studies, oral administration of xanomeline alone or in combination with trospium chloride during the period of organogenesis or during pregnancy and lactation caused maternal toxicities of adverse clinical signs, decreased body weight, weight gain and food consumption, and/or maternal death. At these maternally toxic doses, embryofetal and developmental toxicities included decreased fetal and neonatal weight, stillborn pups, and/or neonatal deaths. The no observed adverse effect level (NOAEL) of xanomeline or xanomeline/trospium chloride combination for maternal, embryofetal, and/or developmental toxicity is equal to or higher than the xanomeline and trospium chloride dose at the maximum recommended human dose (MRHD) of 250/60 mg xanomeline/trospium chloride, based on mg/m2 body surface area (BSA) (see Data). The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of major birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Clinical Considerations Disease-associated maternal and/or embryofetal risk There is a risk to the pregnant patient from untreated schizophrenia, including increased risk of relapse, hospitalization, and suicide. Schizophrenia is associated with adverse perinatal outcomes, including preterm birth. It is not known if this is a direct result of the illness or other comorbid factors. Data Animal Data Pregnant rats were orally treated during the period of organogenesis with 150 mg/kg/day xanomeline alone, 100 mg/kg/day trospium chloride alone, or xanomeline/trospium chloride combination at 30/25, 75/50, and 150/100 mg/kg/day, respectively. Xanomeline alone and the high dose combination caused maternal toxicities of decreased body weight, weight gain, and food consumption. At these maternally toxic doses, fetal weights were decreased. The NOAEL for maternal and embryofetal toxicity is 75/50 mg/kg/day for the combination, which is approximately 3 and 8 times the xanomeline and trospium chloride dose, respectively, at the MRHD of 250/60 mg xanomeline/trospium chloride, based on BSA. No fetal malformation was observed. Trospium chloride alone did not cause maternal or embryofetal toxicity. Pregnant rabbits were orally treated during the period of organogenesis with120 mg/kg/day xanomeline alone, 80 mg/kg/day trospium chloride alone, or xanomeline/trospium chloride combination at 30/20, 60/40, and 120/80 mg/kg/day, respectively. Xanomeline alone and the high dose combination caused maternal toxicities of decreased body weight, weight gain, and food consumption, and/or early abortion. At these maternally toxic doses, decreased fetal weight and decreased fetal viability (increased resorption and post-implantation loss) were observed. The NOAEL for maternal and embryofetal toxicity is 60/40 mg/kg/day for the xanomeline/trospium chloride combination, which is 5 and 13 times the xanomeline and trospium chloride dose, respectively at the MRHD, based on BSA. No fetal malformation was observed. Trospium chloride alone did not cause maternal or embryofetal toxicity. Rats were orally treated during pregnancy and lactation with 30, 75, and 150 mg/kg/day xanomeline alone, 100 mg/kg/day trospium chloride alone, or xanomeline/trospium chloride combination at 30/25, 75/50, and 150/100 mg/kg/day, respectively. Xanomeline alone at ≥ 75 mg/kg/day or in combination with trospium chloride at ≥ 75/50 mg/kg/day caused maternal toxicity of adverse clinical signs, decreased body weight, weight gain, food consumption, and maternal death. At these maternally toxic doses, developmental toxicity was observed in the offspring, including growth suppression (decreased body weight and weight gain), delayed developmental landmarks, stillborn pups, and neonatal deaths. No drug effect was observed on the neurobehavioral function, including learning and memory, or the reproductive capacity of the offspring. The NOAEL for maternal and developmental toxicity is 30/25 mg/kg/day for the xanomeline/trospium chloride combination, which is approximately 1 and 4 times the xanomeline and trospium chloride dose, respectively at the MRHD, based on BSA. Trospium chloride alone did not cause maternal or developmental toxicity. Pregnant rats were treated during the period of organogenesis with trospium chloride at doses up to 200 mg/kg/day. No malformation or fetal toxicity was observed up to 200 mg/kg/day, which is approximately 32 times the trospium chloride dose at the MRHD of 250/60 mg xanomeline/trospium chloride based on BSA. Pregnant rabbits were treated during the period of organogenesis with trospium chloride at doses up to 200 mg/kg/day. Maternal toxicity (reduced feces, hunched posture, and diarrhea) was observed at 200 mg/kg/day. The NOAEL for maternal toxicity is 20 mg/kg/day, which is approximately 3 times the trospium chloride dose at the MRHD based on BSA. Rats were orally treated during pregnancy and lactation with trospium chloride at doses up to 200 mg/kg/day. Maternal toxicity (death, irregular breathing, increased excitability) and neonatal deaths were observed at 200 mg/kg/day, which is approximately 32 times the MRHD, based on BSA. The NOAEL for maternal and developmental toxicity is 20 mg/kg/day, which is approximately 3 times the trospium chloride dose at the MRHD, based BSA.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS • Moderate or Severe Renal Impairment: Not recommended. ( 8.6 ) • Mild Hepatic Impairment: Not recommended. ( 8.7 ) 8.1 Pregnancy Pregnancy Exposure Registry There is a pregnancy exposure registry that monitors outcomes in women exposed to psychiatric medications, including COBENFY, during pregnancy. Healthcare providers are encouraged to advise patients to register by calling 1-866-961-2388 or visiting online at https://womensmentalhealth.org/research/pregnancyregistry/atypicalantipsychotic/ . Risk Summary There are no available data on COBENFY use in pregnant women to evaluate for a drug-associated risk of major birth defects, miscarriage or other adverse maternal or fetal outcomes. There are risks to the mother associated with untreated schizophrenia (see Clinical Considerations). In animal reproduction studies, oral administration of xanomeline alone or in combination with trospium chloride during the period of organogenesis or during pregnancy and lactation caused maternal toxicities of adverse clinical signs, decreased body weight, weight gain and food consumption, and/or maternal death. At these maternally toxic doses, embryofetal and developmental toxicities included decreased fetal and neonatal weight, stillborn pups, and/or neonatal deaths. The no observed adverse effect level (NOAEL) of xanomeline or xanomeline/trospium chloride combination for maternal, embryofetal, and/or developmental toxicity is equal to or higher than the xanomeline and trospium chloride dose at the maximum recommended human dose (MRHD) of 250/60 mg xanomeline/trospium chloride, based on mg/m2 body surface area (BSA) (see Data). The background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of major birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Clinical Considerations Disease-associated maternal and/or embryofetal risk There is a risk to the pregnant patient from untreated schizophrenia, including increased risk of relapse, hospitalization, and suicide. Schizophrenia is associated with adverse perinatal outcomes, including preterm birth. It is not known if this is a direct result of the illness or other comorbid factors. Data Animal Data Pregnant rats were orally treated during the period of organogenesis with 150 mg/kg/day xanomeline alone, 100 mg/kg/day trospium chloride alone, or xanomeline/trospium chloride combination at 30/25, 75/50, and 150/100 mg/kg/day, respectively. Xanomeline alone and the high dose combination caused maternal toxicities of decreased body weight, weight gain, and food consumption. At these maternally toxic doses, fetal weights were decreased. The NOAEL for maternal and embryofetal toxicity is 75/50 mg/kg/day for the combination, which is approximately 3 and 8 times the xanomeline and trospium chloride dose, respectively, at the MRHD of 250/60 mg xanomeline/trospium chloride, based on BSA. No fetal malformation was observed. Trospium chloride alone did not cause maternal or embryofetal toxicity. Pregnant rabbits were orally treated during the period of organogenesis with120 mg/kg/day xanomeline alone, 80 mg/kg/day trospium chloride alone, or xanomeline/trospium chloride combination at 30/20, 60/40, and 120/80 mg/kg/day, respectively. Xanomeline alone and the high dose combination caused maternal toxicities of decreased body weight, weight gain, and food consumption, and/or early abortion. At these maternally toxic doses, decreased fetal weight and decreased fetal viability (increased resorption and post-implantation loss) were observed. The NOAEL for maternal and embryofetal toxicity is 60/40 mg/kg/day for the xanomeline/trospium chloride combination, which is 5 and 13 times the xanomeline and trospium chloride dose, respectively at the MRHD, based on BSA. No fetal malformation was observed. Trospium chloride alone did not cause maternal or embryofetal toxicity. Rats were orally treated during pregnancy and lactation with 30, 75, and 150 mg/kg/day xanomeline alone, 100 mg/kg/day trospium chloride alone, or xanomeline/trospium chloride combination at 30/25, 75/50, and 150/100 mg/kg/day, respectively. Xanomeline alone at ≥ 75 mg/kg/day or in combination with trospium chloride at ≥ 75/50 mg/kg/day caused maternal toxicity of adverse clinical signs, decreased body weight, weight gain, food consumption, and maternal death. At these maternally toxic doses, developmental toxicity was observed in the offspring, including growth suppression (decreased body weight and weight gain), delayed developmental landmarks, stillborn pups, and neonatal deaths. No drug effect was observed on the neurobehavioral function, including learning and memory, or the reproductive capacity of the offspring. The NOAEL for maternal and developmental toxicity is 30/25 mg/kg/day for the xanomeline/trospium chloride combination, which is approximately 1 and 4 times the xanomeline and trospium chloride dose, respectively at the MRHD, based on BSA. Trospium chloride alone did not cause maternal or developmental toxicity. Pregnant rats were treated during the period of organogenesis with trospium chloride at doses up to 200 mg/kg/day. No malformation or fetal toxicity was observed up to 200 mg/kg/day, which is approximately 32 times the trospium chloride dose at the MRHD of 250/60 mg xanomeline/trospium chloride based on BSA. Pregnant rabbits were treated during the period of organogenesis with trospium chloride at doses up to 200 mg/kg/day. Maternal toxicity (reduced feces, hunched posture, and diarrhea) was observed at 200 mg/kg/day. The NOAEL for maternal toxicity is 20 mg/kg/day, which is approximately 3 times the trospium chloride dose at the MRHD based on BSA. Rats were orally treated during pregnancy and lactation with trospium chloride at doses up to 200 mg/kg/day. Maternal toxicity (death, irregular breathing, increased excitability) and neonatal deaths were observed at 200 mg/kg/day, which is approximately 32 times the MRHD, based on BSA. The NOAEL for maternal and developmental toxicity is 20 mg/kg/day, which is approximately 3 times the trospium chloride dose at the MRHD, based BSA. 8.2 Lactation Risk Summary There are no data on the presence of xanomeline or trospium in human milk, the effects on the breastfed infant, or the effects on milk production. Xanomeline and trospium are present in animal milk. When a drug is present in animal milk, it is likely that the drug will be present in human milk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for COBENFY and any potential adverse effects on the breastfed infant from COBENFY or from the underlying maternal condition. 8.4 Pediatric Use The safety and effectiveness of COBENFY in pediatric patients have not been established. 8.5 Geriatric Use Controlled clinical studies of COBENFY did not include patients older than 65 years of age to determine whether they respond differently from younger adult patients. Because COBENFY can increase the risk of urinary retention in geriatric patients, including older males with bladder outlet obstruction due to benign prostatic hyperplasia (BPH), a slower titration and lower maximum dosage is recommended in geriatric patients [see Dosage and Administration (2.3) and Warnings and Precautions (5.1) ] . 8.6 Renal Impairment Patients with mild renal impairment (eGFR 60 to <90 mL/min) showed higher systemic exposures to trospium chloride and xanomeline, the components of COBENFY, compared to subjects with normal renal function. However, in the adequate and well-controlled clinical studies, the safety profiles in patients with mild renal impairment were similar to those observed in patients with normal renal function (eGFR ≥90 mL/min). Therefore, the recommended dosage in patients with mild renal impairment is the same as the recommended dosage for patients with normal renal function. Use of COBENFY is not recommended in patients with moderate or severe renal impairment (eGFR<60 mL/min) [see Warnings and Precautions (5.1 , 5.8) and Clinical Pharmacology (12.3) ] . 8.7 Hepatic Impairment Patients with mild to moderate hepatic impairment (Child-Pugh Class A and B, respectively) have higher xanomeline exposures compared to patients with normal hepatic function [see Clinical Pharmacology (12.3) ] . The pharmacokinetics of COBENFY were not studied in patients with severe hepatic impairment (Child-Pugh Class C). Use of COBENFY is contraindicated in patients moderate or severe hepatic impairment [see Contraindications (4) and Warnings and Precautions (5.2) ] . It is not recommended in patients with mild hepatic impairment.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING How Supplied COBENFY is available as: • 50 mg/20 mg (xanomeline/trospium chloride): Buff capsules imprinted with Karuna 50/20 mg • 100 mg/20 mg (xanomeline/trospium chloride): Brown capsules imprinted with Karuna 100/20 mg • 125 mg/30 mg (xanomeline/trospium chloride): Swedish Orange capsules imprinted with Karuna 125/30 mg COBENFY capsules are packaged as described in Table 5. Table 5: COBENFY Packaging Configurations Capsule Strength Total Package Count Package Configuration Package Components NDC Code 50 mg/20 mg 60 Bottle N/A 0003-0050-60 100 mg/20 mg 60 Bottle N/A 0003-1100-60 125 mg/30 mg 60 Bottle N/A 0003-0125-60 50 mg/20 mg (4) 100 mg/20 mg (52) 56 Starter Pack for 100 mg/20 mg dose 1 Mixed Blister Wallet: four (4) 50 mg/20 mg capsules and ten (10) 100 mg/20 mg capsules and 3 Wallets: fourteen (14) 100 mg/20 mg capsules in each wallet 0003-5200-56 Storage and Handling Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature].
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API