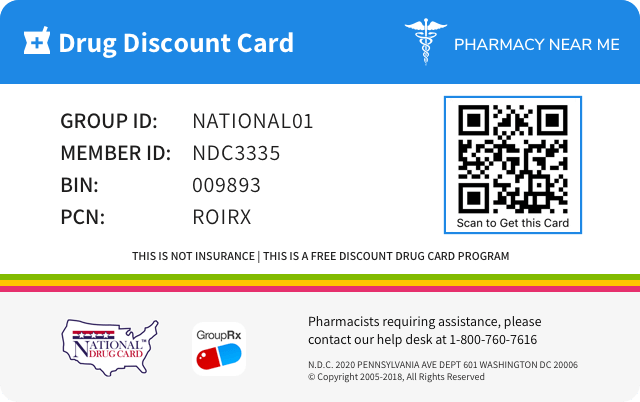
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 75987-021 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug Name | Rayos |
||||||||
| Type | Brand | ||||||||
| Pharm Class | Corticosteroid Hormone Receptor Agonists [MoA], Corticosteroid [EPC] |
||||||||
| Active Ingredients |
|
||||||||
| Route | ORAL | ||||||||
| Dosage Form | TABLET, DELAYED RELEASE | ||||||||
| RxCUI drug identifier | 1303125, 1303131, 1303132, 1303134, 1303135, 1303137 |
||||||||
| Application Number | NDA202020 | ||||||||
| Labeler Name | Horizon Therapeutics USA, Inc. | ||||||||
| Packages |
|
||||||||
| Check if available Online | Get Medication Prices online with Discount |
Overdosage of RAYOS
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE The effects of accidental ingestion of large quantities of prednisone over a very short period of time have not been reported, but prolonged use of the drug can produce mental symptoms, moon face, abnormal fat deposits, fluid retention, excessive appetite, weight gain, hypertrichosis, acne, striae, ecchymosis, increased sweating, pigmentation, dry scaly skin, thinning scalp hair, increased blood pressure, tachycardia, thrombophlebitis, decreased resistance to infection, negative nitrogen balance with delayed bone and wound healing, headache, weakness, menstrual disorders, accentuated menopausal symptoms, neuropathy, fractures, osteoporosis, peptic ulcer, decreased glucose tolerance, hypokalemia, and adrenal insufficiency. Hepatomegaly and abdominal distention have been observed in children. Treatment of acute overdosage is by immediate gastric lavage or emesis followed by supportive and symptomatic therapy. For chronic overdosage in the face of severe disease requiring continuous steroid therapy the dosage of prednisone may be reduced only temporarily, or alternate day treatment may be introduced.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS Common adverse reactions for corticosteroids include fluid retention, alteration in glucose tolerance, elevation in blood pressure, behavioral and mood changes, increased appetite and weight gain. Allergic Reactions: Anaphylaxis, angioedema Cardiovascular: Bradycardia, cardiac arrest, cardiac arrhythmias, cardiac enlargement, circulatory collapse, congestive heart failure, fat embolism, hypertension, hypertrophic cardiomyopathy in premature infants, myocardial rupture following recent myocardial infarction, pulmonary edema, syncope, tachycardia, thromboembolism, thrombophlebitis, vasculitis Dermatologic: Acne, allergic dermatitis, cutaneous and subcutaneous atrophy, dry scalp, edema, facial erythema, hyper or hypopigmentation, impaired wound healing, increased sweating, petechiae and ecchymoses, rash, sterile abscess, striae, suppressed reactions to skin tests, thin fragile skin, thinning scalp hair, urticaria Endocrine: Abnormal fat deposits, decreased carbohydrate tolerance, development of Cushingoid state, hirsutism, manifestations of latent diabetes mellitus and increased requirements for insulin or oral hypoglycemic agents in diabetics, menstrual irregularities, moon facies, secondary adrenocortical and pituitary unresponsiveness (particularly in times of stress, as in trauma, surgery or illness), suppression of growth in children Fluid and Electrolyte Disturbances: Fluid retention, potassium loss, hypertension, hypokalemic alkalosis, sodium retention Gastrointestinal: Abdominal distention, elevation in serum liver enzymes levels (usually reversible upon discontinuation), hepatomegaly, hiccups, malaise, nausea, pancreatitis, peptic ulcer with possible perforation and hemorrhage, ulcerative esophagitis General: Increased appetite and weight gain Metabolic: Negative nitrogen balance due to protein catabolism Musculoskeletal: Osteonecrosis of femoral and humeral heads, charcot-like arthropathy, loss of muscle mass, muscle weakness, osteoporosis, pathologic fracture of long bones, steroid myopathy, tendon rupture, vertebral compression fractures Neurological: Arachnoiditis, convulsions, depression, emotional instability, euphoria, headache, increased intracranial pressure with papilledema (pseudo-tumor cerebri) usually following discontinuation of treatment, insomnia, meningitis, mood swings, neuritis, neuropathy, paraparesis/paraplegia, paresthesia, personality changes, sensory disturbances, vertigo Ophthalmic: Exophthalmos, glaucoma, increased intraocular pressure, posterior subcapsular cataracts, and central serous chorioretinopathy Reproductive: Alteration in motility and number of spermatozoa Common adverse reactions for corticosteroids include fluid retention, alteration in glucose tolerance, elevation in blood pressure, behavioral and mood changes, increased appetite and weight gain. ( 6 ) To report SUSPECTED ADVERSE REACTIONS, contact Horizon at 1-866-479-6742 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch . 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The safety of RAYOS was evaluated in 375 rheumatoid arthritis patients in two controlled trials. Patients treated with RAYOS ranged in age from 20 to 80 years (median age 56 years), with 85% female, 99% Caucasian, 1% African-American, and < 1% Asian. Patients received RAYOS 3 mg to 10 mg once daily at 10 pm; the majority (84%) received ≤ 5 mg. The clinical trial experience did not raise new safety concerns beyond those already established for immediate-release prednisone. 6.2 Postmarketing Experience Adverse reactions have been identified during post approval use of RAYOS. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The postmarketing experience has not raised new safety concerns beyond those already established for immediate-release prednisone.
RAYOS Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS Anticoagulant agents: May enhance or diminish anticoagulant effects. ( 7.4 ) Antidiabetic agents: May increase blood glucose concentrations. Dose adjustments of antidiabetic agents may be required. ( 7.5 ) CYP 3A4 inducers and inhibitors: May, respectively, increase or decrease clearance of corticosteroids, necessitating dose adjustment. ( 7.7 , 7.8 ) Cyclosporine: Increase in activity of both, cyclosporine and corticosteroid when administered concurrently. Convulsions have been reported with concurrent use. ( 7.10 ) NSAIDs including aspirin and salicylates: Increased risk of gastrointestinal side effects. ( 7.13 ) 7.1 Aminoglutethimide Aminoglutethimide may lead to loss of corticosteroid-induced adrenal suppression. 7.2 Amphotericin B Injection There have been cases reported in which concomitant use of Amphotericin B and hydrocortisone was followed by cardiac enlargement and congestive heart failure [see Drug Interactions (7.14) ] . 7.3 Anticholinesterase Agents Concomitant use of anticholinesterase agents and corticosteroids may produce severe weakness in patients with myasthenia gravis. If possible, anticholinesterase agents should be withdrawn at least 24 hours before initiating corticosteroid therapy. 7.4 Anticoagulant Agents Co-administration of corticosteroids and warfarin usually results in inhibition of response to warfarin, although there have been some conflicting reports. Therefore, coagulation indices should be monitored frequently to maintain the desired anticoagulant effect. 7.5 Antidiabetic Agents Because corticosteroids may increase blood glucose concentrations, dosage adjustments of antidiabetic agents may be required. 7.6 Antitubercular Drugs Serum concentrations of isoniazid may be decreased. 7.7 CYP 3A4 Inducers (e.g., Barbiturates, Phenytoin, Carbamazepine, and Rifampin) Drugs such as barbiturates, phenytoin, ephedrine, and rifampin, which induce hepatic microsomal drug metabolizing enzyme activity may enhance the metabolism of corticosteroids and require that the dosage of the corticosteroid be increased. 7.8 CYP 3A4 Inhibitors (e.g., Ketoconazole, Macrolide Antibiotics) Ketoconazole has been reported to decrease the metabolism of certain corticosteroids by up to 60% leading to increased risk of corticosteroid side effects. 7.9 Cholestyramine Cholestyramine may increase the clearance of corticosteroids. 7.10 Cyclosporine Increased activity of both cyclosporine and corticosteroids may occur when the two are used concurrently. Convulsions have been reported with this concurrent use. 7.11 Digitalis Patients on digitalis glycosides may be at increased risk of arrhythmias due to hypokalemia. 7.12 Estrogens, Including Oral Contraceptives Estrogens may decrease the hepatic metabolism of certain corticosteroids, thereby increasing their effect. 7.13 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) Including Aspirin and Salicylates Concomitant use of aspirin or other nonsteroidal anti-inflammatory drugs and corticosteroids increases the risk of gastrointestinal side effects. Aspirin should be used cautiously in conjunction with corticosteroids in hypoprothrombinemia. The clearance of salicylates may be increased with concurrent use of corticosteroids; this could lead to decreased salicylate serum levels or increase the risk of salicylate toxicity when corticosteroid is withdrawn. 7.14 Potassium-Depleting Agents (e.g., Diuretics, Amphotericin B) When corticosteroids are administered concomitantly with potassium-depleting agents, patients should be observed closely for development of hypokalemia. 7.15 Skin Tests Corticosteroids may suppress reactions to skin tests. 7.16 Toxoids and Live or Attenuated Vaccines Patients on corticosteroid therapy may exhibit a diminished response to toxoids and live or inactivated vaccines due to inhibition of antibody response. Corticosteroids may also potentiate the replication of some organisms contained in live attenuated vaccines. Routine administration of vaccines or toxoids should be deferred until corticosteroid therapy is discontinued if possible [see Warnings and Precautions (5.8) ] .
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Naturally occurring corticosteroids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs, such as prednisone, are primarily used for their potent anti-inflammatory effects in disorders of many organ systems. Corticosteroids, such as prednisone, cause profound and varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli. Prednisone is a synthetic adrenocortical steroid drug with predominantly corticosteroid properties. Some of these properties reproduce the physiological actions of endogenous glucocorticosteroids, but others do not necessarily reflect any of the adrenal hormones' normal functions; they are seen only after administration of large therapeutic doses of the drug. The pharmacological effects of prednisone which are due to its corticosteroid properties include: promotion of gluconeogenesis; increased deposition of glycogen in the liver; inhibition of the utilization of glucose; anti-insulin activity; increased catabolism of protein; increased lipolysis; stimulation of fat synthesis and storage; increased glomerular filtration rate and resulting increase in urinary excretion of urate (creatinine excretion remains unchanged); and increased calcium excretion. Depressed production of eosinophils and lymphocytes occurs, but erythropoiesis and production of polymorphonuclear leukocytes are stimulated. Inflammatory processes (edema, fibrin deposition, capillary dilatation, migration of leukocytes and phagocytosis) and the later stages of wound healing (capillary proliferation, deposition of collagen, cicatrization) are inhibited. Prednisone can stimulate secretion of various components of gastric juice. Suppression of the production of corticotropin may lead to suppression of endogenous corticosteroids. Prednisone has slight mineralocorticoid activity, whereby entry of sodium into cells and loss of intracellular potassium is stimulated. This is particularly evident in the kidney, where rapid ion exchange leads to sodium retention and hypertension. 12.3 Pharmacokinetics The pharmacokinetic profile of RAYOS has an approximately 4-hour lag time from that of immediate-release prednisone formulations. While the pharmacokinetic profile of RAYOS when given with food differs in terms of lag time from IR prednisone, its absorption, distribution, and elimination processes are comparable. Absorption Prednisone is released from RAYOS when taken with food approximately 4 hours after oral ingestion. This causes a delay in the time until peak plasma concentrations (T max ) are achieved. Median T max of RAYOS in 27 healthy male subjects was 6.0 - 6.5 hours compared to 2.0 hours for an immediate-release (IR) formulation. Subsequently, prednisone was absorbed at the same rate as the IR formulation. Peak plasma concentrations (C max ) and exposure, as indicated by AUC 0-last and AUC 0--∞ , were comparable for both prednisone IR and RAYOS administered 2.5 hours after a light meal or with normal meal (Figure 1). Figure 1. Mean Plasma Levels of Prednisone After a Single Dose of 5 mg Prednisone Administered as a 5 mg RAYOS Tablet or a 5 mg Immediate-Release (IR) Tablet A: 5 mg IR tablet under fasting conditions, administered at 2 am, B: 5 mg RAYOS, administered 2.5 hours after a light evening meal, and C: 5 mg RAYOS administered immediately after dinner. In a study with 24 healthy subjects, oral absorption of prednisone from RAYOS was significantly affected by the intake of food. Under standard fasting conditions, both the maximum plasma concentration (C max ) and the bioavailability of RAYOS were significantly lower than under fed conditions, shortly after intake of a high fat meal. RAYOS at dose levels of 1 mg, 2 mg, and 5 mg showed dose-proportionality in terms of peak and systemic exposure (C max , AUC 0-∞ , and AUC 0-last ) for the parent drug prednisone as well as for the active metabolite prednisolone. Figure 1 Metabolism Prednisone is completely converted to the active metabolite prednisolone, which is further metabolized mainly in the liver and excreted in the urine as sulfate and glucuronide conjugates. The exposure of prednisolone is 4-6 fold higher than that of prednisone. Excretion The terminal half-life of both prednisone and prednisolone from the administration of RAYOS was 2-3 hours, which is comparable to that from the IR formulation. Special Populations The effects of gender, age, renal impairment, and hepatic impairment on the pharmacokinetics of prednisone or prednisolone after administration of RAYOS have not been evaluated.
| A: 5 mg IR tablet under fasting conditions, administered at 2 am, B: 5 mg RAYOS, administered 2.5 hours after a light evening meal, and C: 5 mg RAYOS administered immediately after dinner. |
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action Naturally occurring corticosteroids (hydrocortisone and cortisone), which also have salt-retaining properties, are used as replacement therapy in adrenocortical deficiency states. Their synthetic analogs, such as prednisone, are primarily used for their potent anti-inflammatory effects in disorders of many organ systems. Corticosteroids, such as prednisone, cause profound and varied metabolic effects. In addition, they modify the body's immune responses to diverse stimuli. Prednisone is a synthetic adrenocortical steroid drug with predominantly corticosteroid properties. Some of these properties reproduce the physiological actions of endogenous glucocorticosteroids, but others do not necessarily reflect any of the adrenal hormones' normal functions; they are seen only after administration of large therapeutic doses of the drug. The pharmacological effects of prednisone which are due to its corticosteroid properties include: promotion of gluconeogenesis; increased deposition of glycogen in the liver; inhibition of the utilization of glucose; anti-insulin activity; increased catabolism of protein; increased lipolysis; stimulation of fat synthesis and storage; increased glomerular filtration rate and resulting increase in urinary excretion of urate (creatinine excretion remains unchanged); and increased calcium excretion. Depressed production of eosinophils and lymphocytes occurs, but erythropoiesis and production of polymorphonuclear leukocytes are stimulated. Inflammatory processes (edema, fibrin deposition, capillary dilatation, migration of leukocytes and phagocytosis) and the later stages of wound healing (capillary proliferation, deposition of collagen, cicatrization) are inhibited. Prednisone can stimulate secretion of various components of gastric juice. Suppression of the production of corticotropin may lead to suppression of endogenous corticosteroids. Prednisone has slight mineralocorticoid activity, whereby entry of sodium into cells and loss of intracellular potassium is stimulated. This is particularly evident in the kidney, where rapid ion exchange leads to sodium retention and hypertension.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics The pharmacokinetic profile of RAYOS has an approximately 4-hour lag time from that of immediate-release prednisone formulations. While the pharmacokinetic profile of RAYOS when given with food differs in terms of lag time from IR prednisone, its absorption, distribution, and elimination processes are comparable. Absorption Prednisone is released from RAYOS when taken with food approximately 4 hours after oral ingestion. This causes a delay in the time until peak plasma concentrations (T max ) are achieved. Median T max of RAYOS in 27 healthy male subjects was 6.0 - 6.5 hours compared to 2.0 hours for an immediate-release (IR) formulation. Subsequently, prednisone was absorbed at the same rate as the IR formulation. Peak plasma concentrations (C max ) and exposure, as indicated by AUC 0-last and AUC 0--∞ , were comparable for both prednisone IR and RAYOS administered 2.5 hours after a light meal or with normal meal (Figure 1). Figure 1. Mean Plasma Levels of Prednisone After a Single Dose of 5 mg Prednisone Administered as a 5 mg RAYOS Tablet or a 5 mg Immediate-Release (IR) Tablet A: 5 mg IR tablet under fasting conditions, administered at 2 am, B: 5 mg RAYOS, administered 2.5 hours after a light evening meal, and C: 5 mg RAYOS administered immediately after dinner. In a study with 24 healthy subjects, oral absorption of prednisone from RAYOS was significantly affected by the intake of food. Under standard fasting conditions, both the maximum plasma concentration (C max ) and the bioavailability of RAYOS were significantly lower than under fed conditions, shortly after intake of a high fat meal. RAYOS at dose levels of 1 mg, 2 mg, and 5 mg showed dose-proportionality in terms of peak and systemic exposure (C max , AUC 0-∞ , and AUC 0-last ) for the parent drug prednisone as well as for the active metabolite prednisolone. Figure 1 Metabolism Prednisone is completely converted to the active metabolite prednisolone, which is further metabolized mainly in the liver and excreted in the urine as sulfate and glucuronide conjugates. The exposure of prednisolone is 4-6 fold higher than that of prednisone. Excretion The terminal half-life of both prednisone and prednisolone from the administration of RAYOS was 2-3 hours, which is comparable to that from the IR formulation. Special Populations The effects of gender, age, renal impairment, and hepatic impairment on the pharmacokinetics of prednisone or prednisolone after administration of RAYOS have not been evaluated.
| A: 5 mg IR tablet under fasting conditions, administered at 2 am, B: 5 mg RAYOS, administered 2.5 hours after a light evening meal, and C: 5 mg RAYOS administered immediately after dinner. |
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS RAYOS is contraindicated in patients who have known hypersensitivity to prednisone or to any of the excipients. Rare instances of anaphylaxis have occurred in patients receiving corticosteroid therapy [see Adverse Reactions (6) ] . Known hypersensitivity to prednisone or any excipients in the formulation ( 4 , 6 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION The active ingredient in RAYOS is prednisone (a corticosteroid). Corticosteroids are adrenocortical steroids, both naturally occurring and synthetic. The molecular formula for prednisone is C 21 H 26 O 5 . The chemical name for prednisone is 17,21-dihydroxypregna-1,4-diene-3,11,20-trione, and the structural formula is: Prednisone is a white to practically white, odorless, crystalline powder and has a molecular weight of 358.43. Prednisone is very slightly soluble in water; slightly soluble in alcohol, chloroform, dioxane, and methanol. RAYOS is a delayed-release prednisone tablet. It consists of a prednisone-containing core tablet in an inactive shell, which delays the onset of in vitro drug dissolution by approximately 4 hours. Each tablet contains 1 mg, 2 mg, or 5 mg of prednisone, with the following inactive ingredients: dibasic calcium phosphate dihydrate, colloidal silicon dioxide, croscarmellose sodium, glycerol dibehenate, lactose monohydrate, magnesium stearate, povidone, yellow ferric oxide, and red ferric oxide. Chemical Structure
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION Individualize dosing based on disease severity and patient response. The timing of administration should take into account the delayed-release pharmacokinetics and the disease or condition being treated ( 2 , 12.1 ): Initial dose: RAYOS 5 mg administered once per day. Patients currently on immediate-release prednisone, prednisolone, or methylprednisolone should be switched to RAYOS at an equivalent dose based on relative potency. ( 2.1 , 2.4 ) Maintenance dose: Use lowest dosage that will maintain an adequate clinical response. ( 2.1 ) Discontinuation: Withdraw gradually if discontinuing long-term or high-dose therapy. ( 2.1 ) RAYOS should be taken daily with food. ( 2.3 , 12.3 ) RAYOS should be swallowed whole and not broken, divided, or chewed. ( 2.3 ) 2.1 Recommended Dosing Dosage of RAYOS should be individualized according to the severity of the disease and the response of the patient. For pediatric patients, the recommended dosage should be governed by the same considerations rather than strict adherence to the ratio indicated by age or body weight. The maximal activity of the adrenal cortex is between 2 am and 8 am and is minimal between 4 pm and midnight. Exogenous corticosteroids suppress adrenocorticoid activity the least when given at the time of maximal activity. RAYOS is a delayed-release formulation of prednisone which releases the active substance beginning approximately 4 hours after intake [see Clinical Pharmacology (12.3) ] . The timing of RAYOS administration should take into account the delayed-release pharmacokinetics and the disease or condition being treated. The initial dosage of RAYOS may vary from 5 to 60 mg per day depending on the specific disease entity being treated. Patients currently on immediate release prednisone, prednisolone, or methylprednisolone should be switched to RAYOS at an equivalent dose based on relative potency (2.4). In situations of less severity, lower doses will generally suffice while in selected patients higher initial doses may be required. The initial dosage should be maintained or adjusted until a satisfactory response is noted. If after a reasonable period there is a lack of satisfactory clinical response, RAYOS should be discontinued and the patient transferred to other appropriate therapy. It should be emphasized that dosage requirements are variable and must be individualized on the basis of the disease under treatment and the response of the patient. After a favorable response is noted, the proper maintenance dosage should be determined by decreasing the initial drug dosage in small decrements at appropriate time intervals until the lowest dosage which will maintain an adequate clinical response is reached. It should be kept in mind that constant monitoring is needed in regard to drug dosage. Included in the situations which may make dosage adjustments necessary are changes in clinical status secondary to remissions or exacerbations in the disease process, the patient's individual drug responsiveness, and the effect of patient exposure to stressful situations not directly related to the disease entity under treatment. In this latter situation it may be necessary to increase the dosage of RAYOS for a period of time consistent with the patient's condition. If a period of spontaneous remission occurs in a chronic condition, treatment should be discontinued. If after long-term therapy the drug is to be stopped, it is recommended that it be withdrawn gradually rather than abruptly. 2.2 Recommended Monitoring Blood pressure, body weight, routine laboratory studies (including 2-hour postprandial blood glucose and serum potassium), and chest X-ray should be obtained at regular intervals during prolonged therapy with RAYOS. Upper GI X-rays are desirable in patients with known or suspected peptic ulcer disease. 2.3 Method of Administration RAYOS is for oral administration. RAYOS should be taken daily with food [see Clinical Pharmacology (12.3) ] . RAYOS tablets should not be broken, divided, or chewed because the delayed release of prednisone is dependent on an intact coating [see Description (11) ]. 2.4 Corticosteroid Comparison Chart For the purpose of comparison, one 5 mg RAYOS tablet is the equivalent milligram dosage of the following various corticosteroids: Betamethasone, 0.75 mg Paramethasone, 2 mg Cortisone, 25 mg Prednisolone, 5 mg Dexamethasone, 0.75 mg Prednisone, 5 mg Hydrocortisone, 20 mg Triamcinolone, 4 mg Methylprednisolone, 4 mg These dose relationships apply only to oral or intravenous administration of these compounds. When these substances or their derivatives are injected intramuscularly or into joint spaces, their relative properties may be greatly altered.
| Betamethasone, 0.75 mg | Paramethasone, 2 mg |
| Cortisone, 25 mg | Prednisolone, 5 mg |
| Dexamethasone, 0.75 mg | Prednisone, 5 mg |
| Hydrocortisone, 20 mg | Triamcinolone, 4 mg |
| Methylprednisolone, 4 mg |
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Delayed-release Tablets RAYOS 1 mg prednisone: Pale yellowish-white, round, unscored delayed-release tablet embossed with "NP 1" on one side. RAYOS 2 mg prednisone: Yellowish-white, round, unscored delayed-release tablet embossed with "NP 2" on one side. RAYOS 5 mg prednisone: Light yellow, round, unscored delayed-release tablet embossed with "NP 5" on one side. Delayed-release tablets: 1 mg, 2 mg, and 5 mg prednisone ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1. INDICATIONS AND USAGE RAYOS is indicated in the treatment of the following diseases or conditions: RAYOS is a corticosteroid indicated as an anti-inflammatory or immunosuppressive agent for certain allergic, dermatologic, gastrointestinal, hematologic, ophthalmologic, nervous system, renal, respiratory, rheumatologic, specific infectious diseases or conditions and organ transplantation ( 1 ) for the treatment of certain endocrine conditions ( 1 ) for palliation of certain neoplastic conditions ( 1 ) 1.1 Allergic Conditions Control of severe or incapacitating allergic conditions intractable to adequate trials of conventional treatment in adults and pediatric populations with: Atopic dermatitis Drug hypersensitivity reactions Seasonal or perennial allergic rhinitis Serum sickness 1.2 Dermatologic Diseases Bullous dermatitis herpetiformis Contact dermatitis Exfoliative erythroderma Mycosis fungoides Pemphigus Severe erythema multiforme (Stevens-Johnson syndrome) 1.3 Endocrine Conditions Congenital adrenal hyperplasia Hypercalcemia of malignancy Nonsuppurative thyroiditis Primary or secondary adrenocortical insufficiency: hydrocortisone or cortisone is the first choice: synthetic analogs may be used in conjunction with mineralocorticoids where applicable 1.4 Gastrointestinal Diseases During acute episodes in: Crohn's Disease Ulcerative colitis 1.5 Hematologic Diseases Acquired (autoimmune) hemolytic anemia Diamond-Blackfan anemia Idiopathic thrombocytopenic purpura in adults Pure red cell aplasia Secondary thrombocytopenia in adults 1.6 Neoplastic Conditions For the treatment of: Acute leukemia Aggressive lymphomas 1.7 Nervous System Conditions Acute exacerbations of multiple sclerosis Cerebral edema associated with primary or metastatic brain tumor, craniotomy or head injury 1.8 Ophthalmic Conditions Sympathetic ophthalmia Uveitis and ocular inflammatory conditions unresponsive to topical steroids 1.9 Conditions Related to Organ Transplantation Acute or chronic solid organ rejection 1.10 Pulmonary Diseases Acute exacerbations of chronic obstructive pulmonary disease (COPD) Allergic bronchopulmonary aspergillosis Aspiration pneumonitis Asthma Fulminating or disseminated pulmonary tuberculosis when used concurrently with appropriate chemotherapy Hypersensitivity pneumonitis Idiopathic bronchiolitis obliterans with organizing pneumonia Idiopathic eosinophilic pneumonias Idiopathic pulmonary fibrosis Pneumocystis carinii pneumonia (PCP) associated with hypoxemia occurring in an HIV(+) individual who is also under treatment with appropriate anti-PCP antibiotics. Symptomatic sarcoidosis 1.11 Renal Conditions To induce a diuresis or remission of proteinuria in nephrotic syndrome, without uremia, of the idiopathic type or that due to lupus erythematosus 1.12 Rheumatologic Conditions As adjunctive therapy for short-term administration (to tide the patient over an acute episode or exacerbation) in: Acute gouty arthritis During an exacerbation or as maintenance therapy in selected cases of: Ankylosing spondylitis Dermatomyositis/polymyositis Polymyalgia rheumatica Psoriatic arthritis Relapsing polychondritis Rheumatoid arthritis, including juvenile rheumatoid arthritis (selected cases may require low dose maintenance therapy) Sjogren's syndrome Systemic lupus erythematosus Vasculitis 1.13 Specific Infectious Diseases Trichinosis with neurologic or myocardial involvement. Tuberculous meningitis with subarachnoid block or impending block used concurrently with appropriate antituberculous chemotherapy.
Spl product data elements
Usually a list of ingredients in a drug product.RAYOS prednisone PREDNISONE PREDNISONE LACTOSE MONOHYDRATE POVIDONE, UNSPECIFIED CROSCARMELLOSE SODIUM SILICON DIOXIDE MAGNESIUM STEARATE FERRIC OXIDE RED FERRIC OXIDE YELLOW DIBASIC CALCIUM PHOSPHATE DIHYDRATE GLYCERYL DIBEHENATE WATER Pale Yellowish White NP;1 RAYOS prednisone PREDNISONE PREDNISONE LACTOSE MONOHYDRATE POVIDONE, UNSPECIFIED CROSCARMELLOSE SODIUM SILICON DIOXIDE MAGNESIUM STEARATE FERRIC OXIDE RED FERRIC OXIDE YELLOW DIBASIC CALCIUM PHOSPHATE DIHYDRATE GLYCERYL DIBEHENATE WATER Yellowish White NP;2 RAYOS prednisone PREDNISONE PREDNISONE LACTOSE MONOHYDRATE POVIDONE, UNSPECIFIED CROSCARMELLOSE SODIUM SILICON DIOXIDE MAGNESIUM STEARATE FERRIC OXIDE RED FERRIC OXIDE YELLOW DIBASIC CALCIUM PHOSPHATE DIHYDRATE GLYCERYL DIBEHENATE WATER Light Yellow NP;5
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Prednisone was not formally evaluated in carcinogenicity studies. Review of the published literature identified carcinogenicity studies of prednisolone, the active metabolite of prednisone, at doses which were less than the typical clinical doses. In a 2-year study, male Sprague-Dawley rats administered prednisolone in drinking water at a dose of 368 mcg/kg/day (equivalent to 3.5 mg/day in a 60 kg individual based on a mg/m 2 body surface area comparison) developed increased incidences of hepatic adenomas. Lower doses were not studied, and therefore, a no effect level could not be identified. In an 18-month study, intermittent oral gavage administration of prednisolone did not induce tumors in female Sprague-Dawley rats when given 1, 2, 4.5, or 9 times per month at 3 mg/kg prednisone (equivalent to 29 mg in a 60-kg individual based on a mg/m 2 body surface area comparison). Prednisone was not formally evaluated for genotoxicity. However, in published studies prednisolone was not mutagenic with or without metabolic activation in the Ames bacterial reverse mutation assay using Salmonella typhimurium and Escherichia coli , or in a mammalian cell gene mutation assay using mouse lymphoma L5178Y cells, according to current evaluation standards. In a published chromosomal aberration study in Chinese Hamster Lung (CHL) cells, a slight increase was seen in the incidence of structural chromosomal aberrations with metabolic activation at the highest concentration tested, however, the effect appears to be equivocal. Prednisolone was not genotoxic in an in vivo micronucleus assay in the mouse, though the study design did not meet current criteria. Prednisone was not formally evaluated in fertility studies. Corticosteroids have been shown to impair fertility in male rats. Menstrual irregularities have been described with clinical use [see Adverse Reactions (6) ] .
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Prednisone was not formally evaluated in carcinogenicity studies. Review of the published literature identified carcinogenicity studies of prednisolone, the active metabolite of prednisone, at doses which were less than the typical clinical doses. In a 2-year study, male Sprague-Dawley rats administered prednisolone in drinking water at a dose of 368 mcg/kg/day (equivalent to 3.5 mg/day in a 60 kg individual based on a mg/m 2 body surface area comparison) developed increased incidences of hepatic adenomas. Lower doses were not studied, and therefore, a no effect level could not be identified. In an 18-month study, intermittent oral gavage administration of prednisolone did not induce tumors in female Sprague-Dawley rats when given 1, 2, 4.5, or 9 times per month at 3 mg/kg prednisone (equivalent to 29 mg in a 60-kg individual based on a mg/m 2 body surface area comparison). Prednisone was not formally evaluated for genotoxicity. However, in published studies prednisolone was not mutagenic with or without metabolic activation in the Ames bacterial reverse mutation assay using Salmonella typhimurium and Escherichia coli , or in a mammalian cell gene mutation assay using mouse lymphoma L5178Y cells, according to current evaluation standards. In a published chromosomal aberration study in Chinese Hamster Lung (CHL) cells, a slight increase was seen in the incidence of structural chromosomal aberrations with metabolic activation at the highest concentration tested, however, the effect appears to be equivocal. Prednisolone was not genotoxic in an in vivo micronucleus assay in the mouse, though the study design did not meet current criteria. Prednisone was not formally evaluated in fertility studies. Corticosteroids have been shown to impair fertility in male rats. Menstrual irregularities have been described with clinical use [see Adverse Reactions (6) ] .
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PRINCIPAL DISPLAY PANEL - 1 mg Tablet Bottle Carton NDC 75987-020-01 RAYOS ® (Prednisone) Delayed-release Tablets 1 mg 30 Tablets Swallow whole. Do not crush, divide, or chew tablets. Rx Only PRINCIPAL DISPLAY PANEL - 1 mg Tablet Bottle Carton
PRINCIPAL DISPLAY PANEL - 2 mg Tablet Bottle Carton NDC 75987-021-01 RAYOS ® (Prednisone) Delayed-release Tablets 2 mg 30 Tablets Swallow whole. Do not crush, divide, or chew tablets. Rx Only PRINCIPAL DISPLAY PANEL - 2 mg Tablet Bottle Carton
PRINCIPAL DISPLAY PANEL - 5 mg Tablet Bottle Carton NDC 75987-022-01 RAYOS ® (Prednisone) Delayed-release Tablets 5 mg 30 Tablets Swallow whole. Do not crush, divide, or chew tablets. Rx Only PRINCIPAL DISPLAY PANEL - 5 mg Tablet Bottle Carton
Recent major changes
A list of the section(s) that contain substantive changes that have been approved by FDA in the product labeling. The headings and subheadings, if appropriate, affected by the change are listed together with each section’s identifying number and the month and year on which the change was incorporated in the labeling.Warnings and Precautions, Immunosuppression and Increased Risk of Infection ( 5.2 ) 03/2024
| Warnings and Precautions, Immunosuppression and Increased Risk of Infection ( | 03/2024 |
Spl unclassified section
Information not classified as belonging to one of the other fields. Approximately 40% of labeling with effective_time between June 2009 and August 2014 have information in this field.Distributed by: Horizon Therapeutics USA, Inc. Deerfield, IL 60015 RAY-US-PI-002
RAYOS: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Patients should be informed of the following information before initiating therapy with RAYOS and periodically during the course of ongoing therapy. Patients should be warned not to discontinue the use of RAYOS abruptly or without medical supervision, to advise any medical attendants that they are taking it, and to seek medical advice at once should they develop fever or other signs of infection. Patients should be told to take RAYOS exactly as prescribed, follow the instructions on the prescription label, and not stop taking RAYOS without first checking with their healthcare providers, as there may be a need for gradual dose reduction. Patients should discuss with their physician if they have had recent or ongoing infections or if they have recently received a vaccine. Persons who are on immunosuppressant doses of corticosteroids should be warned to avoid exposure to chickenpox or measles. Patients should also be advised that if they are exposed, medical advice should be sought without delay. There are a number of medicines that can interact with RAYOS. Patients should inform their healthcare provider of all the medicines they are taking, including over-the-counter and prescription medicines (such as phenytoin, diuretics, digitalis or digoxin, rifampin, amphotericin B, cyclosporine, insulin or diabetes medicines, ketoconazole, estrogens including birth control pills and hormone replacement therapy, blood thinners such as warfarin, aspirin or other NSAIDs, barbiturates), dietary supplements, and herbal products. If patients are taking any of these drugs, alternate therapy, dosage adjustment, and/or special test may be needed during the treatment. For missed doses, patients should be told to take the missed dose as soon as they remember. If it is almost time for the next dose, the missed dose should be skipped and the medicine taken at the next regularly schedule time. Patients should not take an extra dose to make up for the missed dose. Patients should be told to take RAYOS with food. Patients should be advised not to break, divide, or chew RAYOS. Patients should be advised of common adverse reactions that could occur with RAYOS use to include fluid retention, alteration in glucose tolerance, elevation in blood pressure, behavioral and mood changes, increased appetite and weight gain. Advise pregnant women and females of reproductive potential of the potential risk to a fetus. Advise females to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.10) and Use in Specific Populations (8.1) ] .
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES The efficacy of RAYOS in the treatment of rheumatoid arthritis was assessed in one multicenter, double-blind, placebo-controlled, randomized, 12-week trial in patients ≥ 18 years with active rheumatoid arthritis diagnosed according to American College of Rheumatology (ACR) criteria. Patients were enrolled who were not currently treated with corticosteroids but had received non-biologic DMARD therapy for at least 6 months before receipt of study medication, and had an incomplete response to DMARD therapy alone. Patients were randomized in a 2:1 ratio to treatment with RAYOS 5 mg (n = 231) or placebo (n = 119) administered at 10 pm. A total of 350 patients were enrolled and ranged in age from 27 to 80 years (median age 57 years) with 84% females. Race was distributed as follows: 98% Caucasian, 1% African-American, and < 1% Asian. The percentage of patients with improvement in rheumatoid arthritis at 12 weeks using ACR response criteria (ACR20) was assessed as the primary endpoint, and ACR20, ACR50 and ACR70 responses for patients treated with RAYOS 5 mg versus placebo are shown in Table 1. The relative efficacy of RAYOS compared to immediate-release prednisone has not been established. Table 1. ACR Responses (Percentage of Patients) ACR Response at 12 Weeks RAYOS 5 mg Placebo RAYOS 5 mg - Placebo (95% CI) N = 231 N = 119 All missing values were imputed as non-responders. ACR20 47% 29% 17% (7.2, 27.6) ACR50 22% 10% 12% (4.4, 19.6) ACR70 7% 3% 4% (0.1, 8.7) The results of the components of the ACR response criteria are shown in Table 2. Table 2. Components of ACR Response Parameter RAYOS 5 mg + DMARD N = 231 Placebo + DMARD N = 119 Baseline Week 12 Baseline Week 12 Mean (SD) is presented. Baseline values were carried forward for patients with missing data at Week 12. Tender joint count 28-joint count 12.6 (6.2) 7.9 (6.8) 12.5 (5.9) 9.8 (6.7) Swollen joint count 8.4 (4.4) 4.8 (4.8) 8.6 (4.7) 6.1 (5.4) Patient assessment of pain Patient assessment of arthritis pain. Visual analog scale: 0 = no pain, 100 = very intensive pain 55.3 (21.9) 33.0 (24.5) 50.5 (23.3) 39.6 (24.7) Patient global assessment Patient or physician global assessment of disease activity. Visual analog scale: 0 = not active at all, 100 = extremely active 57.4 (20.1) 36.2 (24.5) 50.9 (20.9) 43.0 (22.4) Physician global assessment 55.2 (16.1) 31.9 (19.7) 54.1 (17.4) 40.4 (21.8) Disability index (HAQ-DI) Health Assessment Questionnaire Disability Index; 0 = best, 3 = worst, measures the patient's ability to perform the following: dress/groom, arise, eat, walk, reach, grip, maintain hygiene, and maintain daily activity. 1.3 (0.6) 1.1 (0.6) 1.3 (0.6) 1.2 (0.6) ESR (mm/hr) 33.0 (16.6) 25.2 (16.8) 32.9 (20.0) 26.5 (19.7) CRP (mg/dL) 9.3 (13.2) 7.5 (10.7) 11.8 (18.0) 9.7 (12.1) The percentage of patients achieving ACR20 responses by visit is shown in Figure 2. Figure 2. ACR20 Response Over 12 Weeks The same patients may not have responded at each time point. The percent change from baseline in the duration of morning stiffness at 12 weeks was assessed as a prespecified secondary endpoint. Patients treated with RAYOS had a median decrease in the duration of morning stiffness of 55% compared to 33% in placebo-treated patients (20% estimated median difference between treatment groups with 95% confidence interval [7, 32]). This corresponds to a median duration of morning stiffness of 46 minutes in the RAYOS group and 85 minutes in the placebo group. Figure 2
| ACR Response at 12 Weeks | RAYOS 5 mg | Placebo | RAYOS 5 mg - Placebo (95% CI) |
|---|---|---|---|
| N = 231 | N = 119 | ||
| All missing values were imputed as non-responders. | |||
| ACR20 | 47% | 29% | 17% (7.2, 27.6) |
| ACR50 | 22% | 10% | 12% (4.4, 19.6) |
| ACR70 | 7% | 3% | 4% (0.1, 8.7) |
| Parameter | RAYOS 5 mg + DMARD N = 231 | Placebo + DMARD N = 119 | ||
|---|---|---|---|---|
| Baseline | Week 12 | Baseline | Week 12 | |
| Mean (SD) is presented. Baseline values were carried forward for patients with missing data at Week 12. | ||||
| Tender joint count | 12.6 (6.2) | 7.9 (6.8) | 12.5 (5.9) | 9.8 (6.7) |
| Swollen joint count | 8.4 (4.4) | 4.8 (4.8) | 8.6 (4.7) | 6.1 (5.4) |
| Patient assessment of pain | 55.3 (21.9) | 33.0 (24.5) | 50.5 (23.3) | 39.6 (24.7) |
| Patient global assessment | 57.4 (20.1) | 36.2 (24.5) | 50.9 (20.9) | 43.0 (22.4) |
| Physician global assessment | 55.2 (16.1) | 31.9 (19.7) | 54.1 (17.4) | 40.4 (21.8) |
| Disability index (HAQ-DI) | 1.3 (0.6) | 1.1 (0.6) | 1.3 (0.6) | 1.2 (0.6) |
| ESR (mm/hr) | 33.0 (16.6) | 25.2 (16.8) | 32.9 (20.0) | 26.5 (19.7) |
| CRP (mg/dL) | 9.3 (13.2) | 7.5 (10.7) | 11.8 (18.0) | 9.7 (12.1) |
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use No overall differences in safety or effectiveness were observed between elderly subjects and younger subjects, and other reported clinical experience with prednisone has not identified differences in responses between the elderly and younger patients. However, the incidence of corticosteroid-induced side effects may be increased in geriatric patients and are dose-related. Osteoporosis is the most frequently encountered complication, which occurs at a higher incidence rate in corticosteroid-treated geriatric patients as compared to younger populations and in age-matched controls. Losses of bone mineral density appear to be greatest early on in the course of treatment and may recover over time after steroid withdrawal or use of lower doses (i.e., ≤ 5 mg/day). Prednisone doses of 7.5 mg/day or higher have been associated with an increased relative risk of both vertebral and nonvertebral fractures, even in the presence of higher bone density compared to patients with involution osteoporosis. Routine screening of geriatric patients, including regular assessments of bone mineral density and institution of fracture prevention strategies, along with regular review of prednisone indication should be undertaken to minimize complications and keep the prednisolone dose at the lowest acceptable level. Co-administration of certain bisphosphonates have been shown to retard the rate of bone loss in corticosteroid-treated males and postmenopausal females, and these agents are recommended in the prevention and treatment of corticosteroid-induced osteoporosis [see Warnings and Precautions (5.6) ] . It has been reported that equivalent weight-based doses yield higher total and unbound prednisolone plasma concentrations and reduced renal and non-renal clearance in elderly patients compared to younger populations. Dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use The efficacy and safety of prednisone in the pediatric population are based on the well-established course of effect of corticosteroids which is similar in pediatric and adult populations. Published studies provide evidence of efficacy and safety in pediatric patients for the treatment of nephrotic syndrome (> 2 years of age), and aggressive lymphomas and leukemias (> 1 month of age). However, some of these conclusions and other indications for pediatric use of corticosteroid, e.g., severe asthma and wheezing, are based on adequate and well-controlled trials conducted in adults, on the premises that the course of the diseases and their pathophysiology are considered to be substantially similar in both populations. The adverse effects of prednisone in pediatric patients are similar to those in adults [see Adverse Reactions (6) ] . Like adults, pediatric patients should be carefully observed with frequent measurements of blood pressure, weight, height, intraocular pressure, and clinical evaluation for the presence of infection, psychosocial disturbances, thromboembolism, peptic ulcers, cataracts, and osteoporosis. Children who are treated with corticosteroids by any route, including systemically administered corticosteroids, may experience a decrease in their growth velocity. This negative impact of corticosteroids on growth has been observed at low systemic doses and in the absence of laboratory evidence of HPA axis suppression (i.e., cosyntropin stimulation and basal cortisol levels). Growth velocity may therefore be a more sensitive indicator of systemic corticosteroid exposure in children than some commonly used tests of HPA axis function. The linear growth of children treated with corticosteroids by any route should be monitored, and the potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of other treatment alternatives. In order to minimize the potential growth effects of corticosteroids, children should be titrated to the lowest effective dose [see Warnings and Precautions (5.9) ] .
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Risk Summary Based on findings from human and animal studies, corticosteroids, including RAYOS, can cause fetal harm when administered to a pregnant woman (see Data ) [see Warnings and Precautions (5.10) ] . Published epidemiological studies suggest a small but inconsistent increased risk of orofacial clefts with use of corticosteroids during the first trimester. Intrauterine growth restriction and decreased birth weight have also been reported with maternal use of corticosteroids during pregnancy; however, the underlying maternal condition may also contribute to these risks (see Clinical Considerations ) . Published animal studies show prednisolone to be teratogenic in rats, rabbits, hamsters, and mice with increased incidence of cleft palate in offspring (see Data ) . Advise a pregnant woman about the potential harm to a fetus. The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the US general population, the estimated background risk of major birth defects and miscarriage in clinical recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Clinical Considerations Fetal/Neonatal Adverse Reactions Infants born to pregnant women who have received corticosteroids should be carefully monitored for signs and symptoms of hypoadrenalism [see Warnings and Precautions (5.1) ] . Data Human Data Published epidemiological studies on the association between prednisolone and fetal outcomes have reported inconsistent findings and have important methodological limitations. Multiple cohort and case-controlled studies in humans suggest that maternal corticosteroid use during the first trimester increases the incidence of cleft lip with or without cleft palate from about 1/1000 infants to 3-5/1000 infants; however, a risk for orofacial clefts has not been observed in all studies. Methodological limitations of these studies include non-randomized design, retrospective data collection, and the inability to control for confounders such as underlying maternal disease and use of concomitant medications. Two prospective case control studies showed decreased birth weight in infants exposed to maternal corticosteroids in utero. In humans, the risk of decreased birth weight appears to be dose related and may be minimized by administering lower corticosteroid doses. It is likely that underlying maternal conditions contribute to intrauterine growth restriction and decreased birth weight, but it is unclear to what extent these maternal conditions contribute to the increased risk of orofacial clefts. Animal Data Prednisolone, the active metabolite of prednisone, administered during the period of organogenesis, has been shown to be teratogenic in rats, rabbits, hamsters, and mice with increased incidence of cleft palate in offspring. In teratogenicity studies, cleft palate along with elevation of fetal lethality (or increase in resorptions) and reductions in fetal body weight were seen in rats at maternal doses of 30 mg/kg (equivalent to 290 mg in a 60 kg individual based on mg/m 2 body surface comparison) and higher. Cleft palate was observed in mice at a maternal dose of 20 mg/kg (equivalent to 100 mg in a 60 kg individual based on mg/m 2 comparison). Additionally, constriction of the ductus arteriosus has been observed in fetuses of pregnant rats exposed to prednisolone. RAYOS was not formally evaluated in animal reproduction studies.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Risk Summary Based on findings from human and animal studies, corticosteroids, including RAYOS, can cause fetal harm when administered to a pregnant woman (see Data ) [see Warnings and Precautions (5.10) ] . Published epidemiological studies suggest a small but inconsistent increased risk of orofacial clefts with use of corticosteroids during the first trimester. Intrauterine growth restriction and decreased birth weight have also been reported with maternal use of corticosteroids during pregnancy; however, the underlying maternal condition may also contribute to these risks (see Clinical Considerations ) . Published animal studies show prednisolone to be teratogenic in rats, rabbits, hamsters, and mice with increased incidence of cleft palate in offspring (see Data ) . Advise a pregnant woman about the potential harm to a fetus. The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the US general population, the estimated background risk of major birth defects and miscarriage in clinical recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Clinical Considerations Fetal/Neonatal Adverse Reactions Infants born to pregnant women who have received corticosteroids should be carefully monitored for signs and symptoms of hypoadrenalism [see Warnings and Precautions (5.1) ] . Data Human Data Published epidemiological studies on the association between prednisolone and fetal outcomes have reported inconsistent findings and have important methodological limitations. Multiple cohort and case-controlled studies in humans suggest that maternal corticosteroid use during the first trimester increases the incidence of cleft lip with or without cleft palate from about 1/1000 infants to 3-5/1000 infants; however, a risk for orofacial clefts has not been observed in all studies. Methodological limitations of these studies include non-randomized design, retrospective data collection, and the inability to control for confounders such as underlying maternal disease and use of concomitant medications. Two prospective case control studies showed decreased birth weight in infants exposed to maternal corticosteroids in utero. In humans, the risk of decreased birth weight appears to be dose related and may be minimized by administering lower corticosteroid doses. It is likely that underlying maternal conditions contribute to intrauterine growth restriction and decreased birth weight, but it is unclear to what extent these maternal conditions contribute to the increased risk of orofacial clefts. Animal Data Prednisolone, the active metabolite of prednisone, administered during the period of organogenesis, has been shown to be teratogenic in rats, rabbits, hamsters, and mice with increased incidence of cleft palate in offspring. In teratogenicity studies, cleft palate along with elevation of fetal lethality (or increase in resorptions) and reductions in fetal body weight were seen in rats at maternal doses of 30 mg/kg (equivalent to 290 mg in a 60 kg individual based on mg/m 2 body surface comparison) and higher. Cleft palate was observed in mice at a maternal dose of 20 mg/kg (equivalent to 100 mg in a 60 kg individual based on mg/m 2 comparison). Additionally, constriction of the ductus arteriosus has been observed in fetuses of pregnant rats exposed to prednisolone. RAYOS was not formally evaluated in animal reproduction studies. 8.2 Lactation Risk Summary Prednisolone has been found to be present in human milk following administration to lactating women. Published reports suggest infant daily doses are estimated to be less than 1% of the maternal daily dose. No adverse effects in the breastfed infant have been reported following maternal exposure of prednisolone during breastfeeding. There are no available data on the effects of prednisolone on milk production. High doses of corticosteroids administered to lactating women for long periods could potentially produce problems in the breastfed infant including growth and development and interfere with endogenous corticosteroid production (see Clinical Considerations ) [see Use in Specific Populations (8.4) ] . The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for RAYOS and any potential adverse effects on the breastfed child from RAYOS or from the mother's underlying condition. Clinical Considerations In order to minimize exposure, the lowest dose should be prescribed to lactating women to achieve the desired clinical effect. Data Human Data Reports suggest that prednisolone concentrations in human milk are 5% to 25% of maternal serum levels, and that total infant daily doses are small, about 0.14% of the maternal daily dose. 8.4 Pediatric Use The efficacy and safety of prednisone in the pediatric population are based on the well-established course of effect of corticosteroids which is similar in pediatric and adult populations. Published studies provide evidence of efficacy and safety in pediatric patients for the treatment of nephrotic syndrome (> 2 years of age), and aggressive lymphomas and leukemias (> 1 month of age). However, some of these conclusions and other indications for pediatric use of corticosteroid, e.g., severe asthma and wheezing, are based on adequate and well-controlled trials conducted in adults, on the premises that the course of the diseases and their pathophysiology are considered to be substantially similar in both populations. The adverse effects of prednisone in pediatric patients are similar to those in adults [see Adverse Reactions (6) ] . Like adults, pediatric patients should be carefully observed with frequent measurements of blood pressure, weight, height, intraocular pressure, and clinical evaluation for the presence of infection, psychosocial disturbances, thromboembolism, peptic ulcers, cataracts, and osteoporosis. Children who are treated with corticosteroids by any route, including systemically administered corticosteroids, may experience a decrease in their growth velocity. This negative impact of corticosteroids on growth has been observed at low systemic doses and in the absence of laboratory evidence of HPA axis suppression (i.e., cosyntropin stimulation and basal cortisol levels). Growth velocity may therefore be a more sensitive indicator of systemic corticosteroid exposure in children than some commonly used tests of HPA axis function. The linear growth of children treated with corticosteroids by any route should be monitored, and the potential growth effects of prolonged treatment should be weighed against clinical benefits obtained and the availability of other treatment alternatives. In order to minimize the potential growth effects of corticosteroids, children should be titrated to the lowest effective dose [see Warnings and Precautions (5.9) ] . 8.5 Geriatric Use No overall differences in safety or effectiveness were observed between elderly subjects and younger subjects, and other reported clinical experience with prednisone has not identified differences in responses between the elderly and younger patients. However, the incidence of corticosteroid-induced side effects may be increased in geriatric patients and are dose-related. Osteoporosis is the most frequently encountered complication, which occurs at a higher incidence rate in corticosteroid-treated geriatric patients as compared to younger populations and in age-matched controls. Losses of bone mineral density appear to be greatest early on in the course of treatment and may recover over time after steroid withdrawal or use of lower doses (i.e., ≤ 5 mg/day). Prednisone doses of 7.5 mg/day or higher have been associated with an increased relative risk of both vertebral and nonvertebral fractures, even in the presence of higher bone density compared to patients with involution osteoporosis. Routine screening of geriatric patients, including regular assessments of bone mineral density and institution of fracture prevention strategies, along with regular review of prednisone indication should be undertaken to minimize complications and keep the prednisolone dose at the lowest acceptable level. Co-administration of certain bisphosphonates have been shown to retard the rate of bone loss in corticosteroid-treated males and postmenopausal females, and these agents are recommended in the prevention and treatment of corticosteroid-induced osteoporosis [see Warnings and Precautions (5.6) ] . It has been reported that equivalent weight-based doses yield higher total and unbound prednisolone plasma concentrations and reduced renal and non-renal clearance in elderly patients compared to younger populations. Dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING RAYOS delayed-release tablets (1 mg prednisone) are pale yellowish-white, round, unscored tablets embossed with "NP 1" on one side and supplied as: NDC Number Size 75987-020-01 Bottle of 30 tablets 75987-020-02 Bottle of 100 tablets RAYOS delayed-release tablets (2 mg prednisone) are yellowish-white, round, unscored tablets embossed with "NP 2" on one side and supplied as: NDC Number Size 75987-021-01 Bottle of 30 tablets 75987-021-02 Bottle of 100 tablets RAYOS delayed-release tablets (5 mg prednisone) are light yellow, round, unscored tablets embossed with "NP 5" on one side and supplied as: NDC Number Size 75987-022-01 Bottle of 30 tablets 75987-022-02 Bottle of 100 tablets Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F). [See USP Controlled Room Temperature]. Protect RAYOS tablets from light and moisture. Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
| NDC Number | Size |
|---|---|
| 75987-020-01 | Bottle of 30 tablets |
| 75987-020-02 | Bottle of 100 tablets |
| NDC Number | Size |
|---|---|
| 75987-021-01 | Bottle of 30 tablets |
| 75987-021-02 | Bottle of 100 tablets |
| NDC Number | Size |
|---|---|
| 75987-022-01 | Bottle of 30 tablets |
| 75987-022-02 | Bottle of 100 tablets |
Storage and handling
Information about safe storage and handling of the drug product.Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F). [See USP Controlled Room Temperature]. Protect RAYOS tablets from light and moisture. Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API