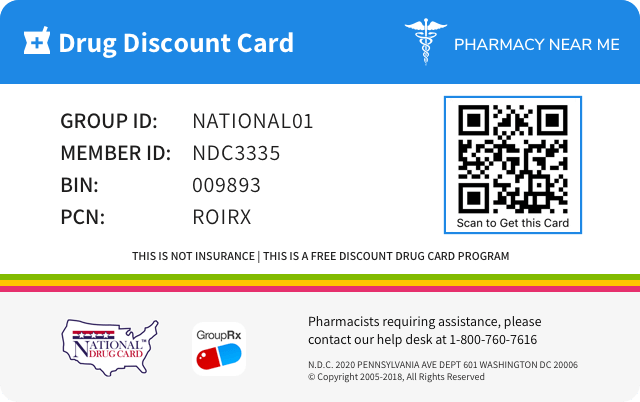
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 60505-4129 | ||||||
|---|---|---|---|---|---|---|---|
| Drug Name | Oxcarbazepine |
||||||
| Type | Generic | ||||||
| Pharm Class | Anti-epileptic Agent [EPC], Decreased Central Nervous System Disorganized Electrical Activity [PE] |
||||||
| Active Ingredients |
|
||||||
| Route | ORAL | ||||||
| Dosage Form | TABLET, EXTENDED RELEASE | ||||||
| RxCUI drug identifier | 1365653, 1365842, 1365844 |
||||||
| Application Number | ANDA213369 | ||||||
| Labeler Name | Apotex Corp. | ||||||
| Packages |
|
||||||
| Check if available Online | Get Medication Prices online with Discount |
Abuse
Information about the types of abuse that can occur with the drug and adverse reactions pertinent to those types of abuse, primarily based on human data. May include descriptions of particularly susceptible patient populations.9.2 Abuse The abuse potential of oxcarbazepine extended-release tablets has not been evaluated in human studies. Oxcarbazepine extended-release tablets are not habit forming, and is not expected to encourage abuse.
Dependence
Information about characteristic effects resulting from both psychological and physical dependence that occur with the drug, the quantity of drug over a period of time that may lead to tolerance or dependence, details of adverse effects related to chronic abuse and the effects of abrupt withdrawl, procedures necessary to diagnose the dependent state, and principles of treating the effects of abrupt withdrawal.9.3 Dependence Intragastric injections of oxcarbazepine to four cynomolgus monkeys demonstrated no signs of physical dependence as measured by the desire to self-administer oxcarbazepine by lever pressing activity.
Drug abuse and dependence
Information about whether the drug is a controlled substance, the types of abuse that can occur with the drug, and adverse reactions pertinent to those types of abuse.9 DRUG ABUSE AND DEPENDENCE 9.2 Abuse The abuse potential of oxcarbazepine extended-release tablets has not been evaluated in human studies. Oxcarbazepine extended-release tablets are not habit forming, and is not expected to encourage abuse. 9.3 Dependence Intragastric injections of oxcarbazepine to four cynomolgus monkeys demonstrated no signs of physical dependence as measured by the desire to self-administer oxcarbazepine by lever pressing activity.
Overdosage of OXCARBAZEPINE
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE 10.1 Human Overdose Experience Isolated cases of overdose with immediate-release oxcarbazepine have been reported. The maximum dose taken was approximately 48,000 mg. All patients recovered with symptomatic treatment. Nausea, vomiting, somnolence, aggression, agitation, hypotension, and tremor each occurred in more than one patient. Coma, confusional state, convulsion, dyscoordination, depressed level of consciousness, diplopia, dizziness, dyskinesia, dyspnea, QT prolongation, headache, miosis, nystagmus, overdose, decreased urine output, and blurred vision also occurred. 10.2 Treatment and Management There is no specific antidote for oxcarbazepine extended-release tablets overdose. Administer symptomatic and supportive treatment as appropriate. Options include removal of the drug by gastric lavage and/or inactivation by administering activated charcoal.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS The following serious adverse reactions are described in other sections of the labeling: Hyponatremia [see Warnings and Precautions ( 5.1 )] Anaphylactic Reactions and Angioedema [see Warnings and Precautions ( 5.2 )] Cross Hypersensitivity Reaction to Carbamazepine [see Warnings and Precautions ( 5.3 )] Serious Dermatological Reactions [see Warnings and Precautions ( 5.4 )] Suicidal Behavior and Ideation [see Warnings and Precautions ( 5.5 )] Withdrawal of AEDs [see Warnings and Precautions ( 5.6 )] Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multi-Organ Hypersensitivity [see Warnings and Precautions ( 5.7 )] Hematologic Reactions [see Warnings and Precautions ( 5.8 )] Risk of Seizures in the Pregnant Patient [see Warnings and Precautions ( 5.9 )] Most commonly observed (≥5% and more frequent than placebo) adverse reactions in adults were dizziness, somnolence, headache, balance disorder, tremor, vomiting, diplopia, asthenia, and fatigue. ( 6.1 ) Adverse reactions in pediatric patients are similar to those seen in adult patients. To report SUSPECTED ADVERSE REACTIONS, contact Apotex Corp. at 1-800-706-5575 or contact FDA at 1-800-FDA-1088 or www.fda.gov/medwatch 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice. The safety data presented below are from 384 patients with partial-onset seizures who received oxcarbazepine extended-release tablets (366 adults and 18 pediatric patients) with concomitant AEDs. In addition, safety data presented below are from a total of 2,288 patients with seizure disorders treated with immediate-release oxcarbazepine; 1,832 were adults and 456 were pediatric patients. Most Common Adverse Reactions Reported by Adult Patients Receiving Concomitant AEDs in Oxcarbazepine Extended-Release Tablets Clinical Studies Table 3 lists adverse reactions that occurred in at least 2% of adult patients with epilepsy treated with oxcarbazepine extended-release tablets or placebo and concomitant AEDs and that were numerically more common in the patients treated with any dosage of oxcarbazepine extended-release tablets than in patients receiving placebo. Table 3: Adverse Reaction Incidence in a Controlled Clinical Study of Oxcarbazepine Extended-Release Tablets with Concomitant AEDs in Adults* Oxcarbazepine extended-release tablets 2,400 mg/day N=123 % Oxcarbazepine extended-release tablets 1,200 mg/day N=122 % Placebo N=121 % Any System / Any Term 69 57 55 Nervous System Disorders Dizziness 41 20 15 Somnolence 14 12 9 Headache 15 8 7 Balance Disorder 7 5 5 Tremor 1 5 2 Nystagmus 3 3 1 Ataxia 1 3 1 Gastrointestinal Disorders Vomiting 15 6 9 Abdominal Pain Upper 0 3 1 Dyspepsia 0 3 1 Gastritis 0 3 2 Eye Disorders Diplopia 13 10 4 Vision Blurred 1 4 3 Visual Impairment 1 3 0 General Disorders and Administration Site Conditions Asthenia 7 3 1 Fatigue 3 6 1 Gait Disturbance 0 3 1 Drug Intolerance 2 0 0 Infections and Infestations Nasopharyngitis 0 3 0 Sinusitis 0 3 2 * Reported by ≥ 2% of patients treated with oxcarbazepine extended-release tablets and numerically more frequent than in the placebo group The overall incidence of adverse reactions appeared to be dose related, particularly during the titration period. The most commonly observed (≥5%) adverse reactions seen in association with oxcarbazepine extended-release tablets and more frequent than in placebo-treated patients were: dizziness, somnolence, headache, balance disorder, tremor, vomiting, diplopia, and asthenia. Adverse Reactions Associated with Discontinuation of Oxcarbazepine Extended-Release Tablets Treatment: Approximately 23.3% of the 366 adult patients receiving oxcarbazepine extended-release tablets in clinical studies discontinued treatment because of an adverse reaction. The adverse reactions most commonly associated with discontinuation of oxcarbazepine extended-release tablets (reported by ≥2%) were: dizziness (9.8%), vomiting (5.3%), nausea (3.7%), diplopia (3.2%), and somnolence (2.4%). Adjunctive Therapy with Oxcarbazepine Extended-Release Tablets in Pediatric Patients 6 to Less than 17 Years of Age Previously Treated with other AEDs In a pharmacokinetic study in 18 pediatric patients (including patients 6 to less than 17 years of age) with partial-onset seizures treated with different dosages of oxcarbazepine extended-release tablets, the observed adverse reactions seen in association with oxcarbazepine extended-release tablets were similar to those seen in adults. Most Common Adverse Reactions in Immediate-Release Oxcarbazepine Controlled Clinical Studies Controlled Clinical Studies of Adjunctive Therapy with Immediate-Release Oxcarbazepine in Adults Previously Treated with other AEDs: Table 4 lists adverse reactions that occurred in at least 2% of adult patients with epilepsy treated with immediate-release oxcarbazepine or placebo with concomitant AEDs and that were numerically more common in the patients treated with any dosage of immediate-release oxcarbazepine than in placebo. As immediate-release oxcarbazepine and oxcarbazepine extended-release tablets were not examined in the same trial, adverse event frequencies cannot be directly compared between the two formulations. Table 4: Adverse Reaction Incidence in a Controlled Clinical Study of Immediate Release Oxcarbazepine with Concomitant AEDs in Adults* Immediate-Release Oxcarbazepine Dosage (mg/day) Placebo N = 166 % OXC 600 N = 163 % OXC 1,200 N = 171 % OXC 2,400 N = 126 % Body as a Whole Fatigue 15 12 15 7 Asthenia 6 3 6 5 Edema Legs 2 1 2 1 Weight Increase 1 2 2 1 Feeling Abnormal 0 1 2 0 Cardiovascular System Hypotension 0 1 2 0 Digestive System Nausea 15 25 29 10 Vomiting 13 25 36 5 Pain Abdominal 10 13 11 5 Diarrhea 5 6 7 6 Dyspepsia 5 5 6 2 Constipation 2 2 6 4 Gastritis 2 1 2 1 Metabolic and Nutritional Disorders Hyponatremia 3 1 2 1 Musculoskeletal System Muscle Weakness 1 2 2 0 Sprains and Strains 0 2 2 1 Nervous System Headache 32 28 26 23 Dizziness 36 32 49 13 Somnolence 20 28 36 12 Ataxia 9 17 31 5 Nystagmus 7 20 26 5 Gait Abnormal 5 10 17 1 Insomnia 4 2 3 1 Tremor 3 8 16 5 Nervousness 2 4 2 1 Agitation 1 1 2 1 Coordination Abnormal 1 3 2 1 EEG Abnormal 0 0 2 0 Speech Disorder 1 1 3 0 Confusion 1 1 2 1 Cranial Injury NOS 1 0 2 1 Dysmetria 1 2 3 0 Thinking Abnormal 0 2 4 0 Respiratory System Rhinitis 2 4 5 4 Skin and Appendages Acne 1 2 2 0 Special Senses Diplopia 14 30 40 5 Vertigo 6 12 15 2 Vision Abnormal 6 14 13 4 Accommodation Abnormal 0 0 2 0 * Events in at least 2% of patients treated with 2,400 mg/day of immediate-release oxcarbazepine and numerically more frequent than in the placebo group Other Reactions Observed in Association with the Administration of Immediate-Release Oxcarbazepine In the paragraphs that follow, the adverse reactions, other than those in the preceding tables or text, that occurred in a total of 565 children and 1,574 adults exposed to immediate-release oxcarbazepine and that are reasonably likely to be related to drug use are presented. Events common in the population, events reflecting chronic illness and events likely to reflect concomitant illness are omitted particularly if minor. They are listed in order of decreasing frequency. Because the reports cite reactions observed in open-label and uncontrolled trials, the role of immediate-release oxcarbazepine in their causation cannot be reliably determined. Body as a Whole: fever, malaise, pain chest precordial, rigors, weight decrease. Cardiovascular System: bradycardia, cardiac failure, cerebral hemorrhage, hypertension, hypotension postural, palpitation, syncope, tachycardia. Digestive System: appetite increased, blood in stool, cholelithiasis, colitis, duodenal ulcer, dysphagia, enteritis, eructation, esophagitis, flatulence, gastric ulcer, gingival bleeding, gum hyperplasia, hematemesis, hemorrhage rectum, hemorrhoids, hiccup, mouth dry, pain biliary, pain right hypochondrium, retching, sialoadenitis, stomatitis, stomatitis ulcerative. Hematologic and Lymphatic System: thrombocytopenia. Laboratory Abnormality: gamma-GT increased, hyperglycemia, hypocalcemia, hypoglycemia, hypokalemia, liver enzymes elevated, serum transaminase increased. Musculoskeletal System: hypertonia muscle. Nervous System: aggressive reaction, amnesia, anguish, anxiety, apathy, aphasia, aura, convulsions aggravated, delirium, delusion, depressed level of consciousness, dysphonia, dystonia, emotional lability, euphoria, extrapyramidal disorder, feeling drunk, hemiplegia, hyperkinesia, hyperreflexia, hypoesthesia, hypokinesia, hyporeflexia, hypotonia, hysteria, libido decreased, libido increased, manic reaction, migraine, muscle contractions involuntary, nervousness, neuralgia, oculogyric crisis, panic disorder, paralysis, paroniria, personality disorder, psychosis, ptosis, stupor, tetany. Respiratory System: asthma, bronchitis, coughing, dyspnea, epistaxis, laryngismus, pleurisy. Skin and Appendages: acne, alopecia, angioedema, bruising, dermatitis contact, eczema, facial rash, flushing, folliculitis, heat rash, hot flushes, photosensitivity reaction, pruritus genital, psoriasis, purpura, rash erythematous, rash maculopapular, vitiligo, urticaria. Special Senses: accommodation abnormal, cataract, conjunctival hemorrhage, edema eye, hemianopia, mydriasis, otitis externa, photophobia, scotoma, taste perversion, tinnitus, xerophthalmia. Urogenital and Reproductive System: dysuria, hematuria, intermenstrual bleeding, leukorrhea, menorrhagia, micturition frequency, pain renal, pain urinary tract, polyuria, priapism, renal calculus, urinary tract infection. Other: Systemic lupus erythematosus. Laboratory Tests Serum sodium levels below 125 mmol/L have been observed in patients treated with immediate-release oxcarbazepine [see Warnings and Precautions ( 5.1 )] . Experience from clinical trials with immediate-release oxcarbazepine indicates that serum sodium levels return toward normal when the dosage is reduced or discontinued, or when the patient was treated conservatively (e.g., fluid restriction). Laboratory data from clinical trials suggest that immediate-release oxcarbazepine use was associated with decreases in T4, without changes in T3 or TSH. 6.2 Postmarketing and Other Experience The following adverse reactions have been observed in named patient programs or post-marketing experience with immediate-release oxcarbazepine or oxcarbazepine extended-release tablets. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Body as a Whole: multi-organ hypersensitivity disorders characterized by features such as rash, fever, lymphadenopathy, abnormal liver function tests, eosinophilia, and arthralgia [see Warnings and Precautions ( 5.7 )] Cardiovascular System: atrioventricular block Digestive System: pancreatitis and/or lipase and/or amylase increase Hematologic and Lymphatic Systems: aplastic anemia [see Warnings and Precautions ( 5.8 )] Immune System Disorders: anaphylaxis [see Warnings and Precautions ( 5.2 )] Metabolism and Nutrition Disorders: hypothyroidism and syndrome of inappropriate antidiuretic hormone secretion (SIADH) Skin and Subcutaneous Tissue Disorders: erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis [see Warnings and Precautions ( 5.4 )] , Acute Generalized Exanthematous Pustulosis (AGEP) Musculoskeletal, Connective Tissue and Bone Disorders: There have been reports of decreased bone mineral density, osteoporosis and fractures in patients on long-term therapy with immediate-release oxcarbazepine.
| Oxcarbazepine extended-release tablets 2,400 mg/day N=123 % | Oxcarbazepine extended-release tablets 1,200 mg/day N=122 % | Placebo N=121 % | |
| Any System / Any Term | 69 | 57 | 55 |
| Dizziness | 41 | 20 | 15 |
| Somnolence | 14 | 12 | 9 |
| Headache | 15 | 8 | 7 |
| Balance Disorder | 7 | 5 | 5 |
| Tremor | 1 | 5 | 2 |
| Nystagmus | 3 | 3 | 1 |
| Ataxia | 1 | 3 | 1 |
| Vomiting | 15 | 6 | 9 |
| Abdominal Pain Upper | 0 | 3 | 1 |
| Dyspepsia | 0 | 3 | 1 |
| Gastritis | 0 | 3 | 2 |
| Diplopia | 13 | 10 | 4 |
| Vision Blurred | 1 | 4 | 3 |
| Visual Impairment | 1 | 3 | 0 |
| Asthenia | 7 | 3 | 1 |
| Fatigue | 3 | 6 | 1 |
| Gait Disturbance | 0 | 3 | 1 |
| Drug Intolerance | 2 | 0 | 0 |
| Nasopharyngitis | 0 | 3 | 0 |
| Sinusitis | 0 | 3 | 2 |
| * Reported by ≥ 2% of patients treated with oxcarbazepine extended-release tablets and numerically more frequent than in the placebo group | |||
| Fatigue | 15 | 12 | 15 | 7 |
| Asthenia | 6 | 3 | 6 | 5 |
| Edema Legs | 2 | 1 | 2 | 1 |
| Weight Increase | 1 | 2 | 2 | 1 |
| Feeling Abnormal | 0 | 1 | 2 | 0 |
| Hypotension | 0 | 1 | 2 | 0 |
| Nausea | 15 | 25 | 29 | 10 |
| Vomiting | 13 | 25 | 36 | 5 |
| Pain Abdominal | 10 | 13 | 11 | 5 |
| Diarrhea | 5 | 6 | 7 | 6 |
| Dyspepsia | 5 | 5 | 6 | 2 |
| Constipation | 2 | 2 | 6 | 4 |
| Gastritis | 2 | 1 | 2 | 1 |
| Hyponatremia | 3 | 1 | 2 | 1 |
| Muscle Weakness | 1 | 2 | 2 | 0 |
| Sprains and Strains | 0 | 2 | 2 | 1 |
| Headache | 32 | 28 | 26 | 23 |
| Dizziness | 36 | 32 | 49 | 13 |
| Somnolence | 20 | 28 | 36 | 12 |
| Ataxia | 9 | 17 | 31 | 5 |
| Nystagmus | 7 | 20 | 26 | 5 |
| Gait Abnormal | 5 | 10 | 17 | 1 |
| Insomnia | 4 | 2 | 3 | 1 |
| Tremor | 3 | 8 | 16 | 5 |
| Nervousness | 2 | 4 | 2 | 1 |
| Agitation | 1 | 1 | 2 | 1 |
| Coordination Abnormal | 1 | 3 | 2 | 1 |
| EEG Abnormal | 0 | 0 | 2 | 0 |
| Speech Disorder | 1 | 1 | 3 | 0 |
| Confusion | 1 | 1 | 2 | 1 |
| Cranial Injury NOS | 1 | 0 | 2 | 1 |
| Dysmetria | 1 | 2 | 3 | 0 |
| Thinking Abnormal | 0 | 2 | 4 | 0 |
| Rhinitis | 2 | 4 | 5 | 4 |
| Acne | 1 | 2 | 2 | 0 |
| Diplopia | 14 | 30 | 40 | 5 |
| Vertigo | 6 | 12 | 15 | 2 |
| Vision Abnormal | 6 | 14 | 13 | 4 |
| Accommodation Abnormal | 0 | 0 | 2 | 0 |
| * Events in at least 2% of patients treated with 2,400 mg/day of immediate-release oxcarbazepine and numerically more frequent than in the placebo group | ||||
OXCARBAZEPINE Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS Phenytoin, Carbamazepine, and Phenobarbital: Coadministration decreased blood levels of an active metabolite of oxcarbazepine extended-release tablets: Greater dosage of oxcarbazepine extended-release tablets may be required. ( 2.5 , 7.2 ) Oral Contraceptives: Advise patients that oxcarbazepine extended-release tablets may decrease the effectiveness of hormonal contraceptives. Additional non-hormonal forms of contraception are recommended. ( 7.3 ) 7.1 Effect of Oxcarbazepine Extended-Release Tablets on Other Drugs It is recommended that the plasma levels of phenytoin be monitored during the period of oxcarbazepine extended-release tablets titration and dosage modification [see Clinical Pharmacology ( 12.3 )] . A decrease in the dosage of phenytoin may be required. 7.2 Effect of Other Drugs on Oxcarbazepine Extended-Release Tablets If oxcarbazepine extended-release tablets and strong CYP3A4 inducers or UGT inducers (e.g., rifampin, carbamazepine, phenytoin and phenobarbital) are administered concurrently, it is recommended that the plasma levels of MHD be monitored during the period of oxcarbazepine extended-release tablets titration [see Clinical Pharmacology ( 12.3 )] . Dosage adjustment of oxcarbazepine extended-release tablets may be required after initiation, dosage modification, or discontinuation of such inducers [see Dosage and Administration ( 2.5 )]. 7.3 Hormonal Contraceptives Concurrent use of immediate-release oxcarbazepine with hormonal contraceptives may render these contraceptives less effective [see Clinical Pharmacology ( 12.3 )] . Studies with other oral or implant contraceptives have not been conducted.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action The pharmacological activity of oxcarbazepine extended-release tablets are primarily exerted through the 10-monohydroxy metabolite (MHD) of oxcarbazepine [see Clinical Pharmacology ( 12.3 )] . The precise mechanism by which oxcarbazepine and MHD exert their antiseizure effect is unknown; however, in vitro electrophysiological studies indicate that they produce blockade of voltage-sensitive sodium channels, resulting in stabilization of hyperexcited neural membranes, inhibition of repetitive neuronal firing, and diminution of propagation of synaptic impulses. These actions are thought to be important in the prevention of seizure spread in the intact brain. In addition, increased potassium conductance and modulation of high-voltage activated calcium channels may contribute to the anticonvulsant effects of the drug. No significant interactions of oxcarbazepine or MHD with brain neurotransmitter or modulator receptor sites have been demonstrated. 12.2 Pharmacodynamics Oxcarbazepine and its active metabolite (MHD) exhibit anticonvulsant properties in animal seizure models. They protected rodents against electrically induced tonic extension seizures and, to a lesser degree, chemically induced clonic seizures, and abolished or reduced the frequency of chronically recurring focal seizures in Rhesus monkeys with aluminum implants. No development of tolerance (i.e., attenuation of anticonvulsive activity) was observed in the maximal electroshock test when mice and rats were treated daily for five days and four weeks, respectively, with oxcarbazepine or MHD. 12.3 Pharmacokinetics Following oral administration, oxcarbazepine is absorbed and extensively metabolized to its pharmacologically active 10-monohydroxy metabolite (MHD), which is responsible for most antiepileptic activity. In clinical studies of oxcarbazepine extended-release tablets, the elimination half-life of oxcarbazepine was between 7 and 11 hours; the elimination half-life of MHD is between 9 and 11 hours. In a mass balance study in humans, only 2% of total radioactivity in plasma after administration of immediate-release oxcarbazepine was due to unchanged oxcarbazepine, with approximately 70% present as MHD, and the remainder attributable to minor metabolites. Absorption Oxcarbazepine extended-release tablets administered as a once daily dosage is not bioequivalent to the same total dosage of the immediate-release formulation given twice daily at steady state. Steady state plasma concentrations of MHD are reached within 5 days when oxcarbazepine extended-release tablets are given once daily. At steady state, when 1,200 mg oxcarbazepine extended-release tablets were given once daily, MHD C max occurred 7 hours post-dose. At steady state, oxcarbazepine extended-release tablets given once daily produced MHD exposures (AUC and C max ) about 19% lower and MHD minimum concentrations (C min ) about 16% lower than the immediate-release oxcarbazepine given twice daily when administered at the same 1,200 mg total daily dosage. When oxcarbazepine extended-release tablets were administered at an equivalent 600 mg single dose (4 x 150 mg tablets, 2 x 300 mg tablets, or 1 x 600 mg tablet), equivalent MHD exposures (AUC) were observed. Following a single dose of oxcarbazepine extended-release tablets (1 x 150 mg tablets, 1 x 300 mg tablets, or 1 x 600 mg tablet), the pharmacokinetics of MHD are not linear and show greater than dose proportional increase in AUC and less than proportional increase in C max : AUC increases 2.4-fold and C max increases 1.9-fold with a 2-fold increase in dose. Effect of Food : Single dose administration of 600 mg oxcarbazepine extended-release tablets following a high fat meal (800 to 1,000 calories) produced MHD exposure (AUC) equivalent to that produced under fasting conditions. Peak MHD concentration (C max ) was about 60% higher and occurred 2 hours earlier under fed conditions than under fasting conditions. The increase in C max , even without a significant change in the overall exposure, should be considered by the prescriber especially during the titration phase, when some adverse reactions are most likely to occur coincidentally with peak levels. Distribution The apparent volume of distribution of MHD is 49 L. Approximately 40% of MHD is bound to serum proteins, predominantly to albumin. Binding is independent of the serum concentration within the therapeutically relevant range. Oxcarbazepine and MHD do not bind to alpha-1-acid glycoprotein. Elimination Metabolism Oxcarbazepine is rapidly reduced by cytosolic enzymes in the liver to MHD, which is primarily responsible for the pharmacological effect of oxcarbazepine extended-release tablets. MHD is metabolized further by conjugation with glucuronic acid. Minor amounts (4% of the dose) are oxidized to the pharmacologically inactive 10,11-dihydroxy metabolite (DHD). Excretion Oxcarbazepine is cleared from the body mostly in the form of metabolites which are predominantly excreted by the kidneys. More than 95% of a dose of immediate-release oxcarbazepine appears in the urine, with less than 1% as unchanged oxcarbazepine. Fecal excretion accounts for less than 4% of an administered dose. Approximately 80% of the dose is excreted in the urine either as glucuronides of MHD (49%) or as unchanged MHD (27%); the inactive DHD accounts for approximately 3% and conjugates of MHD and oxcarbazepine account for 13% of the dose. The half-life of the parent was about two hours, while the half-life of MHD was about nine hours after the immediate-release formulation. A population pharmacokinetic model for oxcarbazepine extended-release tablets was developed in healthy normal adults and applied to pharmacokinetic data in patients with epilepsy. For oxcarbazepine, systemic parameters were scaled allometrically, suggesting that steady state oxcarbazepine exposure will vary inversely with weight. Specific Populations Geriatric Patients No studies with oxcarbazepine extended-release tablets in elderly patients have been completed [see Use in Specific Populations ( 8.5 )]. Following administration of single (300 mg) and multiple (600 mg/day) doses of immediate-release oxcarbazepine to elderly volunteers (60 to 82 years of age), the maximum plasma concentrations and AUC values of MHD were 30% to 60% higher than in younger volunteers (18 to 32 years of age). Comparisons of creatinine clearance in young and elderly volunteers indicate that the difference was due to age-related reductions in creatinine clearance. Pediatric Patients A pharmacokinetic study of oxcarbazepine was performed in 18 pediatric patients with epilepsy, which included patients 6 to less than 17 years of age, after multiple doses. The population pharmacokinetic model suggested that dosing of pediatric patients with oxcarbazepine can be determined based on body weight. Weight-normalized doses in pediatric patients should produce MHD exposures (AUC) comparable to that in typical adults, with oxcarbazepine exposures ~40% higher in children than in adults [see Use in Specific Populations ( 8.4 )] . The pharmacokinetics of oxcarbazepine in pediatric patients are similar when used as monotherapy or as adjunctive therapy for the treatment of partial-onset seizures. Pediatric Patients with Obesity A population PK analysis of immediate-release oxcarbazepine was conducted that included n=54 obese and non-obese pediatric patients 6 to <18 years of age to evaluate the potential impact of obesity on plasma oxcarbazepine exposures. Obesity was defined as BMI ≥95th percentile for age and sex based on CDC 2,000 growth chart recommendations. Simulated results from this analysis suggested that the target maintenance doses for oxcarbazepine, applied in pediatric patients ≥6 years of age, produced equivalent steady-state exposure of MHD between pediatric patients with and without obesity. This finding is consistent when using total body weight, or when using fat-free mass in the simulations. Dosage adjustment according to obesity status is not necessary. Male and Female Patients The effects of gender have not been studied for oxcarbazepine. No gender-related pharmacokinetic differences have been observed in children, adults, or the elderly with immediate-release oxcarbazepine. Racial or Ethnic Groups The effects of race have not been studied for oxcarbazepine. Patients with Renal or Hepatic Impairment The effects of renal or hepatic impairment have not been studied for oxcarbazepine [see Use in Specific Populations ( 8.6 , 8.7 )]. Based on investigations with immediate-release oxcarbazepine, there is a linear correlation between creatinine clearance and the renal clearance of MHD. When immediate-release oxcarbazepine is administered as a single 300 mg dose in renally-impaired patients (creatinine clearance <30 mL/min), the elimination half-life of MHD is prolonged to 19 hours, with a two-fold increase in AUC. Dosage adjustment is recommended in these patients [see Dosage and Administration ( 2.3 ) and Use in Special Populations ( 8.6 )]. The pharmacokinetics and metabolism of immediate-release oxcarbazepine and MHD were evaluated in healthy volunteers and hepatically impaired subjects after a single 900 mg oral dose. Mild-to-moderate hepatic impairment did not affect the pharmacokinetics of immediate-release oxcarbazepine and MHD. The pharmacokinetics of oxcarbazepine and MHD have not been evaluated in severe hepatic impairment, and therefore it is not recommended in these patients [see Use in Specific Populations (8.7)]. Pregnant Women Due to physiological changes during pregnancy, MHD plasma levels may gradually decrease throughout pregnancy [see Use in Specific Populations ( 8.1 )]. Drug Interaction Studies In Vitro: Oxcarbazepine can inhibit CYP2C19 and induce CYP3A4/5 with potentially important effects on plasma concentrations of other drugs. In addition, several AEDs that are cytochrome P450 inducers can decrease plasma concentrations of oxcarbazepine and MHD. Oxcarbazepine was evaluated in human liver microsomes to determine its capacity to inhibit the major cytochrome P450 enzymes responsible for the metabolism of other drugs. Results demonstrate that oxcarbazepine and its pharmacologically active 10-monohydroxy metabolite (MHD) have little or no capacity to function as inhibitors for most of the human cytochrome P450 enzymes evaluated (CYP1A2, CYP2A6, CYP2C9, CYP2D6, CYP2E1, CYP4A9 and CYP4A11) with the exception of CYP2C19 and CYP3A4/5. Although inhibition of CYP3A4/5 by oxcarbazepine and MHD did occur at high concentrations, it is not likely to be of clinical significance. The inhibition of CYP2C19 by oxcarbazepine and MHD, is clinically relevant. In vitro , the UDP-glucuronyl transferase level was increased, indicating induction of this enzyme. Increases of 22% with MHD and 47% with oxcarbazepine were observed. As MHD, the predominant plasma substrate, is only a weak inducer of UDP-glucuronyl transferase, it is unlikely to have an effect on drugs that are mainly eliminated by conjugation through UDP-glucuronyl transferase (e.g., valproic acid, lamotrigine). In addition, oxcarbazepine and MHD induce a subgroup of the cytochrome P450 3A family (CYP3A4 and CYP3A5) responsible for the metabolism of dihydropyridine calcium antagonists, oral contraceptives and cyclosporine resulting in a lower plasma concentration of these drugs. Several AEDs that are cytochrome P450 inducers can decrease plasma concentrations of oxcarbazepine and MHD. No autoinduction has been observed with immediate-release oxcarbazepine. As binding of MHD to plasma proteins is low (40%), clinically significant interactions with other drugs through competition for protein binding sites are unlikely. In Vivo: Other Antiepileptic Drugs Potential interactions between immediate-release oxcarbazepine and other AEDs were assessed in clinical studies. The effect of these interactions on mean AUCs and C min are summarized in Table 5 [see Drug Interactions (7.1, 7.2)]. Table 5: AED Drug Interactions with Immediate-Release (IR) Oxcarbazepine AED Coadministered (daily dosage) IR-Oxcarbazepine (daily dosage) Influence of IR- Oxcarbazepine on AED Concentration Mean Change [90% Confidence Interval] Influence of AED on MHD Concentration (Mean Change, 90% Confidence Interval) Carbamazepine (400 to 2,000 mg) 900 mg nc 1 40% decrease [CI: 17% decrease, 57% decrease] Phenobarbital (100 to 150 mg) 600 to 1,800 mg 14% increase [CI: 2% increase, 24% increase] 25% decrease [CI: 12% decrease, 51% decrease] Phenytoin (250 to 500 mg) 600 to 1,800 > 1,200 to 2,400 nc 1,2 up to 40% increase 3 [CI: 12% increase, 60% increase] 30% decrease [CI: 3% decrease, 48% decrease] Valproic Acid (400 to 2,800 mg) 600 to 1,800 nc 1 18% decrease [CI: 13% decrease, 40% decrease] Lamotrigine (200 mg) 1,200 nc 1 nc 1 1 nc denotes a mean change of less than 10% 2 Pediatrics 3 Mean increase in adults at high doses of immediate-release oxcarbazepine Hormonal Contraceptives Coadministration of immediate-release oxcarbazepine with an oral contraceptive has been shown to influence the plasma concentrations of two components of hormonal contraceptives, ethinylestradiol (EE) and levonorgestrel (LNG). The mean AUC values of EE were decreased by 48% [90% CI: 22 to 65] in one study and 52% [90% CI: 38 to 52] in another study. The mean AUC values of LNG were decreased by 32% [90% CI: 20 to 45] in one study and 52% [90% CI: 42 to 52] in another study. Other Drug Interactions Calcium Antagonists: After repeated coadministration of immediate-release oxcarbazepine, the AUC of felodipine was lowered by 28% [90% CI: 20 to 33]. Verapamil produced a decrease of 20% [90% CI: 18 to 27] of the plasma levels of MHD after coadministration with immediate-release oxcarbazepine Cimetidine, erythromycin and dextropropoxyphene had no effect on the pharmacokinetics of MHD after coadministration with immediate-release oxcarbazepine. Results with warfarin show no evidence of interaction with either single or repeated doses of immediate-release oxcarbazepine.
| Carbamazepine (400 to 2,000 mg) | 900 mg | nc1 | 40% decrease [CI: 17% decrease, 57% decrease] |
| Phenobarbital (100 to 150 mg) | 600 to 1,800 mg | 14% increase [CI: 2% increase, 24% increase] | 25% decrease [CI: 12% decrease, 51% decrease] |
| Phenytoin (250 to 500 mg) | 600 to 1,800 > 1,200 to 2,400 | nc1,2 up to 40% increase3 [CI: 12% increase, 60% increase] | 30% decrease [CI: 3% decrease, 48% decrease] |
| Valproic Acid (400 to 2,800 mg) | 600 to 1,800 | nc1 | 18% decrease [CI: 13% decrease, 40% decrease] |
| Lamotrigine (200 mg) | 1,200 | nc1 | nc1 |
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action The pharmacological activity of oxcarbazepine extended-release tablets are primarily exerted through the 10-monohydroxy metabolite (MHD) of oxcarbazepine [see Clinical Pharmacology ( 12.3 )] . The precise mechanism by which oxcarbazepine and MHD exert their antiseizure effect is unknown; however, in vitro electrophysiological studies indicate that they produce blockade of voltage-sensitive sodium channels, resulting in stabilization of hyperexcited neural membranes, inhibition of repetitive neuronal firing, and diminution of propagation of synaptic impulses. These actions are thought to be important in the prevention of seizure spread in the intact brain. In addition, increased potassium conductance and modulation of high-voltage activated calcium channels may contribute to the anticonvulsant effects of the drug. No significant interactions of oxcarbazepine or MHD with brain neurotransmitter or modulator receptor sites have been demonstrated.
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Oxcarbazepine and its active metabolite (MHD) exhibit anticonvulsant properties in animal seizure models. They protected rodents against electrically induced tonic extension seizures and, to a lesser degree, chemically induced clonic seizures, and abolished or reduced the frequency of chronically recurring focal seizures in Rhesus monkeys with aluminum implants. No development of tolerance (i.e., attenuation of anticonvulsive activity) was observed in the maximal electroshock test when mice and rats were treated daily for five days and four weeks, respectively, with oxcarbazepine or MHD.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Following oral administration, oxcarbazepine is absorbed and extensively metabolized to its pharmacologically active 10-monohydroxy metabolite (MHD), which is responsible for most antiepileptic activity. In clinical studies of oxcarbazepine extended-release tablets, the elimination half-life of oxcarbazepine was between 7 and 11 hours; the elimination half-life of MHD is between 9 and 11 hours. In a mass balance study in humans, only 2% of total radioactivity in plasma after administration of immediate-release oxcarbazepine was due to unchanged oxcarbazepine, with approximately 70% present as MHD, and the remainder attributable to minor metabolites. Absorption Oxcarbazepine extended-release tablets administered as a once daily dosage is not bioequivalent to the same total dosage of the immediate-release formulation given twice daily at steady state. Steady state plasma concentrations of MHD are reached within 5 days when oxcarbazepine extended-release tablets are given once daily. At steady state, when 1,200 mg oxcarbazepine extended-release tablets were given once daily, MHD C max occurred 7 hours post-dose. At steady state, oxcarbazepine extended-release tablets given once daily produced MHD exposures (AUC and C max ) about 19% lower and MHD minimum concentrations (C min ) about 16% lower than the immediate-release oxcarbazepine given twice daily when administered at the same 1,200 mg total daily dosage. When oxcarbazepine extended-release tablets were administered at an equivalent 600 mg single dose (4 x 150 mg tablets, 2 x 300 mg tablets, or 1 x 600 mg tablet), equivalent MHD exposures (AUC) were observed. Following a single dose of oxcarbazepine extended-release tablets (1 x 150 mg tablets, 1 x 300 mg tablets, or 1 x 600 mg tablet), the pharmacokinetics of MHD are not linear and show greater than dose proportional increase in AUC and less than proportional increase in C max : AUC increases 2.4-fold and C max increases 1.9-fold with a 2-fold increase in dose. Effect of Food : Single dose administration of 600 mg oxcarbazepine extended-release tablets following a high fat meal (800 to 1,000 calories) produced MHD exposure (AUC) equivalent to that produced under fasting conditions. Peak MHD concentration (C max ) was about 60% higher and occurred 2 hours earlier under fed conditions than under fasting conditions. The increase in C max , even without a significant change in the overall exposure, should be considered by the prescriber especially during the titration phase, when some adverse reactions are most likely to occur coincidentally with peak levels. Distribution The apparent volume of distribution of MHD is 49 L. Approximately 40% of MHD is bound to serum proteins, predominantly to albumin. Binding is independent of the serum concentration within the therapeutically relevant range. Oxcarbazepine and MHD do not bind to alpha-1-acid glycoprotein. Elimination Metabolism Oxcarbazepine is rapidly reduced by cytosolic enzymes in the liver to MHD, which is primarily responsible for the pharmacological effect of oxcarbazepine extended-release tablets. MHD is metabolized further by conjugation with glucuronic acid. Minor amounts (4% of the dose) are oxidized to the pharmacologically inactive 10,11-dihydroxy metabolite (DHD). Excretion Oxcarbazepine is cleared from the body mostly in the form of metabolites which are predominantly excreted by the kidneys. More than 95% of a dose of immediate-release oxcarbazepine appears in the urine, with less than 1% as unchanged oxcarbazepine. Fecal excretion accounts for less than 4% of an administered dose. Approximately 80% of the dose is excreted in the urine either as glucuronides of MHD (49%) or as unchanged MHD (27%); the inactive DHD accounts for approximately 3% and conjugates of MHD and oxcarbazepine account for 13% of the dose. The half-life of the parent was about two hours, while the half-life of MHD was about nine hours after the immediate-release formulation. A population pharmacokinetic model for oxcarbazepine extended-release tablets was developed in healthy normal adults and applied to pharmacokinetic data in patients with epilepsy. For oxcarbazepine, systemic parameters were scaled allometrically, suggesting that steady state oxcarbazepine exposure will vary inversely with weight. Specific Populations Geriatric Patients No studies with oxcarbazepine extended-release tablets in elderly patients have been completed [see Use in Specific Populations ( 8.5 )]. Following administration of single (300 mg) and multiple (600 mg/day) doses of immediate-release oxcarbazepine to elderly volunteers (60 to 82 years of age), the maximum plasma concentrations and AUC values of MHD were 30% to 60% higher than in younger volunteers (18 to 32 years of age). Comparisons of creatinine clearance in young and elderly volunteers indicate that the difference was due to age-related reductions in creatinine clearance. Pediatric Patients A pharmacokinetic study of oxcarbazepine was performed in 18 pediatric patients with epilepsy, which included patients 6 to less than 17 years of age, after multiple doses. The population pharmacokinetic model suggested that dosing of pediatric patients with oxcarbazepine can be determined based on body weight. Weight-normalized doses in pediatric patients should produce MHD exposures (AUC) comparable to that in typical adults, with oxcarbazepine exposures ~40% higher in children than in adults [see Use in Specific Populations ( 8.4 )] . The pharmacokinetics of oxcarbazepine in pediatric patients are similar when used as monotherapy or as adjunctive therapy for the treatment of partial-onset seizures. Pediatric Patients with Obesity A population PK analysis of immediate-release oxcarbazepine was conducted that included n=54 obese and non-obese pediatric patients 6 to <18 years of age to evaluate the potential impact of obesity on plasma oxcarbazepine exposures. Obesity was defined as BMI ≥95th percentile for age and sex based on CDC 2,000 growth chart recommendations. Simulated results from this analysis suggested that the target maintenance doses for oxcarbazepine, applied in pediatric patients ≥6 years of age, produced equivalent steady-state exposure of MHD between pediatric patients with and without obesity. This finding is consistent when using total body weight, or when using fat-free mass in the simulations. Dosage adjustment according to obesity status is not necessary. Male and Female Patients The effects of gender have not been studied for oxcarbazepine. No gender-related pharmacokinetic differences have been observed in children, adults, or the elderly with immediate-release oxcarbazepine. Racial or Ethnic Groups The effects of race have not been studied for oxcarbazepine. Patients with Renal or Hepatic Impairment The effects of renal or hepatic impairment have not been studied for oxcarbazepine [see Use in Specific Populations ( 8.6 , 8.7 )]. Based on investigations with immediate-release oxcarbazepine, there is a linear correlation between creatinine clearance and the renal clearance of MHD. When immediate-release oxcarbazepine is administered as a single 300 mg dose in renally-impaired patients (creatinine clearance <30 mL/min), the elimination half-life of MHD is prolonged to 19 hours, with a two-fold increase in AUC. Dosage adjustment is recommended in these patients [see Dosage and Administration ( 2.3 ) and Use in Special Populations ( 8.6 )]. The pharmacokinetics and metabolism of immediate-release oxcarbazepine and MHD were evaluated in healthy volunteers and hepatically impaired subjects after a single 900 mg oral dose. Mild-to-moderate hepatic impairment did not affect the pharmacokinetics of immediate-release oxcarbazepine and MHD. The pharmacokinetics of oxcarbazepine and MHD have not been evaluated in severe hepatic impairment, and therefore it is not recommended in these patients [see Use in Specific Populations (8.7)]. Pregnant Women Due to physiological changes during pregnancy, MHD plasma levels may gradually decrease throughout pregnancy [see Use in Specific Populations ( 8.1 )]. Drug Interaction Studies In Vitro: Oxcarbazepine can inhibit CYP2C19 and induce CYP3A4/5 with potentially important effects on plasma concentrations of other drugs. In addition, several AEDs that are cytochrome P450 inducers can decrease plasma concentrations of oxcarbazepine and MHD. Oxcarbazepine was evaluated in human liver microsomes to determine its capacity to inhibit the major cytochrome P450 enzymes responsible for the metabolism of other drugs. Results demonstrate that oxcarbazepine and its pharmacologically active 10-monohydroxy metabolite (MHD) have little or no capacity to function as inhibitors for most of the human cytochrome P450 enzymes evaluated (CYP1A2, CYP2A6, CYP2C9, CYP2D6, CYP2E1, CYP4A9 and CYP4A11) with the exception of CYP2C19 and CYP3A4/5. Although inhibition of CYP3A4/5 by oxcarbazepine and MHD did occur at high concentrations, it is not likely to be of clinical significance. The inhibition of CYP2C19 by oxcarbazepine and MHD, is clinically relevant. In vitro , the UDP-glucuronyl transferase level was increased, indicating induction of this enzyme. Increases of 22% with MHD and 47% with oxcarbazepine were observed. As MHD, the predominant plasma substrate, is only a weak inducer of UDP-glucuronyl transferase, it is unlikely to have an effect on drugs that are mainly eliminated by conjugation through UDP-glucuronyl transferase (e.g., valproic acid, lamotrigine). In addition, oxcarbazepine and MHD induce a subgroup of the cytochrome P450 3A family (CYP3A4 and CYP3A5) responsible for the metabolism of dihydropyridine calcium antagonists, oral contraceptives and cyclosporine resulting in a lower plasma concentration of these drugs. Several AEDs that are cytochrome P450 inducers can decrease plasma concentrations of oxcarbazepine and MHD. No autoinduction has been observed with immediate-release oxcarbazepine. As binding of MHD to plasma proteins is low (40%), clinically significant interactions with other drugs through competition for protein binding sites are unlikely. In Vivo: Other Antiepileptic Drugs Potential interactions between immediate-release oxcarbazepine and other AEDs were assessed in clinical studies. The effect of these interactions on mean AUCs and C min are summarized in Table 5 [see Drug Interactions (7.1, 7.2)]. Table 5: AED Drug Interactions with Immediate-Release (IR) Oxcarbazepine AED Coadministered (daily dosage) IR-Oxcarbazepine (daily dosage) Influence of IR- Oxcarbazepine on AED Concentration Mean Change [90% Confidence Interval] Influence of AED on MHD Concentration (Mean Change, 90% Confidence Interval) Carbamazepine (400 to 2,000 mg) 900 mg nc 1 40% decrease [CI: 17% decrease, 57% decrease] Phenobarbital (100 to 150 mg) 600 to 1,800 mg 14% increase [CI: 2% increase, 24% increase] 25% decrease [CI: 12% decrease, 51% decrease] Phenytoin (250 to 500 mg) 600 to 1,800 > 1,200 to 2,400 nc 1,2 up to 40% increase 3 [CI: 12% increase, 60% increase] 30% decrease [CI: 3% decrease, 48% decrease] Valproic Acid (400 to 2,800 mg) 600 to 1,800 nc 1 18% decrease [CI: 13% decrease, 40% decrease] Lamotrigine (200 mg) 1,200 nc 1 nc 1 1 nc denotes a mean change of less than 10% 2 Pediatrics 3 Mean increase in adults at high doses of immediate-release oxcarbazepine Hormonal Contraceptives Coadministration of immediate-release oxcarbazepine with an oral contraceptive has been shown to influence the plasma concentrations of two components of hormonal contraceptives, ethinylestradiol (EE) and levonorgestrel (LNG). The mean AUC values of EE were decreased by 48% [90% CI: 22 to 65] in one study and 52% [90% CI: 38 to 52] in another study. The mean AUC values of LNG were decreased by 32% [90% CI: 20 to 45] in one study and 52% [90% CI: 42 to 52] in another study. Other Drug Interactions Calcium Antagonists: After repeated coadministration of immediate-release oxcarbazepine, the AUC of felodipine was lowered by 28% [90% CI: 20 to 33]. Verapamil produced a decrease of 20% [90% CI: 18 to 27] of the plasma levels of MHD after coadministration with immediate-release oxcarbazepine Cimetidine, erythromycin and dextropropoxyphene had no effect on the pharmacokinetics of MHD after coadministration with immediate-release oxcarbazepine. Results with warfarin show no evidence of interaction with either single or repeated doses of immediate-release oxcarbazepine.
| Carbamazepine (400 to 2,000 mg) | 900 mg | nc1 | 40% decrease [CI: 17% decrease, 57% decrease] |
| Phenobarbital (100 to 150 mg) | 600 to 1,800 mg | 14% increase [CI: 2% increase, 24% increase] | 25% decrease [CI: 12% decrease, 51% decrease] |
| Phenytoin (250 to 500 mg) | 600 to 1,800 > 1,200 to 2,400 | nc1,2 up to 40% increase3 [CI: 12% increase, 60% increase] | 30% decrease [CI: 3% decrease, 48% decrease] |
| Valproic Acid (400 to 2,800 mg) | 600 to 1,800 | nc1 | 18% decrease [CI: 13% decrease, 40% decrease] |
| Lamotrigine (200 mg) | 1,200 | nc1 | nc1 |
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS Oxcarbazepine extended-release tablets are contraindicated in patients with a known hypersensitivity to oxcarbazepine, to any of the components of oxcarbazepine extended-release tablets, or to eslicarbazepine acetate. Reactions have included anaphylaxis and angioedema [see Warnings and Precautions ( 5.2 , 5.3 )]. Known hypersensitivity to oxcarbazepine, any of the components of oxcarbazepine extended-release tablets, or to eslicarbazepine acetate. ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION Oxcarbazepine extended-release tablet is an antiepileptic drug (AED). Oxcarbazepine extended-release tablets contain oxcarbazepine, USP for once-a-day oral administration. Oxcarbazepine, USP is 10,11-Dihydro-10-oxo- 5H -dibenz[ b,f ]azepine-5-carboxamide, and its structural formula is Oxcarbazepine is light orange to creamish white or off-white powder. Oxcarbazepine is soluble in acetic acid, sparingly soluble in chloroform and practically insoluble in water. The molecular formula is C 15 H 12 N 2 O 2 and its molecular weight is 252.27 g/mol. Oxcarbazepine extended-release tablets contain the following inactive ingredients: colloidal silicon dioxide, ferric oxide red (300 mg, 600 mg tablets only), ferric oxide yellow (150 mg, 300 mg tablets only), hydroxypropyl methyl cellulose, iron oxide black (300 mg tablet only), magnesium stearate, polyethylene glycol, polyvinyl alcohol, sorbitol, talc, titanium dioxide (300 mg, 600 mg tablets only).
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION Adult Patients: The recommended initial dosage is 600 mg once per day. Increase the dosage in weekly increments of 600 mg once per day, based on clinical response and tolerability, to a recommended maintenance dosage of 1,200 mg to 2,400 mg once per day. ( 2.2 ) In adult patients with a creatinine clearance <30 mL/min, initiate at one-half the usual starting dosage and increase slowly. ( 2.3 ) Pediatric Patients: The recommended dosage is based on body weight and is administered orally once per day. Increase the dosage in weekly intervals based on clinical response and tolerability, to the recommended dosage. ( 2.2 ) Geriatric Patients: Start at lower dosage (300 mg or 450 mg/day) and increase slowly. ( 2.4 ) In conversion of oxcarbazepine immediate-release to oxcarbazepine extended-release tablets, higher dosages of oxcarbazepine extended-release tablets may be necessary. ( 2.7 , 12.3 ) 2.1 Important Administration Instructions Administer oxcarbazepine extended-release tablets as a single daily dose taken on an empty stomach (at least 1 hour before or at least 2 hours after meals) [see Clinical Pharmacology ( 12.3 )] . If oxcarbazepine extended-release tablets are taken with food, adverse reactions are more likely to occur because of increased peak levels [see Clinical Pharmacology ( 12.3 )]. Swallow oxcarbazepine extended-release tablets whole. Do not cut, crush, or chew the tablets. For ease of swallowing in pediatric patients or patients with difficulty swallowing, achieve daily dosages with multiples of appropriate lower strength tablets (e.g., 150 mg tablets). 2.2 General Dosing Recommendations Monotherapy or Adjunctive Therapy Adult Patients Initiate treatment at a dosage of 600 mg/day given orally once daily for one week. Subsequent dosage increases can be made at weekly intervals in 600 mg/day increments to achieve the recommended daily dosage. The recommended daily dosage of oxcarbazepine extended-release tablets is 1,200 mg to 2,400 mg/day, given once daily. The dosage of 2,400 mg/day showed slightly greater efficacy than 1,200 mg/day, but was associated with an increase in adverse reactions [see Adverse Reactions ( 6.1 ) and Clinical Studies ( 14.1 )] . Dosage adjustment is recommended with concomitant use of strong CYP3A4 enzyme inducers or UGT inducers, which include certain antiepileptic drugs (AEDs) [see Drug Interactions ( 7.1 , 7.2 )]. Pediatric Patients (6 to Less than 17 Years of Age) In pediatric patients 6 to less than 17 years of age, initiate treatment at a daily dosage of 8 mg/kg to 10 mg/kg orally once daily, not to exceed 600 mg per day in the first week. Subsequent dosage increases can be made at weekly intervals in 8 mg/kg to 10 mg/kg increments once daily, not to exceed 600 mg, to achieve the target daily dosage. The target maintenance dosage, achieved over two to three weeks, is displayed in Table 1. Table 1: Target Daily Dosage in Pediatric Patients (6 to Less Than 17 Years of Age) Weight Target Daily Dosage 20 kg to 29 kg 900 mg/day 29.1 kg to 39 kg 1,200 mg/day Greater than 39 kg 1,800 mg/day Dosage adjustment is recommended with concomitant use of strong CYP3A4 enzyme inducers or UGT inducers, which include certain antiepileptic drugs (AEDs) [see Drug Interactions ( 7.1 , 7.2 )]. 2.3 Dosage Modifications in Adult Patients with Renal Impairment In adult patients with severe renal impairment (creatinine clearance less than 30 mL/minute), initiate oxcarbazepine extended-release tablets at one-half the usual starting dosage (300 mg/day). Subsequent dosage increases can be made at weekly intervals in increments of 300 mg to 450 mg/day to achieve the desired clinical response [see Use in Specific Populations ( 8.6 )]. 2.4 Dosage Modifications in Geriatric Patients In geriatric patients, consider starting at a lower dosage (300 mg or 450 mg/day). Subsequent dosage increases can be made at weekly intervals in increments of 300 mg to 450 mg/day to achieve the desired clinical effect [see Use in Specific Populations ( 8.5 )]. 2.5 Dosage Modification with Concomitant Use of Strong CYP3A4 Enzyme Inducers or UGT Enzyme Inducers Strong CYP3A4 inducers, including enzyme-inducing antiepileptic drugs such as carbamazepine, phenobarbital, and phenytoin, and UGT inducers (e.g., rifampin) decrease exposure to 10-monohydroxy derivative (MHD), the active metabolite [see Drug Interactions ( 7.2 ) and Clinical Pharmacology ( 12.3 )] . Dosage adjustment of oxcarbazepine extended-release tablets may be required after initiation, dosage modification, or discontinuation of such inducers. Dosage increases of oxcarbazepine extended-release tablets may be necessary with concomitant use. Consider initiating at 900 mg once daily for adults and 12 to 15 mg/kg orally once daily (not to exceed 900 mg per day in the first week) in pediatric patients. 2.6 Withdrawal of AEDs As with most antiepileptic drugs, oxcarbazepine extended-release tablets should be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus [see Warnings and Precautions ( 5.6 )]. 2.7 Conversion from Immediate-Release Oxcarbazepine to Oxcarbazepine Extended-Release Tablets In conversion of oxcarbazepine immediate-release to oxcarbazepine extended-release tablets, higher dosages of oxcarbazepine extended-release tablets may be necessary [see Clinical Pharmacology ( 12.3 )].
| Weight | Target Daily Dosage |
| 20 kg to 29 kg | 900 mg/day |
| 29.1 kg to 39 kg | 1,200 mg/day |
| Greater than 39 kg | 1,800 mg/day |
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Extended-release tablets : 150 mg: Yellow, oval, biconvex film-coated tablet. Engraved “OX150” on one side, “APO” on the other side. 300 mg: Brown, oval, biconvex film-coated tablet. Engraved “OX300” on one side, “APO” on the other side. 600 mg: Brownish red, oval, biconvex film-coated tablet. Engraved “OX600” on one side, “APO” on the other side. Extended-release tablets: 150 mg, 300 mg and 600 mg ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE Oxcarbazepine extended-release tablets are indicated for the treatment of partial-onset seizures in patients 6 years of age and older. Oxcarbazepine extended-release tablets are indicated for the treatment of partial-onset seizures in patients 6 years of age and older. ( 1 )
Spl product data elements
Usually a list of ingredients in a drug product.OXCARBAZEPINE OXCARBAZEPINE Oxcarbazepine Oxcarbazepine Sorbitol Silicon Dioxide Magnesium Stearate Hypromellose 2208 (100 Mpa.S) Talc Polyethylene Glycol 8000 Ferric Oxide Yellow Polyvinyl Alcohol OX150;APO OXCARBAZEPINE OXCARBAZEPINE Oxcarbazepine Oxcarbazepine Sorbitol Silicon Dioxide Magnesium Stearate Hypromellose 2208 (100 Mpa.S) Talc Polyethylene Glycol 8000 Ferric Oxide Yellow Ferric Oxide Red Titanium Dioxide Ferrosoferric Oxide Polyvinyl Alcohol OX300;APO OXCARBAZEPINE OXCARBAZEPINE Oxcarbazepine Oxcarbazepine Sorbitol Silicon Dioxide Magnesium Stearate Hypromellose 2208 (100 Mpa.S) Talc Polyethylene Glycol 8000 Ferric Oxide Red Titanium Dioxide Polyvinyl Alcohol OX600;APO Structure-1 LBL150mg100s LBL300mg100s LBL600mg100s
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis In two-year carcinogenicity studies, oxcarbazepine was administered in the diet at doses of up to 100 mg/kg/day to mice and by gavage at doses of up to 250 mg/kg/day to rats, and the pharmacologically active 10-hydroxy metabolite (MHD) was administered orally at doses of up to 600 mg/kg/day to rats. In mice, a dose-related increase in the incidence of hepatocellular adenomas was observed at oxcarbazepine doses ≥ 70 mg/kg/day or approximately 0.1 times the maximum recommended human dose (MRHD) on a mg/m 2 basis. In rats, the incidence of hepatocellular carcinomas was increased in females treated with oxcarbazepine at doses ≥25 mg/kg/day (0.1 times the MRHD on a mg/m 2 basis), and incidences of hepatocellular adenomas and/or carcinomas were increased in males and females treated with MHD at doses of 600 mg/kg/day (2.4 times the MRHD on a mg/m 2 basis) and ≥ 250 mg/kg/day (equivalent to the MRHD on a mg/m 2 basis), respectively. There was an increase in the incidence of benign testicular interstitial cell tumors in rats at 250 mg oxcarbazepine/kg/day and at ≥ 250 mg MHD/kg/day, and an increase in the incidence of granular cell tumors in the cervix and vagina in rats at 600 mg MHD/kg/day. Mutagenesis Oxcarbazepine increased mutation frequencies in the Ames test in vitro in the absence of metabolic activation in one of five bacterial strains. Both oxcarbazepine and MHD produced increases in chromosomal aberrations and polyploidy in the Chinese hamster ovary assay in vitro in the absence of metabolic activation. MHD was negative in the Ames test, and no mutagenic or clastogenic activity was found with either oxcarbazepine or MHD in V79 Chinese hamster cells in vitro. Oxcarbazepine and MHD were both negative for clastogenic or aneugenic effects (micronucleus formation) in an in vivo rat bone marrow assay. Impairment of Fertility In a fertility study in which rats were administered MHD (50, 150, or 450 mg/kg) orally prior to and during mating and early gestation, estrous cyclicity was disrupted and numbers of corpora lutea, implantations, and live embryos were reduced in females receiving the highest dose (approximately two times the MRHD on a mg/m 2 basis).
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis In two-year carcinogenicity studies, oxcarbazepine was administered in the diet at doses of up to 100 mg/kg/day to mice and by gavage at doses of up to 250 mg/kg/day to rats, and the pharmacologically active 10-hydroxy metabolite (MHD) was administered orally at doses of up to 600 mg/kg/day to rats. In mice, a dose-related increase in the incidence of hepatocellular adenomas was observed at oxcarbazepine doses ≥ 70 mg/kg/day or approximately 0.1 times the maximum recommended human dose (MRHD) on a mg/m 2 basis. In rats, the incidence of hepatocellular carcinomas was increased in females treated with oxcarbazepine at doses ≥25 mg/kg/day (0.1 times the MRHD on a mg/m 2 basis), and incidences of hepatocellular adenomas and/or carcinomas were increased in males and females treated with MHD at doses of 600 mg/kg/day (2.4 times the MRHD on a mg/m 2 basis) and ≥ 250 mg/kg/day (equivalent to the MRHD on a mg/m 2 basis), respectively. There was an increase in the incidence of benign testicular interstitial cell tumors in rats at 250 mg oxcarbazepine/kg/day and at ≥ 250 mg MHD/kg/day, and an increase in the incidence of granular cell tumors in the cervix and vagina in rats at 600 mg MHD/kg/day. Mutagenesis Oxcarbazepine increased mutation frequencies in the Ames test in vitro in the absence of metabolic activation in one of five bacterial strains. Both oxcarbazepine and MHD produced increases in chromosomal aberrations and polyploidy in the Chinese hamster ovary assay in vitro in the absence of metabolic activation. MHD was negative in the Ames test, and no mutagenic or clastogenic activity was found with either oxcarbazepine or MHD in V79 Chinese hamster cells in vitro. Oxcarbazepine and MHD were both negative for clastogenic or aneugenic effects (micronucleus formation) in an in vivo rat bone marrow assay. Impairment of Fertility In a fertility study in which rats were administered MHD (50, 150, or 450 mg/kg) orally prior to and during mating and early gestation, estrous cyclicity was disrupted and numbers of corpora lutea, implantations, and live embryos were reduced in females receiving the highest dose (approximately two times the MRHD on a mg/m 2 basis).
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PRINCIPAL DISPLAY PANEL - 150 mg PRINCIPAL DISPLAY PANEL - 150 mg BOTTLE LABEL APOTEX CORP. NDC 60505-4128-7 OXCARBAZEPINE EXTENDED-RELEASE TABLETS 150 mg Rx 100 Tablets
PRINCIPAL DISPLAY PANEL - 300 mg PRINCIPAL DISPLAY PANEL - 300 mg BOTTLE LABEL APOTEX CORP. NDC 60505-4129-7 OXCARBAZEPINE EXTENDED-RELEASE TABLETS 300 mg Rx 100 Tablets
PRINCIPAL DISPLAY PANEL - 600 mg PRINCIPAL DISPLAY PANEL - 600 mg BOTTLE LABEL APOTEX CORP. NDC 60505-4130-7 OXCARBAZEPINE EXTENDED-RELEASE TABLETS 600 mg Rx 100 Tablets
OXCARBAZEPINE: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Advise the patient to read the FDA-Approved patient labeling (Medication Guide). Administration Information Advise patients to take the tablet whole. Do not cut, chew, or crush the tablet. Advise patients to take oxcarbazepine extended-release tablets on an empty stomach. This means they should take oxcarbazepine extended-release tablets at least one hour before food or at least two hours after food [see Dosage and Administration (2.1) and Clinical Pharmacology (12.3)]. Hyponatremia Advise patients that oxcarbazepine extended-release tablets may reduce serum sodium concentrations especially if they are taking other medications that can lower sodium. Advise patients to report symptoms of low sodium like nausea, tiredness, lack of energy, confusion, and more frequent or more severe seizures [see Warnings and Precautions (5.1)]. Anaphylactic Reactions and Angioedema Anaphylactic reactions and angioedema may occur during treatment with oxcarbazepine extended-release tablets. Advise patients to immediately report signs and symptoms suggesting angioedema (swelling of the face, eyes, lips, tongue, or difficulty in swallowing or breathing) and to stop taking the drug until they have consulted with their physician [see Warnings and Precautions (5.2)]. Cross Hypersensitivity Reaction to Carbamazepine Inform patients who have exhibited hypersensitivity reactions to carbamazepine that approximately 25% to 30% of these patients may also experience hypersensitivity reactions with oxcarbazepine extended-release tablets. If patients experience a hypersensitivity reaction while taking oxcarbazepine extended-release tablets, advise them to consult with their physician immediately [see Warnings and Precautions (5.3)] . Serious Dermatological Reactions Advise patients that serious skin reactions have been reported in association with immediate-release oxcarbazepine. If patients experience a skin reaction while taking oxcarbazepine extended-release tablets, advise patients to consult with their physician immediately [see Warnings and Precautions (5.4)]. Suicidal Behavior and Ideation Counsel patients, their caregivers, and families that AEDs, including oxcarbazepine extended-release tablets, may increase the risk of suicidal thoughts and behavior and that they need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Advise them to immediately report behaviors of concern to healthcare providers [see Warnings and Precautions (5.5)]. DRESS/Multi-Organ Hypersensitivity Instruct patients that a fever associated with signs of other organ system involvement (e.g., rash, lymphadenopathy, hepatic dysfunction, etc.) occurring during treatment with oxcarbazepine extended-release tablets may be drug-related, and advise them to consult their physician immediately [see Warnings and Precautions (5.7)]. Hematologic Reactions Advise patients that there have been rare reports of blood disorders reported in patients treated with immediate-release oxcarbazepine. Instruct patients to immediately consult with their physician if they experience symptoms suggestive of blood disorders during treatment with oxcarbazepine extended-release tablets [see Warnings and Precautions (5.8)]. Drug Interactions Warn female patients of childbearing age that the concurrent use of oxcarbazepine extended-release tablets with hormonal contraceptives may render this method of contraception less effective [see Drug Interactions (7.3) and Use in Specific Populations (8.1)]. Additional non-hormonal forms of contraception are recommended when using oxcarbazepine extended-release tablets. Pregnancy Registry Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during oxcarbazepine extended-release tablets therapy. Encourage patients to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant. This registry is collecting information about the safety of antiepileptic drugs during pregnancy [see Use in Specific Populations (8.1)]. Dispense with Medication Guide available at https://www.apotex.com/products/us/mg.asp APOTEX INC. OXCARBAZEPINE EXTENDED-RELEASE TABLETS 150 mg, 300 mg and 600 mg Manufactured by Manufactured for Apotex Inc. Toronto, Ontario Canada M9L 1T9 Apotex Corp. Weston, Florida USA 33326 Revision: 4
| Apotex Inc. Toronto, Ontario Canada M9L 1T9 | Apotex Corp. Weston, Florida USA 33326 |
Spl medguide
Information about the patient medication guide that accompanies the drug product. Certain drugs must be dispensed with an accompanying medication guide. This field may contain information about when to consult the medication guide and the contents of the medication guide.MEDICATION GUIDE Oxcarbazepine (ox’’ kar baz’ e peen) extended-release tablets, for oral use Medication Guide available at https://www.apotex.com/products/us/mg.asp What is the most important information I should know about oxcarbazepine extended-release tablets? Do not stop taking oxcarbazepine extended-release tablets without first talking to your healthcare provider. Stopping oxcarbazepine extended-release tablets suddenly can cause serious problems. Oxcarbazepine extended-release tablets can cause serious side effects, including: 1. Oxcarbazepine extended-release tablets may cause the level of sodium in your blood to be low. Symptoms of low blood sodium include: nausea tiredness, lack of energy headache confusion more frequent or more severe seizures Similar symptoms that are not related to low sodium may occur from taking oxcarbazepine extended-release tablets. You should tell your healthcare provider if you have any of these side effects and if they bother you or they do not go away. Some other medicines can also cause low sodium in your blood. Be sure to tell your healthcare provider about all the other medicines that you are taking. Your healthcare provider may do blood tests to check your sodium levels during your treatment with oxcarbazepine extended-release tablets . 2. Oxcarbazepine extended-release tablets may also cause allergic reactions or serious problems which may affect organs and other parts of your body like the liver or blood cells. You may or may not have a rash with these types of reactions. Call your healthcare provider right away if you have any of the following: swelling of your face, eyes, lips, or tongue trouble swallowing or breathing a skin rash hives fever, swollen glands, or sore throat that does not go away or comes and goes painful sores in the mouth or around your eyes yellowing of your skin or eyes unusual bruising or bleeding severe fatigue or weakness severe muscle pain frequent infections that do not go away Many people who are allergic to carbamazepine are also allergic to oxcarbazepine extended-release tablets. Tell your healthcare provider if you are allergic to carbamazepine. 3. Like other antiepileptic drugs, oxcarbazepine extended-release tablets may cause suicidal thoughts or actions in a very small number of people, about 1 in 500. Call your healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you: thoughts about suicide or dying attempts to commit suicide new or worse depression new or worse anxiety feeling agitated or restless panic attacks trouble sleeping (insomnia) new or worse irritability acting aggressive, being angry, or violent acting on dangerous impulses an extreme increase in activity and talking (mania) other unusual changes in behavior or mood How can I watch for early symptoms of suicidal thoughts and actions? Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. Keep all follow-up visits with your healthcare provider as scheduled. Call your healthcare provider between visits as needed, especially if you are worried about symptoms. Do not stop taking oxcarbazepine extended-release tablets without first talking to a healthcare provider. Stopping oxcarbazepine extended-release tablets suddenly can cause serious problems. Stopping a seizure medicine suddenly in a patient who has epilepsy may cause seizures that will not stop (status epilepticus). Suicidal thoughts or actions may be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes. What is oxcarbazepine extended-release tablets? Oxcarbazepine extended-release tablets are a prescription medicine used to treat partial onset seizures in adults and children 6 years of age and older. Oxcarbazepine extended-release tablets are not for use in children under 6 years of age. It is not known if oxcarbazepine extended-release tablets are safe and effective in children under 6 years of age. Who should not take oxcarbazepine extended-release tablets? Do not take oxcarbazepine extended-release tablets if you are allergic to oxcarbazepine or any of the other ingredients in oxcarbazepine extended-release tablets, or to eslicarbazepine acetate. See the end of this Medication Guide for a complete list of ingredients in oxcarbazepine extended-release tablets. What should I tell my healthcare provider before taking oxcarbazepine extended-release tablets? Before taking oxcarbazepine extended-release tablets, tell your healthcare provider about all your medical conditions, including if you: have or have had suicidal thoughts or actions, depression or mood problems. have liver problems. have kidney problems. are allergic to carbamazepine. Many people who are allergic to carbamazepine are also allergic to oxcarbazepine extended-release tablets. use birth control medicine. Oxcarbazepine extended-release tablets may cause your birth control medicine to be less effective. Talk to your healthcare provider about the best birth control method to use. are pregnant or plan to become pregnant. Oxcarbazepine extended-release tablets may harm your unborn baby. Tell your healthcare provider right away if you become pregnant while taking oxcarbazepine extended-release tablets. You and your healthcare provider will decide if you should take oxcarbazepine extended-release tablets while you are pregnant. If you become pregnant while taking oxcarbazepine extended-release tablets, talk to your healthcare provider about registering with the North American Antiepileptic Drug (NAAED) Pregnancy Registry. The purpose of this registry is to collect information about the safety of antiepileptic medicine during pregnancy. You can enroll in this registry by calling 1-888-233-2334. are breastfeeding or plan to breastfeed. Oxcarbazepine extended-release tablets passes into breast milk. Talk with your healthcare provider about the best way to feed your baby if you take oxcarbazepine extended-release tablets. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Taking oxcarbazepine extended-release tablets with certain other medicines may cause side effects or affect how well they work. Do not start or stop other medicines without talking to your healthcare provider. Especially tell your healthcare provider if you take : carbamazepine, phenobarbital, phenytoin, or birth control medicine. Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine. How should I take oxcarbazepine extended-release tablets? Do not stop taking oxcarbazepine extended-release tablets without talking to your healthcare provider. Stopping oxcarbazepine extended-release tablets suddenly can cause serious problems, including seizures that will not stop (status epilepticus). Take oxcarbazepine extended-release tablets exactly as prescribed. Your healthcare provider may change your dose. Your healthcare provider will tell you how much oxcarbazepine extended-release tablets to take. Take oxcarbazepine extended-release tablets 1 time each day. Take oxcarbazepine extended-release tablets on an empty stomach. This means you should take oxcarbazepine extended-release tablets at least 1 hour before or at least 2 hours after a meal. Take oxcarbazepine extended-release tablets whole with water or other liquid. Do not cut, crush, or chew the tablets before swallowing. If you take too much oxcarbazepine extended-release tablets call your healthcare provider right away. What are the possible side effects of oxcarbazepine extended-release tablets? See “What is the most important information I should know about oxcarbazepine extended-release tablets?” Oxcarbazepine extended-release tablets may cause other serious side effects including: seizures that can happen more often or become worse, especially in children. The most common side effects of oxcarbazepine extended-release tablets include: dizziness sleepiness headache balance problems tremors vomiting double vision weakness or lack of energy (asthenia) These are not all the possible side effects of oxcarbazepine extended-release tablets. For more information, ask your healthcare provider or pharmacist. Tell your healthcare provider if you have any side effect that bothers you or does not go away. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store oxcarbazepine extended-release tablets? Store oxcarbazepine extended-release tablets at room temperature between 68°F to 77°F (20°C and 25°C). Keep oxcarbazepine extended-release tablets in a tightly closed container and out of the light. Keep oxcarbazepine extended-release tablets dry. Keep oxcarbazepine extended-release tablets and all medicines out of the reach of children. General Information about the safe and effective use of oxcarbazepine extended-release tablets. Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use oxcarbazepine extended-release tablets for a condition for which it was not prescribed. Do not give oxcarbazepine extended-release tablets to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about oxcarbazepine extended-release tablets that is written for health professionals. What are the ingredients in oxcarbazepine extended-release tablets? Active ingredient: oxcarbazepine Inactive ingredients: 150 mg tablets: colloidal silicon dioxide, ferric oxide yellow, hydroxypropyl methyl cellulose, magnesium stearate, polyethylene glycol, polyvinyl alcohol, sorbitol, talc. 300 mg tablets: colloidal silicon dioxide, ferric oxide red, ferric oxide yellow, hydroxypropyl methyl cellulose, black iron oxide, magnesium stearate, polyethylene glycol, polyvinyl alcohol, sorbitol, talc, titanium dioxide. 600 mg tablets: colloidal silicon dioxide, ferric oxide red, hydroxypropyl methyl cellulose, magnesium stearate, polyethylene glycol, polyvinyl alcohol, sorbitol, talc, titanium dioxide. For more information, go to www.apotex.com or call 1-800-706-5575. This Medication Guide has been approved by the U.S. Food and Drug Administration. APOTEX INC. OXCARBAZEPINE EXTENDED-RELEASE TABLETS 150 mg, 300 mg and 600 mg Manufactured by Manufactured for Apotex Inc. Toronto, Ontario Canada M9L 1T9 Apotex Corp. Weston, Florida USA 33326 Revised: September 2024 Revision: 4
| Apotex Inc. Toronto, Ontario Canada M9L 1T9 | Apotex Corp. Weston, Florida USA 33326 |
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES Oxcarbazepine extended-release tablets has been evaluated as adjunctive therapy for partial-onset seizures in adults. The use of oxcarbazepine extended-release tablets for the treatment of partial-onset seizures in pediatric patients 6 years of age and older is based on adequate and well-controlled studies of oxcarbazepine extended-release tablets in adults, along with clinical trials of immediate-release oxcarbazepine in pediatric patients, and on pharmacokinetic evaluations of the use of oxcarbazepine extended-release tablets in pediatric patients. 14.1 Oxcarbazepine Extended-Release Tablets Primary Trial A multicenter, randomized, double-blind, placebo-controlled, three-arm, parallel-group study (Study 1) in male and female adults with refractory partial-onset seizures (18 to 65 years of age, inclusive) was performed to examine the safety and efficacy of oxcarbazepine extended-release tablets. Patients had at least three partial-onset seizures per 28 days during an 8-week Baseline Period. Subjects were receiving treatment with at least one to three antiepileptic drugs and were on stable treatment for a minimum of 4 weeks. Subjects with a diagnosis other than partial-onset seizures were excluded. The study included an 8 week Baseline Period, followed by a Treatment Period, which included a 4 week Titration Phase followed by a 12 week Maintenance Phase. The primary endpoint of the study was median percentage change from baseline in seizure frequency per 28 days during the treatment period relative to the baseline period. The criterion for statistical significance was p<0.05. A total of 366 patients were enrolled at 88 sites in North America and Eastern Europe. Subjects were randomized to one of three treatment groups and took oxcarbazepine extended-release tablets (1,200 or 2,400 mg/day) or placebo. Table 6 presents the primary efficacy results by treatment group. Table 6: Primary Efficacy Results in Study 1: Percent Change from Baseline in Partial-Onset Seizure Frequency in the 16-week Treatment Period Median seizure frequency during 8-week baseline period (per 28 days) Median seizure frequency during 16-week treatment period (per 28 days) Median percent change in seizure frequency Seizure frequency percent change effect size P value vs placebo* Placebo (N=121) 7.0 5.0 -28.7 % Oxcarbazepine extended-release tablets 1,200mg/day (N=122) 6.0 4.3 -38.2 % 9.5% 0.078 Oxcarbazepine extended-release tablets 2,400mg/day (N=123) 6.0 3.7 -42.9 % 14.2% 0.003 *Wilcoxon rank-sum test of the median percentage change in partial-onset seizure frequency per 28 days during the 16-week Treatment Phase (Titration + Maintenance Periods) relative to the 8-week Baseline Phase. Although the 1,200 mg/day-placebo contrast did not reach statistical significance, concentration-response analyses reveal that the 1,200 mg/day dosage is an effective dosage. 14.2 Immediate-Release Oxcarbazepine Adjunctive Therapy Trials The effectiveness of immediate-release oxcarbazepine as an adjunctive therapy for partial-onset seizures in adults was demonstrated at dosages of 600 mg/day, 1,200 mg/day, and 2,400 mg/day (divided twice daily) in a randomized, double-blind, placebo-controlled trial. All dosages resulted in a statistically significant reduction in seizure frequency when compared to placebo (p<0.05). The effectiveness of immediate-release oxcarbazepine in dosages of 30 to 46 mg/kg/day, depending on baseline weight, as an adjunctive therapy for partial-onset seizures in pediatric patients, including patients 6 to less than 17 years of age, was studied in a randomized, double-blind, placebo-controlled trial. Oxcarbazepine in the single weight-based dosage group resulted in a statistically significant reduction in seizure frequency when compared to placebo (p<0.05).
| Placebo (N=121) | 7.0 | 5.0 | -28.7 % | ||
| Oxcarbazepine extended-release tablets 1,200mg/day (N=122) | -38.2 % | ||||
| Oxcarbazepine extended-release tablets 2,400mg/day (N=123) |
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use Following administration of single (300 mg) and multiple (600 mg/day) doses of immediate-release oxcarbazepine to elderly volunteers (60 to 82 years of age), the maximum plasma concentrations and AUC values of MHD were 30% to 60% higher than in younger volunteers (18 to 32 years of age). Comparisons of creatinine clearance in young and elderly volunteers indicate that the difference was due to age-related reductions in creatinine clearance. Consider starting at a lower dosage and lower titration [see Dosage and Administration ( 2.4 )] . Close monitoring of sodium levels is required in elderly patients at risk for hyponatremia [see Warnings and Precautions ( 5.1 )] .
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use The safety and effectiveness of oxcarbazepine extended-release tablets in pediatric patients 6 years of age and older for the treatment of partial-onset seizures is supported by: 1) An adequate and well-controlled safety and efficacy study of oxcarbazepine extended-release tablets in adults that included pharmacokinetic sampling [see Clinical Studies ( 14.1 )] , 2) A pharmacokinetic study of oxcarbazepine extended-release tablets in pediatric patients, which included patients 6 to less than 17 years of age [see Clinical Pharmacology ( 12.3 )] , 3) Safety and efficacy studies with the immediate-release formulation in adults and pediatric patients [see Clinical Studies ( 14.2 ) and Adverse Reactions ( 6.1 )] . Oxcarbazepine extended-release tablets is not approved for pediatric patients less than 6 years of age because the size of the tablets are inappropriate for younger children.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Pregnancy Exposure Registry There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to AEDs, such as oxcarbazepine extended-release tablets, during pregnancy. Encourage women who are taking oxcarbazepine extended-release tablets during pregnancy to enroll in the North American Antiepileptic Drug (NAAED Pregnancy Registry) by calling 1-888-233-2334 or visiting http://www.aedpregnancyregistry.org/ . Risk Summary There are no adequate data on the developmental risks associated with the use of oxcarbazepine extended-release tablets in pregnant women; however, oxcarbazepine extended-release tablets are closely related structurally to carbamazepine, which is considered to be teratogenic in humans. Data on a limited number of pregnancies from pregnancy registries suggest that oxcarbazepine monotherapy use is associated with congenital malformations (e.g., craniofacial defects such as oral clefts, and cardiac malformations such as ventricular septal defects). Increased incidences of fetal structural abnormalities and other manifestations of developmental toxicity (embryolethality, growth retardation) were observed in the offspring of animals treated with either oxcarbazepine or its active 10-hydroxy metabolite (MHD) during pregnancy at doses similar to the maximum recommended human dose (MRHD). In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown. Clinical Considerations An increase in seizure frequency may occur during pregnancy because of altered levels of the active metabolite of oxcarbazepine. Monitor patients carefully during pregnancy and through the postpartum period [see Warnings and Precautions ( 5.9 )] Data Human Data Data from published registries have reported craniofacial defects such as oral clefts and cardiac malformations such as ventricular septal defects in children with prenatal oxcarbazepine exposure. Animal Data When pregnant rats were given oxcarbazepine (30, 300, or 1,000 mg/kg/day) orally throughout the period of organogenesis, increased incidences of fetal malformations (craniofacial, cardiovascular, and skeletal) and variations were observed at the intermediate and high doses (approximately 1.2 and 4 times, respectively, the MRHD on a mg/m 2 basis). Increased embryofetal death and decreased fetal body weights were seen at the high dose. Doses ≥ 300 mg/kg were also maternally toxic (decreased body weight gain, clinical signs), but there is no evidence to suggest that teratogenicity was secondary to the maternal effects. In a study in which pregnant rabbits were orally administered MHD (20, 100, or 200 mg/kg/day) during organogenesis, embryofetal mortality was increased at the highest dose (1.5 times the MRHD on a mg/m 2 basis). This dose produced only minimal maternal toxicity. In a study in which female rats were dosed orally with oxcarbazepine (25, 50, or 150 mg/kg/day) during the latter part of gestation and throughout the lactation period, a persistent reduction in body weights and altered behavior (decreased activity) were observed in offspring exposed to the highest dose (0.6 times the MRHD on a mg/m 2 basis). Oral administration of MHD (25, 75, or 250 mg/kg/day) to rats during gestation and lactation resulted in a persistent reduction in offspring weights at the highest dose (equivalent to the MRHD on a mg/m 2 basis).
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS Pregnancy: May cause fetal harm. ( 5.9 , 8.1 ) Severe Hepatic Impairment: Not recommended. ( 8.7 ) 8.1 Pregnancy Pregnancy Exposure Registry There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to AEDs, such as oxcarbazepine extended-release tablets, during pregnancy. Encourage women who are taking oxcarbazepine extended-release tablets during pregnancy to enroll in the North American Antiepileptic Drug (NAAED Pregnancy Registry) by calling 1-888-233-2334 or visiting http://www.aedpregnancyregistry.org/ . Risk Summary There are no adequate data on the developmental risks associated with the use of oxcarbazepine extended-release tablets in pregnant women; however, oxcarbazepine extended-release tablets are closely related structurally to carbamazepine, which is considered to be teratogenic in humans. Data on a limited number of pregnancies from pregnancy registries suggest that oxcarbazepine monotherapy use is associated with congenital malformations (e.g., craniofacial defects such as oral clefts, and cardiac malformations such as ventricular septal defects). Increased incidences of fetal structural abnormalities and other manifestations of developmental toxicity (embryolethality, growth retardation) were observed in the offspring of animals treated with either oxcarbazepine or its active 10-hydroxy metabolite (MHD) during pregnancy at doses similar to the maximum recommended human dose (MRHD). In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. The background risk of major birth defects and miscarriage for the indicated population is unknown. Clinical Considerations An increase in seizure frequency may occur during pregnancy because of altered levels of the active metabolite of oxcarbazepine. Monitor patients carefully during pregnancy and through the postpartum period [see Warnings and Precautions ( 5.9 )] Data Human Data Data from published registries have reported craniofacial defects such as oral clefts and cardiac malformations such as ventricular septal defects in children with prenatal oxcarbazepine exposure. Animal Data When pregnant rats were given oxcarbazepine (30, 300, or 1,000 mg/kg/day) orally throughout the period of organogenesis, increased incidences of fetal malformations (craniofacial, cardiovascular, and skeletal) and variations were observed at the intermediate and high doses (approximately 1.2 and 4 times, respectively, the MRHD on a mg/m 2 basis). Increased embryofetal death and decreased fetal body weights were seen at the high dose. Doses ≥ 300 mg/kg were also maternally toxic (decreased body weight gain, clinical signs), but there is no evidence to suggest that teratogenicity was secondary to the maternal effects. In a study in which pregnant rabbits were orally administered MHD (20, 100, or 200 mg/kg/day) during organogenesis, embryofetal mortality was increased at the highest dose (1.5 times the MRHD on a mg/m 2 basis). This dose produced only minimal maternal toxicity. In a study in which female rats were dosed orally with oxcarbazepine (25, 50, or 150 mg/kg/day) during the latter part of gestation and throughout the lactation period, a persistent reduction in body weights and altered behavior (decreased activity) were observed in offspring exposed to the highest dose (0.6 times the MRHD on a mg/m 2 basis). Oral administration of MHD (25, 75, or 250 mg/kg/day) to rats during gestation and lactation resulted in a persistent reduction in offspring weights at the highest dose (equivalent to the MRHD on a mg/m 2 basis). 8.2 Lactation Risk Summary Oxcarbazepine and its active metabolite (MHD) are present in human milk after oxcarbazepine administration. The effects of oxcarbazepine and its active metabolite (MHD) on the breastfed infant or on milk production are unknown. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for oxcarbazepine extended-release tablets and any potential adverse effects on the breastfed infant from oxcarbazepine extended-release tablets or from the underlying maternal condition. 8.3 Females and Males of Reproductive Potential Contraception Use of oxcarbazepine extended-release tablets with hormonal contraceptives containing ethinylestradiol or levonorgestrel is associated with decreased plasma concentrations of these hormones and may result in a failure of the therapeutic effect of the oral contraceptive drug. Advise women of reproductive potential taking oxcarbazepine extended-release tablets who are using a contraceptive containing ethinylestradiol or levonorgestrel to use additional or alternative non-hormonal birth control [see Drug Interactions ( 7.3 ) and Clinical Pharmacology ( 12.3 )]. 8.4 Pediatric Use The safety and effectiveness of oxcarbazepine extended-release tablets in pediatric patients 6 years of age and older for the treatment of partial-onset seizures is supported by: 1) An adequate and well-controlled safety and efficacy study of oxcarbazepine extended-release tablets in adults that included pharmacokinetic sampling [see Clinical Studies ( 14.1 )] , 2) A pharmacokinetic study of oxcarbazepine extended-release tablets in pediatric patients, which included patients 6 to less than 17 years of age [see Clinical Pharmacology ( 12.3 )] , 3) Safety and efficacy studies with the immediate-release formulation in adults and pediatric patients [see Clinical Studies ( 14.2 ) and Adverse Reactions ( 6.1 )] . Oxcarbazepine extended-release tablets is not approved for pediatric patients less than 6 years of age because the size of the tablets are inappropriate for younger children. 8.5 Geriatric Use Following administration of single (300 mg) and multiple (600 mg/day) doses of immediate-release oxcarbazepine to elderly volunteers (60 to 82 years of age), the maximum plasma concentrations and AUC values of MHD were 30% to 60% higher than in younger volunteers (18 to 32 years of age). Comparisons of creatinine clearance in young and elderly volunteers indicate that the difference was due to age-related reductions in creatinine clearance. Consider starting at a lower dosage and lower titration [see Dosage and Administration ( 2.4 )] . Close monitoring of sodium levels is required in elderly patients at risk for hyponatremia [see Warnings and Precautions ( 5.1 )] . 8.6 Renal Impairment There is a linear correlation between creatinine clearance and the renal clearance of MHD [see Clinical Pharmacology ( 12.3 ) and Dosage and Administration ( 2.3 )]. The pharmacokinetics of oxcarbazepine extended-release tablets has not been evaluated in patients with renal impairment. In patients with severe renal impairment (creatinine clearance <30 mL/min) given immediate-release oxcarbazepine, the elimination half-life of MHD was prolonged with a corresponding two-fold increase in AUC [see Clinical Pharmacology ( 12.3 )] . In these patients initiate oxcarbazepine extended-release tablets at a lower starting dosage and increase, if necessary, at a slower than usual rate until the desired clinical response is achieved [ see Dosage and Administration ( 2.3 )]. In patients with end-stage renal disease on dialysis, it is recommended that immediate-release oxcarbazepine be used instead of oxcarbazepine extended-release tablets. 8.7 Hepatic Impairment The pharmacokinetics of oxcarbazepine and MHD has not been evaluated in severe hepatic impairment, and therefore is not recommended in these patients [see Clinical Pharmacology (12.3 )].
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING 16.1 How Supplied 150 mg: Yellow, oval, biconvex film-coated tablet. Engraved “OX150” on one side, “APO” on the other side. Bottles of 100 tablets with child-resistant closure..…………………… NDC 60505-4128-7 Bottles of 500 tablets……………………………………………………NDC 60505-4128-5 300 mg: Brown, oval, biconvex film-coated tablet. Engraved “OX300” on one side, “APO” on the other side. Bottles of 100 tablets with child-resistant closure ………………….. NDC 60505-4129-7 Bottles of 500 tablets…………………………………………………. NDC 60505-4129-5 600 mg: Brownish red, oval, biconvex film-coated tablet. Engraved “OX600” on one side, “APO” on the other side. Bottles of 100 tablets with child-resistant closure………………… NDC 60505-4130-7 Bottles of 500 tablets………………………………………………. NDC 60505-4130-5 16.2 Storage and Handling Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F) [See USP controlled room temperature]. Protect from light and moisture. Dispense in a tight, light-resistant container.
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API