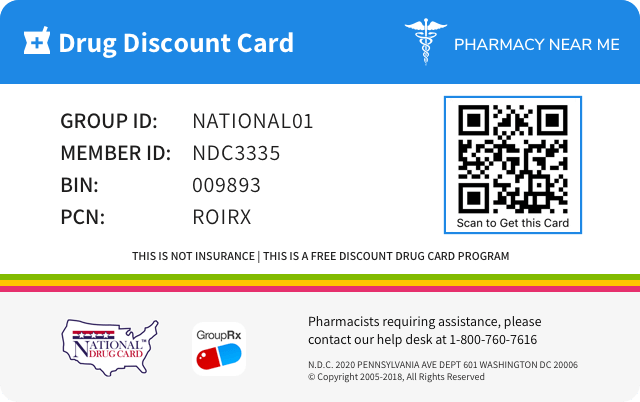
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 82667-800 | ||||
|---|---|---|---|---|---|
| Drug Name | Triesence |
||||
| Type | Brand | ||||
| Pharm Class | Corticosteroid Hormone Receptor Agonists [MoA], Corticosteroid [EPC] |
||||
| Active Ingredients |
|
||||
| Route | OPHTHALMIC | ||||
| Dosage Form | INJECTION, SUSPENSION | ||||
| RxCUI drug identifier | 1086259, 1792144 |
||||
| Application Number | NDA022048 | ||||
| Labeler Name | Harrow Eye, LLC | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. Adverse event data were collected from 300 published articles containing data from controlled and uncontrolled clinical trials which evaluated over 14000 eyes treated with different concentrations of triamcinolone acetonide. The most common dose administered within these trials was triamcinolone acetonide 4 mg administered as primary or adjunctive therapy primarily as a single injection. The most common reported adverse events following administration of triamcinolone acetonide were elevated IOP and cataract progression. These events have been reported to occur in 20% to 60% of patients. Less common reactions occurring in up to 2% include endophthalmitis (infectious and non-infectious), hypopyon, injection site reactions (described as blurring and transient discomfort), glaucoma, vitreous floaters, and detachment of retinal pigment epithelium, optic disc vascular disorder, eye inflammation, conjunctival hemorrhage, and visual acuity reduced. Cases of exophthalmos have also been reported. Common adverse reactions for systemically administered corticosteroids include fluid retention, alteration in glucose tolerance, elevation in blood pressure, behavioral and mood changes, increased appetite, and weight gain. Other reactions reported to have occurred with the administration of corticosteroids include: Allergic Reactions: Anaphylactoid reaction, anaphylaxis, angioedema Cardiovascular: Bradycardia, cardiac arrest, cardiac arrhythmias, cardiac enlargement, circulatory collapse, congestive heart failure, fat embolism, hypertrophic cardiomyopathy in premature infants, myocardial rupture following recent myocardial infarction, pulmonary edema, syncope, tachycardia, thromboembolism, thrombophlebitis, vasculitis Dermatologic: Acne, allergic dermatitis, cutaneous and subcutaneous atrophy, dry scalp, edema, facial erythema, hyper or hypo-pigmentation, impaired wound healing, increased sweating, petechiae and ecchymoses, rash, sterile abscess, striae, suppressed reactions to skin tests, thin fragile skin, thinning scalp hair, urticaria Endocrine: Abnormal fat deposits, decreased carbohydrate tolerance, development of Cushingoid state, hirsutism, manifestations of latent diabetes mellitus and increased requirements for insulin or oral hypoglycemic agents in diabetics, menstrual irregularities, moon facies, secondary adrenocortical and pituitary unresponsiveness (particularly in times of stress, as in trauma, surgery or illness), suppression of growth in children Fluid and Electrolyte Disturbances: Potassium loss, hypokalemic alkalosis, sodium retention Gastrointestinal: Abdominal distention, elevation in serum liver enzymes levels (usually reversible upon discontinuation), hepatomegaly, hiccups, malaise, nausea, pancreatitis, peptic ulcer with possible perforation and hemorrhage, ulcerative esophagitis Metabolic: Negative nitrogen balance due to protein catabolism Musculoskeletal: Aseptic necrosis of femoral and humeral heads, charcot-like arthropathy, loss of muscle mass, muscle weakness, osteoporosis, pathologic fracture of long bones, steroid myopathy, tendon rupture, vertebral compression fractures Neurological: Arachnoiditis, convulsions, depression, emotional instability, euphoria, headache, increased intracranial pressure with papilledema (pseudo-tumor cerebri) usually following discontinuation of treatment, insomnia, meningitis, neuritis, neuropathy, paraparesis/paraplegia, paresthesia, sensory disturbances, vertigo Reproductive: Alteration in motility and number of spermatozoa
TRIESENCE Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS • Amphotericin B: There have been cases reported in which concomitant use of Amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure (s ee Potassium Depleting Agents). • Anticholinesterase agents: Concomitant use of anticholinesterase agents and corticosteroids may produce severe weakness in patients with myasthenia gravis. If possible, anticholinesterase agents should be withdrawn at least 24 hours before initiating corticosteroid therapy. • Anticoagulant agents: Coadministration of corticosteroids and warfarin usually results in inhibition of response to warfarin, although there have been some conflicting reports. Therefore, coagulation indices should be monitored frequently to maintain the desired anticoagulant effect. • Antidiabetic agents: Because corticosteroids may increase blood glucose concentrations, dosage adjustments of antidiabetic agents may be required. • Antitubercular drugs: Serum concentrations of isoniazid may be decreased. • CYP 3A4 inducers (e.g., barbiturates, phenytoin, carbamazepine, and rifampin): Drugs, such as barbiturates, phenytoin, ephedrine, and rifampin, which induce hepatic microsomal drug metabolizing enzyme activity may enhance metabolism of corticosteroid and require that the dosage of corticosteroid be increased. • CYP 3A4 inhibitors (e.g., ketoconazole, macrolide antibiotics): Ketoconazole has been reported to decrease the metabolism of certain corticosteroids by up to 60% leading to an increased risk of corticosteroid side effects. • Cholestyramine: Cholestyramine may increase the clearance of corticosteroids. • Cyclosporine: Increased activity of both cyclosporine and corticosteroids may occur when the two are used concurrently. Convulsions have been reported with concurrent use. • Digitalis: Patients on digitalis glycosides may be at increased risk of arrhythmias due to hypokalemia. • Estrogens, including oral contraceptives: Estrogens may decrease the hepatic metabolism of certain corticosteroids thereby increasing their effect. • NSAIDs including aspirin and salicylates: Concomitant use of aspirin or other non-steroidal antiinflammatory agents and corticosteroids increases the risk of gastrointestinal side effects. Aspirin should be used cautiously in conjunction with corticosteroids in hypoprothrombinemia. The clearance of salicylates may be increased with concurrent use of corticosteroids. • Potassium depleting agents (e.g., diuretics, Amphotericin B): When corticosteroids are administered concomitantly with potassium-depleting agents, patients should be observed closely for development of hypokalemia. • Skin tests: Corticosteroids may suppress reactions to skin tests. • Toxoids and live or inactivated vaccines: Due to inhibition of antibody response, patients on prolonged corticosteroid therapy may exhibit a diminished response to toxoids and live or inactivated vaccines. Corticosteroids may also potentiate the replication of some organisms contained in live attenuated vaccines. • Anticoagulant agents: May enhance or diminish anticoagulant effects. Monitor coagulation indices. ( 7 ) • Antidiabetic agents: May increase blood glucose concentrations. Dose adjustments of antidiabetic agents may be required. ( 7 ) • CYP 3A4 inducers and inhibitors: May respectively increase or decrease clearance of corticosteroids necessitating dose adjustment. ( 7 ) • Non-steroidal anti inflammatory drugs (NSAIDs), including aspirin and salicylates: Increased risk of gastrointestinal side effects. ( 7 )
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs, such as prednisolone and triamcinolone are primarily used for their anti-inflammatory effects in disorders of many organ systems. Triamcinolone acetonide possesses glucocorticoid activity typical of this class of drug, but with little or no mineralocorticoid activity. For the purposes of comparison, the following is the equivalent milligram dosage of the various glucocorticoids: Cortisone, 25 Prednisone, 5 Paramethasone, 2 Hydrocortisone, 20 Methylprednisolone, 4 Betamethasone, 0.75 Prednisolone, 5 Triamcinolone, 4 Dexamethasone, 0.75 Corticosteroids have been demonstrated to depress the production of eosinophils and lymphocytes, but erythropoiesis and production of polymorphonuclear leukocytes are stimulated. Inflammatory processes (edema, fibrin deposition, capillary dilatation, migration of leukocytes and phagocytosis) and the later stages of wound healing (capillary proliferation, deposition of collagen, cicatrization) are inhibited. 12.3 Pharmacokinetics Aqueous humor pharmacokinetics of triamcinolone have been assessed in 5 patients following a single intravitreal administration (4 mg) of triamcinolone acetonide. Aqueous humor samples were obtained from 5 patients (5 eyes) via an anterior chamber paracentesis on Days 1, 3, 10, 17, and 31 postinjection. Peak aqueous humor concentrations of triamcinolone ranged from 2151 to 7202 ng/mL, half-life 76 to 635 hours, and the area under the concentration-time curve (AUC 0-t ) from 231 to 1911 ng.h/mL following the single intravitreal administration. The mean elimination half-life was 18.7 ± 5.7 days in 4 nonvitrectomized eyes (4 patients). In a patient who had undergone vitrectomy (1 eye), the elimination half-life of triamcinolone from the vitreous was much faster (3.2 days) relative to patients that had not undergone vitrectomy.
| Cortisone, 25 | Prednisone, 5 | Paramethasone, 2 |
| Hydrocortisone, 20 | Methylprednisolone, 4 | Betamethasone, 0.75 |
| Prednisolone, 5 | Triamcinolone, 4 | Dexamethasone, 0.75 |
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action Naturally occurring glucocorticoids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs, such as prednisolone and triamcinolone are primarily used for their anti-inflammatory effects in disorders of many organ systems. Triamcinolone acetonide possesses glucocorticoid activity typical of this class of drug, but with little or no mineralocorticoid activity. For the purposes of comparison, the following is the equivalent milligram dosage of the various glucocorticoids: Cortisone, 25 Prednisone, 5 Paramethasone, 2 Hydrocortisone, 20 Methylprednisolone, 4 Betamethasone, 0.75 Prednisolone, 5 Triamcinolone, 4 Dexamethasone, 0.75 Corticosteroids have been demonstrated to depress the production of eosinophils and lymphocytes, but erythropoiesis and production of polymorphonuclear leukocytes are stimulated. Inflammatory processes (edema, fibrin deposition, capillary dilatation, migration of leukocytes and phagocytosis) and the later stages of wound healing (capillary proliferation, deposition of collagen, cicatrization) are inhibited.
| Cortisone, 25 | Prednisone, 5 | Paramethasone, 2 |
| Hydrocortisone, 20 | Methylprednisolone, 4 | Betamethasone, 0.75 |
| Prednisolone, 5 | Triamcinolone, 4 | Dexamethasone, 0.75 |
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Aqueous humor pharmacokinetics of triamcinolone have been assessed in 5 patients following a single intravitreal administration (4 mg) of triamcinolone acetonide. Aqueous humor samples were obtained from 5 patients (5 eyes) via an anterior chamber paracentesis on Days 1, 3, 10, 17, and 31 postinjection. Peak aqueous humor concentrations of triamcinolone ranged from 2151 to 7202 ng/mL, half-life 76 to 635 hours, and the area under the concentration-time curve (AUC 0-t ) from 231 to 1911 ng.h/mL following the single intravitreal administration. The mean elimination half-life was 18.7 ± 5.7 days in 4 nonvitrectomized eyes (4 patients). In a patient who had undergone vitrectomy (1 eye), the elimination half-life of triamcinolone from the vitreous was much faster (3.2 days) relative to patients that had not undergone vitrectomy.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS Corticosteroids are contraindicated in patients with systemic fungal infections. Triamcinolone is contraindicated in patients who are hypersensitive to corticosteroids or any components of this product. Rare instances of anaphylactoid reactions have occurred in patients receiving corticosteroid therapy. [ see Adverse Reactions (6) ]. • Patients with systemic fungal infections. ( 4 ) • Hypersensitivity to triamcinolone or any component of this product. ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION TRIESENCE (triamcinolone acetonide injectable suspension) 40 mg/mL is a synthetic corticosteroid with anti-inflammatory action. Each mL of the sterile, aqueous suspension provides 40 mg of triamcinolone acetonide, with sodium chloride for isotonicity, 0.5% (w/v) carboxymethylcellulose sodium and 0.015% polysorbate 80. It also contains calcium chloride (dihydrate), magnesium chloride (hexahydrate), potassium chloride, sodium acetate (trihydrate), sodium citrate (dihydrate) and water for injection. Sodium hydroxide and hydrochloric acid may be present to adjust pH to a target value 6 - 7.5. The chemical name for triamcinolone acetonide is 9-Fluro- 11β, 16α, 17,21-tetrahydroxypregna-1,4-diene-3,20-dione cyclic 16,17- acetal with acetone. Its structural formula of C 24 H 31 FO 6 is: 434.50 g/mol Molecular Weight Triamcinolone acetonide occurs as a white to cream-colored, crystalline powder having not more than a slight odor and is practically insoluble in water and very soluble in alcohol. chemical
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION • Initial recommended dose for all indications except visualization: 4 mg (100 microliters of 40 mg/mL suspension) with subsequent dosage as needed over the course of treatment. ( 2.1 ) • Recommended dose for visualization: 1 to 4 mg (25 to 100 microliters of 40 mg/mL suspension) administered intravitreally. ( 2.2 ) 2.1 Dosage for Treatment of Ophthalmic Diseases The initial recommended dose of TRIESENCE suspension is 4 mg (100 microliters of 40 mg/mL suspension) with subsequent dosage as needed over the course of treatment. 2.2 Dosage for Visualization During Vitrectomy The recommended dose of TRIESENCE ® suspension is 1 to 4 mg (25 to 100 microliters of 40 mg/mL suspension) administered intravitreally. 2.3 Preparation for Administration STRICT ASEPTIC TECHNIQUE IS MANDATORY. The vial should be vigorously shaken for 10 seconds before use to ensure a uniform suspension. Prior to withdrawal, the suspension should be inspected for clumping or granular appearance (agglomeration). An agglomerated product results from exposure to freezing temperatures and should not be used. After withdrawal, TRIESENCE suspension should be injected without delay to prevent settling in the syringe. Careful technique should be employed to avoid the possibility of entering a blood vessel or introducing organisms that can cause infection. 2.4 Administration The injection procedure should be carried out under controlled aseptic conditions, which include the use of sterile gloves, a sterile drape, and a sterile eyelid speculum (or equivalent). Adequate anesthesia and a broad-spectrum microbicide should be given prior to the injection. Following the injection, patients should be monitored for elevation in intraocular pressure (IOP) and for endophthalmitis. Monitoring may consist of a check for perfusion of the optic nerve head immediately after the injection, tonometry within 30 minutes following the injection, and biomicroscopy between two and seven days following the injection. Patients should be instructed to report any symptoms suggestive of endophthalmitis without delay. Each vial should only be used for the treatment of a single eye. If the contralateral eye requires treatment, a new vial should be used and the sterile field, syringe, gloves, drapes, eyelid speculum, and injection needles should be changed before TRIESENCE suspension is administered to the other eye.
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Single use 1 mL vial containing 40 mg/mL of sterile triamcinolone acetonide suspension. Single use 1 mL vial containing 40 mg/mL of triamcinolone acetonide suspension. ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE TRIESENCE suspension is a synthetic corticosteroid indicated for: • Treatment of the following ophthalmic diseases: sympathetic ophthalmia, temporal arteritis, uveitis, and ocular inflammatory conditions unresponsive to topical corticosteroids. ( 1.1 ) • Visualization during vitrectomy. ( 1.2 ) 1.1 Ophthalmic Diseases TRIESENCE (triamcinolone acetonide injectable suspension) 40 mg/mL is indicated for: • sympathetic ophthalmia, • temporal arteritis, • uveitis, and • ocular inflammatory conditions unresponsive to topical corticosteroids. 1.2 Visualization During Vitrectomy TRIESENCE suspension is indicated for visualization during vitrectomy.
Spl product data elements
Usually a list of ingredients in a drug product.TRIESENCE triamcinolone acetonide SODIUM CHLORIDE CARBOXYMETHYLCELLULOSE SODIUM POLYSORBATE 80 POTASSIUM CHLORIDE CALCIUM CHLORIDE MAGNESIUM CHLORIDE SODIUM ACETATE SODIUM CITRATE WATER SODIUM HYDROXIDE HYDROCHLORIC ACID TRIAMCINOLONE ACETONIDE TRIAMCINOLONE ACETONIDE
Animal pharmacology and or toxicology
Information from studies of the drug in animals, if the data were not relevant to nor included in other parts of the labeling. Most labels do not contain this field.13.2 Animal Toxicology and/or Pharmacology Studies were conducted with triamcinolone acetonide, including those employing the proposed dosage form, i.e., 4.0% triamcinolone acetonide injectable suspension formulation containing 0.5% carboxymethylcellulose and 0.015% polysorbate-80 in a balanced salt solution. Triamcinolone acetonide was demonstrated to be non-inflammatory when injected intravitreally in New Zealand White NZW rabbits, non-cytotoxic to mouse L-929 cells in an in vitro assay and non-sensitizing in a guinea-pig maximization assay. Furthermore, the results of single-dose intravitreal injection studies with triamcinolone acetonide in both rabbits and monkeys demonstrate that the drug is well tolerated for up to one month with only minor findings of slight decrease in body weight gain and slight corneal thinning.
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility No evidence of mutagenicity was detected from in vitro tests conducted with triamcinolone acetonide, including a reverse mutation test in Salmonella bacteria and a forward mutation test in Chinese hamster ovary cells. With regard to carcinogenicity, in a two-year study in rats, triamcinolone acetonide caused no treatment-related carcinogenicity at oral doses up to 0.001 mg/kg and in a two-year study in mice, triamcinolone acetonide caused no treatment-related carcinogenicity at oral doses up to 0.003 mg/kg (less than 1/25th of the recommended human dose). In male and female rats, triamcinolone acetonide caused no change in pregnancy rate at oral doses up to 0.015 mg/kg, but caused increased fetal resorptions and stillbirths and decreases in pup weight and survival at doses of 0.005 mg/kg (less than 1/10th of the recommended human dose).
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility No evidence of mutagenicity was detected from in vitro tests conducted with triamcinolone acetonide, including a reverse mutation test in Salmonella bacteria and a forward mutation test in Chinese hamster ovary cells. With regard to carcinogenicity, in a two-year study in rats, triamcinolone acetonide caused no treatment-related carcinogenicity at oral doses up to 0.001 mg/kg and in a two-year study in mice, triamcinolone acetonide caused no treatment-related carcinogenicity at oral doses up to 0.003 mg/kg (less than 1/25th of the recommended human dose). In male and female rats, triamcinolone acetonide caused no change in pregnancy rate at oral doses up to 0.015 mg/kg, but caused increased fetal resorptions and stillbirths and decreases in pup weight and survival at doses of 0.005 mg/kg (less than 1/10th of the recommended human dose). 13.2 Animal Toxicology and/or Pharmacology Studies were conducted with triamcinolone acetonide, including those employing the proposed dosage form, i.e., 4.0% triamcinolone acetonide injectable suspension formulation containing 0.5% carboxymethylcellulose and 0.015% polysorbate-80 in a balanced salt solution. Triamcinolone acetonide was demonstrated to be non-inflammatory when injected intravitreally in New Zealand White NZW rabbits, non-cytotoxic to mouse L-929 cells in an in vitro assay and non-sensitizing in a guinea-pig maximization assay. Furthermore, the results of single-dose intravitreal injection studies with triamcinolone acetonide in both rabbits and monkeys demonstrate that the drug is well tolerated for up to one month with only minor findings of slight decrease in body weight gain and slight corneal thinning.
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.NDC 82667-800-01 Sterile Triesence ® (triamcinolone acetonide injectable suspension) 40 mg/mL Preservative Free 1 mL HARROW ® Carton.jpg
Spl unclassified section
Information not classified as belonging to one of the other fields. Approximately 40% of labeling with effective_time between June 2009 and August 2014 have information in this field.Distributed by: Harrow Eye, LLC™ Nashville, TN 37205 USA
TRIESENCE: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Patients should discuss with their physician if they have had recent or ongoing infections or if they have recently received a vaccine. There are a number of medicines that can interact with corticosteroids, such as triamcinolone. Patients should inform their health-care provider of all the medicines they are taking, including over-the-counter and prescription medicines (such as phenytoin, diuretics, digitalis or digoxin, rifampin, amphotericin B, cyclosporine, insulin or diabetes medicines, ketoconazole, estrogens, including birth control pills and hormone replacement therapy, blood thinners, such as warfarin, aspirin or other NSAIDs, barbiturates), dietary supplements, and herbal products. If patients are taking any of these drugs, alternate therapy, dosage adjustment, and/or special test may be needed during the treatment. Patients should be advised of common adverse reactions that could occur with corticosteroid use to include elevated IOP, cataracts, fluid retention, alteration in glucose tolerance, elevation in blood pressure, behavioral and mood changes, increased appetite and weight gain.
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use No overall differences in safety or effectiveness were observed between elderly subjects and younger subjects, and other reported clinical experience with triamcinolone has not identified differences in responses between the elderly and younger patients. However, the incidence of corticosteroid-induced side effects may be increased in geriatric patients and are dose-related. Osteoporosis is the most frequently encountered complication, which occurs at a higher incidence rate in corticosteroid-treated geriatric patients as compared to younger populations and in age-matched controls. Losses of bone mineral density appear to be greatest early on in the course of treatment and may recover over time after steroid withdrawal or use of lower doses.
Nursing mothers
Information about excretion of the drug in human milk and effects on the nursing infant, including pertinent adverse effects observed in animal offspring.8.3 Nursing Mothers Corticosteroids are secreted in human milk. Reports suggest that steroid concentrations in human milk are 5% to 25% of maternal serum levels, and that total infant daily doses are small, less than 0.2% of the maternal daily dose. The risk of infant exposure to steroids through breast milk should be weighed against the known benefits of breastfeeding for both the mother and baby.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use The efficacy and safety of corticosteroids in the pediatric population are based on the well established course of effect of corticosteroids which is similar in pediatric and adult populations. The adverse effects of corticosteroids in pediatric patients are similar to those in adults. [see Adverse Reactions (6) ] . Like adults, pediatric patients should be carefully observed with frequent measurements of blood pressure, weight, height, IOP, and clinical evaluation for the presence of infection, psychosocial disturbances, thromboembolism, peptic ulcers, cataracts, and osteoporosis. Children, who are treated with corticosteroids by any route, including systemically administered corticosteroids, may experience a decrease in their growth velocity. This negative impact of corticosteroids on growth has been observed at low systemic doses and in the absence of laboratory evidence of HPA axis suppression (i.e., cosyntropin stimulation and basal cortisol plasma levels). Growth velocity may therefore be a more sensitive indicator of systemic corticosteroid exposure in children than some commonly used tests of HPA axis function. The linear growth of children treated with corticosteroids by any route should be monitored, and the potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of other treatment alternatives. In order to minimize the potential growth effects of corticosteroids, children should be titrated to the lowest effective dose.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Teratogenic Effects: Pregnancy Category D [see Warnings and Precautions (5.10) ] Multiple cohort and case controlled studies in humans suggest that maternal corticosteroid use during the first trimester increases the rate of cleft lip with or without cleft palate from about 1/1000 infants to 3- 5/1000 infants. Two prospective case control studies showed decreased birth weight in infants exposed to maternal corticosteroids in utero. Triamcinolone acetonide was teratogenic in rats, rabbits, and monkeys. In rats and rabbits, triamcinolone acetonide was teratogenic at inhalation doses of 0.02 mg/kg and above and in monkeys, triamcinolone acetonide was teratogenic at an inhalation dose of 0.5 mg/kg (1/4 and 7 times the recommended human dose). Dose-related teratogenic effects in rats and rabbits included cleft palate and/or internal hydrocephaly and axial skeletal defects, whereas the effects observed in monkeys were cranial malformations. These effects are similar to those noted with other corticosteroids. Corticosteroids should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Infants born to mothers who received corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Teratogenic Effects: Pregnancy Category D [see Warnings and Precautions (5.10) ] Multiple cohort and case controlled studies in humans suggest that maternal corticosteroid use during the first trimester increases the rate of cleft lip with or without cleft palate from about 1/1000 infants to 3- 5/1000 infants. Two prospective case control studies showed decreased birth weight in infants exposed to maternal corticosteroids in utero. Triamcinolone acetonide was teratogenic in rats, rabbits, and monkeys. In rats and rabbits, triamcinolone acetonide was teratogenic at inhalation doses of 0.02 mg/kg and above and in monkeys, triamcinolone acetonide was teratogenic at an inhalation dose of 0.5 mg/kg (1/4 and 7 times the recommended human dose). Dose-related teratogenic effects in rats and rabbits included cleft palate and/or internal hydrocephaly and axial skeletal defects, whereas the effects observed in monkeys were cranial malformations. These effects are similar to those noted with other corticosteroids. Corticosteroids should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Infants born to mothers who received corticosteroids during pregnancy should be carefully observed for signs of hypoadrenalism. 8.3 Nursing Mothers Corticosteroids are secreted in human milk. Reports suggest that steroid concentrations in human milk are 5% to 25% of maternal serum levels, and that total infant daily doses are small, less than 0.2% of the maternal daily dose. The risk of infant exposure to steroids through breast milk should be weighed against the known benefits of breastfeeding for both the mother and baby. 8.4 Pediatric Use The efficacy and safety of corticosteroids in the pediatric population are based on the well established course of effect of corticosteroids which is similar in pediatric and adult populations. The adverse effects of corticosteroids in pediatric patients are similar to those in adults. [see Adverse Reactions (6) ] . Like adults, pediatric patients should be carefully observed with frequent measurements of blood pressure, weight, height, IOP, and clinical evaluation for the presence of infection, psychosocial disturbances, thromboembolism, peptic ulcers, cataracts, and osteoporosis. Children, who are treated with corticosteroids by any route, including systemically administered corticosteroids, may experience a decrease in their growth velocity. This negative impact of corticosteroids on growth has been observed at low systemic doses and in the absence of laboratory evidence of HPA axis suppression (i.e., cosyntropin stimulation and basal cortisol plasma levels). Growth velocity may therefore be a more sensitive indicator of systemic corticosteroid exposure in children than some commonly used tests of HPA axis function. The linear growth of children treated with corticosteroids by any route should be monitored, and the potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of other treatment alternatives. In order to minimize the potential growth effects of corticosteroids, children should be titrated to the lowest effective dose. 8.5 Geriatric Use No overall differences in safety or effectiveness were observed between elderly subjects and younger subjects, and other reported clinical experience with triamcinolone has not identified differences in responses between the elderly and younger patients. However, the incidence of corticosteroid-induced side effects may be increased in geriatric patients and are dose-related. Osteoporosis is the most frequently encountered complication, which occurs at a higher incidence rate in corticosteroid-treated geriatric patients as compared to younger populations and in age-matched controls. Losses of bone mineral density appear to be greatest early on in the course of treatment and may recover over time after steroid withdrawal or use of lower doses.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING TRIESENCE (triamcinolone acetonide injectable suspension) 40 mg/mL is supplied as 1 mL of a 40 mg/mL sterile triamcinolone acetonide suspension in a flint Type 1 single use glass vial with a gray rubber stopper and an open target aluminum seal. Each labeled vial is sealed in a polycarbonate blister with a backing material which provides tamper evidence and is stored in a carton. • 1 mL single use vial NDC 82667-800-01 Storage Store at 4°C to 25°C (39°F to 77°F); Do Not Freeze. Protect from light by storing in carton.
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API