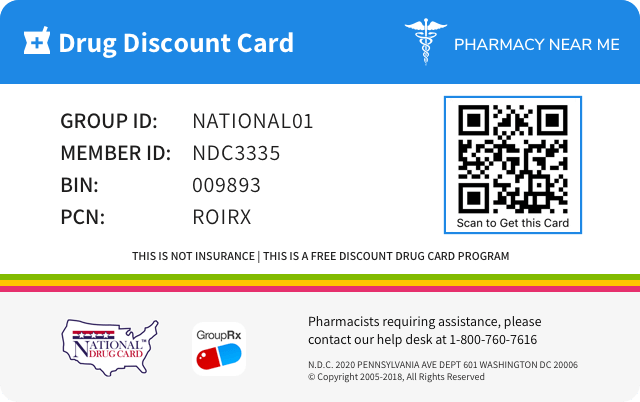
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 63187-429 | ||||
|---|---|---|---|---|---|
| Drug Name | Olanzapine |
||||
| Type | Generic | ||||
| Pharm Class | Atypical Antipsychotic [EPC] | ||||
| Active Ingredients |
|
||||
| Route | ORAL | ||||
| Dosage Form | TABLET, FILM COATED | ||||
| RxCUI drug identifier | 200034, 314154 |
||||
| Application Number | ANDA090798 | ||||
| Labeler Name | Proficient Rx LP | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Dependence
Information about characteristic effects resulting from both psychological and physical dependence that occur with the drug, the quantity of drug over a period of time that may lead to tolerance or dependence, details of adverse effects related to chronic abuse and the effects of abrupt withdrawl, procedures necessary to diagnose the dependent state, and principles of treating the effects of abrupt withdrawal.9.3 Dependence In studies prospectively designed to assess abuse and dependence potential, olanzapine was shown to have acute depressive CNS effects but little or no potential of abuse or physical dependence in rats administered oral doses up to 15 times the maximum recommended human daily oral dose (20 mg) and rhesus monkeys administered oral doses up to 8 times the maximum recommended human daily oral dose on a mg/m 2 basis. Olanzapine has not been systematically studied in humans for its potential for abuse, tolerance, or physical dependence. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic, and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of misuse or abuse of olanzapine (e.g., development of tolerance, increases in dose, drug-seeking behavior).
Drug abuse and dependence
Information about whether the drug is a controlled substance, the types of abuse that can occur with the drug, and adverse reactions pertinent to those types of abuse.9 DRUG ABUSE AND DEPENDENCE 9.3 Dependence In studies prospectively designed to assess abuse and dependence potential, olanzapine was shown to have acute depressive CNS effects but little or no potential of abuse or physical dependence in rats administered oral doses up to 15 times the maximum recommended human daily oral dose (20 mg) and rhesus monkeys administered oral doses up to 8 times the maximum recommended human daily oral dose on a mg/m 2 basis. Olanzapine has not been systematically studied in humans for its potential for abuse, tolerance, or physical dependence. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic, and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of misuse or abuse of olanzapine (e.g., development of tolerance, increases in dose, drug-seeking behavior).
Overdosage of Olanzapine
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE 10.1 Human Experience In premarketing trials involving more than 3100 patients and/or normal subjects, accidental or intentional acute overdosage of olanzapine was identified in 67 patients. In the patient taking the largest identified amount, 300 mg, the only symptoms reported were drowsiness and slurred speech. In the limited number of patients who were evaluated in hospitals, including the patient taking 300 mg, there were no observations indicating an adverse change in laboratory analytes or ECG. Vital signs were usually within normal limits following overdoses. In postmarketing reports of overdose with olanzapine alone, symptoms have been reported in the majority of cases. In symptomatic patients, symptoms with ≥10% incidence included agitation/aggressiveness, dysarthria, tachycardia, various extrapyramidal symptoms, and reduced level of consciousness ranging from sedation to coma. Among less commonly reported symptoms were the following potentially medically serious reactions: aspiration, cardiopulmonary arrest, cardiac arrhythmias (such as supraventricular tachycardia and 1 patient experiencing sinus pause with spontaneous resumption of normal rhythm), delirium, possible neuroleptic malignant syndrome, respiratory depression/arrest, convulsion, hypertension, and hypotension. Reports have been received of fatality in association with overdose of olanzapine alone. In 1 case of death, the amount of acutely ingested olanzapine was reported to be possibly as low as 450 mg of oral olanzapine; however, in another case, a patient was reported to survive an acute olanzapine ingestion of approximately 2 g of oral olanzapine. 10.2 Management of Overdose The possibility of multiple drug involvement should be considered. In case of acute overdosage, establish and maintain an airway and ensure adequate oxygenation and ventilation, which may include intubation. Gastric lavage (after intubation, if patient is unconscious) and administration of activated charcoal together with a laxative should be considered. The administration of activated charcoal (1 g) reduced the Cmax and AUC of oral olanzapine by about 60%. As peak olanzapine levels are not typically obtained until about 6 hours after dosing, charcoal may be a useful treatment for olanzapine overdose. The possibility of obtundation, seizures, or dystonic reaction of the head and neck following overdose may create a risk of aspiration with induced emesis. Cardiovascular monitoring should commence immediately and should include continuous electrocardiographic monitoring to detect possible arrhythmias. There is no specific antidote to olanzapine. Therefore, appropriate supportive measures should be initiated. Hypotension and circulatory collapse should be treated with appropriate measures such as intravenous fluids and/or sympathomimetic agents. (Do not use epinephrine, dopamine, or other sympathomimetics with beta-agonist activity, since beta stimulation may worsen hypotension in the setting of olanzapine-induced alpha blockade.) Close medical supervision and monitoring should continue until the patient recovers. For specific information about overdosage with lithium or valproate, refer to the Overdosage section of the package inserts for these products. For specific information about overdosage with olanzapine and fluoxetine in combination, refer to the Overdosage section of the Symbyax ® package insert.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS When using olanzapine tablets and fluoxetine in combination, also refer to the Adverse Reactions section of the package insert for Symbyax ® . Most common adverse reactions (≥5% and at least twice that for placebo) associated with: Oral Olanzapine Monotherapy: • Schizophrenia (Adults) – postural hypotension, constipation, weight gain, dizziness, personality disorder, akathisia ( 6.1 ) • Schizophrenia (Adolescents) – sedation, weight increased, headache, increased appetite, dizziness, abdominal pain, pain in extremity, fatigue, dry mouth ( 6.1 ) • Manic or Mixed Episodes, Bipolar I Disorder (Adults) – asthenia, dry mouth, constipation, increased appetite, somnolence, dizziness, tremor ( 6.1 ) • Manic or Mixed Episodes, Bipolar I Disorder (Adolescents) – sedation, weight increased, increased appetite, headache, fatigue, dizziness, dry mouth, abdominal pain, pain in extremity ( 6.1 ) Combination of Olanzapine Tablets and Lithium or Valproate: • Manic or Mixed Episodes, Bipolar I Disorder (Adults) – dry mouth, weight gain, increased appetite, dizziness, back pain, constipation, speech disorder, increased salivation, amnesia, paresthesia ( 6.1 ) Olanzapine tablets and Fluoxetine in Combination: Also refer to the Adverse Reactions section of the package insert for Symbyax ® . ( 6 ) To report SUSPECTED ADVERSE REACTIONS, contact Apotex Corp. at 1-800-667-4708 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect or predict the rates observed in practice. Clinical Trials in Adults The information below for olanzapine is derived from a clinical trial database for olanzapine consisting of 8661 adult patients with approximately 4165 patient-years of exposure to oral olanzapine and 722 patients with exposure to intramuscular olanzapine for injection. This database includes: (1) 2500 patients who participated in multiple-dose oral olanzapine premarketing trials in schizophrenia and Alzheimer's disease representing approximately 1122 patient-years of exposure as of February 14, 1995; (2) 182 patients who participated in oral olanzapine premarketing bipolar I disorder (manic or mixed episodes) trials representing approximately 66 patient-years of exposure; (3) 191 patients who participated in an oral olanzapine trial of patients having various psychiatric symptoms in association with Alzheimer's disease representing approximately 29 patient-years of exposure; (4) 5788 patients from 88 additional oral olanzapine clinical trials as of December 31, 2001; and (5) 722 patients who participated in intramuscular olanzapine for injection premarketing trials in agitated patients with schizophrenia, bipolar I disorder (manic or mixed episodes), or dementia. In addition, information from the premarketing 6-week clinical study database for olanzapine in combination with lithium or valproate, consisting of 224 patients who participated in bipolar I disorder (manic or mixed episodes) trials with approximately 22 patient-years of exposure, is included below. The conditions and duration of treatment with olanzapine varied greatly and included (in overlapping categories) open-label and double-blind phases of studies, inpatients and outpatients, fixed-dose and dose-titration studies, and short-term or longer-term exposure. Adverse reactions were assessed by collecting adverse reactions, results of physical examinations, vital signs, weights, laboratory analytes, ECGs, chest x-rays, and results of ophthalmologic examinations. Certain portions of the discussion below relating to objective or numeric safety parameters, namely, dose-dependent adverse reactions, vital sign changes, weight gain, laboratory changes, and ECG changes are derived from studies in patients with schizophrenia and have not been duplicated for bipolar I disorder (manic or mixed episodes) or agitation. However, this information is also generally applicable to bipolar I disorder (manic or mixed episodes) and agitation. Adverse reactions during exposure were obtained by spontaneous report and recorded by clinical investigators using terminology of their own choosing. Consequently, it is not possible to provide a meaningful estimate of the proportion of individuals experiencing adverse reactions without first grouping similar types of reactions into a smaller number of standardized reaction categories. In the tables and tabulations that follow, MedDRA and COSTART Dictionary terminology has been used to classify reported adverse reactions. The stated frequencies of adverse reactions represent the proportion of individuals who experienced, at least once, a treatment-emergent adverse reaction of the type listed. A reaction was considered treatment emergent if it occurred for the first time or worsened while receiving therapy following baseline evaluation. The reported reactions do not include those reaction terms that were so general as to be uninformative. Reactions listed elsewhere in labeling may not be repeated below. It is important to emphasize that, although the reactions occurred during treatment with olanzapine, they were not necessarily caused by it. The entire label should be read to gain a complete understanding of the safety profile of olanzapine. The prescriber should be aware that the figures in the tables and tabulations cannot be used to predict the incidence of side effects in the course of usual medical practice where patient characteristics and other factors differ from those that prevailed in the clinical trials. Similarly, the cited frequencies cannot be compared with figures obtained from other clinical investigations involving different treatments, uses, and investigators. The cited figures, however, do provide the prescribing physician with some basis for estimating the relative contribution of drug and nondrug factors to the adverse reactions incidence in the population studied. Incidence of Adverse Reactions in Short-Term, Placebo-Controlled and Combination Trials The following findings are based on premarketing trials of oral olanzapine for schizophrenia, bipolar I disorder (manic or mixed episodes), a subsequent trial of patients having various psychiatric symptoms in association with Alzheimer's disease, and premarketing combination trials. Adverse Reactions Associated with Discontinuation of Treatment in Short-Term, Placebo-Controlled Trials Schizophrenia — Overall, there was no difference in the incidence of discontinuation due to adverse reactions (5% for oral olanzapine vs 6% for placebo). However, discontinuations due to increases in ALT were considered to be drug related (2% for oral olanzapine vs 0% for placebo). Bipolar I Disorder (Manic or Mixed Episodes) Monotherapy — Overall, there was no difference in the incidence of discontinuation due to adverse reactions (2% for oral olanzapine vs 2% for placebo). Adverse Reactions Associated with Discontinuation of Treatment in Short-Term Combination Trials Bipolar I Disorder (Manic or Mixed Episodes), Olanzapine as Adjunct to Lithium or Valproate — In a study of patients who were already tolerating either lithium or valproate as monotherapy, discontinuation rates due to adverse reactions were 11% for the combination of oral olanzapine with lithium or valproate compared to 2% for patients who remained on lithium or valproate monotherapy. Discontinuations with the combination of oral olanzapine and lithium or valproate that occurred in more than 1 patient were: somnolence (3%), weight gain (1%), and peripheral edema (1%). Commonly Observed Adverse Reactions in Short-Term, Placebo-Controlled Trials The most commonly observed adverse reactions associated with the use of oral olanzapine (incidence of 5% or greater) and not observed at an equivalent incidence among placebo-treated patients (olanzapine incidence at least twice that for placebo) were: Table 9: Common Treatment-Emergent Adverse Reactions Associated with the Use of Oral Olanzapine in 6-Week Trials — SCHIZOPHRENIA a Personality disorder is the COSTART term for designating nonaggressive objectionable behavior. Adverse Reaction Percentage of Patients Reporting Event Olanzapine (N=248) Placebo (N=118) Postural hypotension 5 2 Constipation 9 3 Weight gain 6 1 Dizziness 11 4 Personality disorder a 8 4 Akathisia 5 1 Table 10: Common Treatment-Emergent Adverse Reactions Associated with the Use of Oral Olanzapine in 3-Week and 4-Week Trials — Bipolar I Disorder (Manic or Mixed Episodes) Adverse Reaction Percentage of Patients Reporting Event Olanzapine (N=125) Placebo (N=129) Asthenia 15 6 Dry mouth 22 7 Constipation 11 5 Dyspepsia 11 5 Increased appetite 6 3 Somnolence 35 13 Dizziness 18 6 Tremor 6 3 Adverse Reactions Occurring at an Incidence of 2% or More among Oral Olanzapine-Treated Patients in Short-Term, Placebo-Controlled Trials Table 11 enumerates the incidence, rounded to the nearest percent, of treatment-emergent adverse reactions that occurred in 2% or more of patients treated with oral olanzapine (doses ≥2.5 mg/day) and with incidence greater than placebo who participated in the acute phase of placebo-controlled trials. Table 11: Treatment-Emergent Adverse Reactions: Incidence in Short-Term, Placebo-Controlled Clinical Trials with Oral Olanzapine Body System/Adverse Reaction Percentage of Patients Reporting Event Olanzapine (N=532) Placebo (N=294) Body as a Whole Accidental injury 12 8 Asthenia 10 9 Fever 6 2 Back pain 5 2 Chest pain 3 1 Cardiovascular System Postural hypotension 3 1 Tachycardia 3 1 Hypertension 2 1 Digestive System Dry mouth 9 5 Constipation 9 4 Dyspepsia 7 5 Vomiting 4 3 Increased appetite 3 2 Hemic and Lymphatic System Ecchymosis 5 3 Metabolic and Nutritional Disorders Weight gain 5 3 Peripheral edema 3 1 Musculoskeletal System Extremity pain (other than joint) 5 3 Joint pain 5 3 Nervous System Somnolence 29 13 Insomnia 12 11 Dizziness 11 4 Abnormal gait 6 1 Tremor 4 3 Akathisia 3 2 Hypertonia 3 2 Articulation impairment 2 1 Respiratory System Rhinitis 7 6 Cough increased 6 3 Pharyngitis 4 3 Special Senses Amblyopia 3 2 Urogenital System Urinary incontinence 2 1 Urinary tract infection 2 1 Commonly Observed Adverse Reactions in Short-Term Trials of Oral Olanzapine as Adjunct to Lithium or Valproate In the bipolar I disorder (manic or mixed episodes) adjunct placebo-controlled trials, the most commonly observed adverse reactions associated with the combination of olanzapine and lithium or valproate (incidence of ≥5% and at least twice placebo) were: Table 12: Common Treatment-Emergent Adverse Reactions Associated with the Use of Oral Olanzapine in 6-Week Adjunct to Lithium or Valproate Trials — Bipolar I Disorder (Manic or Mixed Episodes) Adverse Reaction Percentage of Patients Reporting Event Olanzapine with lithium or valproate (N=229) Placebo with lithium or valproate (N=115) Dry mouth 32 9 Weight gain 26 7 Increased appetite 24 8 Dizziness 14 7 Back pain 8 4 Constipation 8 4 Speech disorder 7 1 Increased salivation 6 2 Amnesia 5 2 Paresthesia 5 2 Adverse Reactions Occurring at an Incidence of 2% or More among Oral Olanzapine-Treated Patients in Short-Term Trials of Olanzapine as Adjunct to Lithium or Valproate Table 13 enumerates the incidence, rounded to the nearest percent, of treatment-emergent adverse reactions that occurred in 2% or more of patients treated with the combination of olanzapine (doses ≥5 mg/day) and lithium or valproate and with incidence greater than lithium or valproate alone who participated in the acute phase of placebo-controlled combination trials. Table 13: Treatment-Emergent Adverse Reactions: Incidence in Short-Term, Placebo-Controlled Clinical Trials of Oral Olanzapine as Adjunct to Lithium or Valproate a Denominator used was for females only (olanzapine, N=128; placebo, N=51). Body System/Adverse Reaction Percentage of Patients Reporting Event Olanzapine with lithium or valproate (N=229) Placebo with lithium or valproate (N=115) Body as a Whole Asthenia 18 13 Back pain 8 4 Accidental injury 4 2 Chest pain 3 2 Cardiovascular System Hypertension 2 1 Digestive System Dry mouth 32 9 Increased appetite 24 8 Thirst 10 6 Constipation 8 4 Increased salivation 6 2 Metabolic and Nutritional Disorders Weight gain 26 7 Peripheral edema 6 4 Edema 2 1 Nervous System Somnolence 52 27 Tremor 23 13 Depression 18 17 Dizziness 14 7 Speech disorder 7 1 Amnesia 5 2 Paresthesia 5 2 Apathy 4 3 Confusion 4 1 Euphoria 3 2 Incoordination 2 0 Respiratory System Pharyngitis 4 1 Dyspnea 3 1 Skin and Appendages Sweating 3 1 Acne 2 0 Dry skin 2 0 Special Senses Amblyopia 9 5 Abnormal vision 2 0 Urogenital System Dysmenorrhea a 2 0 Vaginitis a 2 0 For specific information about the adverse reactions observed with lithium or valproate, refer to the Adverse Reactions section of the package inserts for these other products. Additional Findings Observed in Clinical Trials Dose Dependency of Adverse Reactions in Short-Term, Placebo-Controlled Trials Extrapyramidal Symptoms: The following table enumerates the percentage of patients with treatment-emergent extrapyramidal symptoms as assessed by categorical analyses of formal rating scales during acute therapy in a controlled clinical trial comparing oral olanzapine at 3 fixed doses with placebo in the treatment of schizophrenia in a 6-week trial. Table 15: Treatment-Emergent Extrapyramidal Symptoms Assessed by Rating Scales Incidence in a Fixed Dosage Range, Placebo-Controlled Clinical Trial of Oral Olanzapine in Schizophrenia — Acute Phase a Percentage of patients with a Simpson-Angus Scale total score >3. b Percentage of patients with a Barnes Akathisia Scale global score ≥2. Percentage of Patients Reporting Event Placebo Olanzapine 5 ± 2.5 mg/day Olanzapine 10 ± 2.5 mg/day Olanzapine 15 ± 2.5 mg/day Parkinsonism a 15 14 12 14 Akathisia b 23 16 19 27 The following table enumerates the percentage of patients with treatment-emergent extrapyramidal symptoms as assessed by spontaneously reported adverse reactions during acute therapy in the same controlled clinical trial comparing olanzapine at 3 fixed doses with placebo in the treatment of schizophrenia in a 6-week trial. Table 16: Treatment-Emergent Extrapyramidal Symptoms Assessed by Adverse Reactions Incidence in a Fixed Dosage Range, Placebo-Controlled Clinical Trial of Oral Olanzapine in Schizophrenia — Acute Phase a Patients with the following COSTART terms were counted in this category: dystonia, generalized spasm, neck rigidity, oculogyric crisis, opisthotonos, torticollis. b Patients with the following COSTART terms were counted in this category: akinesia, cogwheel rigidity, extrapyramidal syndrome, hypertonia, hypokinesia, masked facies, tremor. c Patients with the following COSTART terms were counted in this category: akathisia, hyperkinesia. d Patients with the following COSTART terms were counted in this category: buccoglossal syndrome, choreoathetosis, dyskinesia, tardive dyskinesia. e Patients with the following COSTART terms were counted in this category: movement disorder, myoclonus, twitching. Percentage of Patients Reporting Event Placebo (N=68) Olanzapine 5 ± 2.5 mg/day (N=65) Olanzapine 10 ± 2.5 mg/day (N=64) Olanzapine 15 ± 2.5 mg/day (N=69) Dystonic events a 1 3 2 3 Parkinsonism events b 10 8 14 20 Akathisia events c 1 5 11 10 Dyskinetic events d 4 0 2 1 Residual events e 1 2 5 1 Any extrapyramidal event 16 15 25 32 The following table enumerates the percentage of adolescent patients with treatment-emergent extrapyramidal symptoms as assessed by spontaneously reported adverse reactions during acute therapy (dose range: 2.5 to 20 mg/day). Table 17: Treatment-Emergent Extrapyramidal Symptoms Assessed by Adverse Reactions Incidence in Placebo-Controlled Clinical Trials of Oral Olanzapine in Schizophrenia and Bipolar I Disorder — Adolescents a Categories are based on Standard MedDRA Queries (SMQ) for extrapyramidal symptoms as defined in MedDRA version 12.0. Percentage of Patients Reporting Event Placebo Olanzapine Categories a (N=89) (N=179) Dystonic events 0 1 Parkinsonism events 2 1 Akathisia events 4 6 Dyskinetic events 0 1 Nonspecific events 0 4 Any extrapyramidal event 6 10 Dystonia, Class Effect: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, the frequency and severity are greater with high potency and at higher doses of first generation antipsychotic drugs. In general, an elevated risk of acute dystonia may be observed in males and younger age groups receiving antipsychotics; however, events of dystonia have been reported infrequently (<1%) with olanzapine use. Other Adverse Reactions: The following table addresses dose relatedness for other adverse reactions using data from a schizophrenia trial involving fixed dosage ranges of oral olanzapine. It enumerates the percentage of patients with treatment-emergent adverse reactions for the 3 fixed-dose range groups and placebo. The data were analyzed using the Cochran-Armitage test, excluding the placebo group, and the table includes only those adverse reactions for which there was a trend. Table 20: Percentage of Patients from a Schizophrenia Trial with Treatment-Emergent Adverse Reactions for the 3 Dose Range Groups and Placebo Adverse Reaction Percentage of Patients Reporting Event Placebo (N=68) Olanzapine 5 ± 2.5 mg/day (N=65) Olanzapine 10 ± 2.5 mg/day (N=64) Olanzapine 15 ± 2.5 mg/day (N=69) Asthenia 15 8 9 20 Dry mouth 4 3 5 13 Nausea 9 0 2 9 Somnolence 16 20 30 39 Tremor 3 0 5 7 Differences among Fixed-Dose Groups Observed in Other Olanzapine Clinical Trials In a single 8-week randomized, double-blind, fixed-dose study comparing 10 (N=199), 20 (N=200) and 40 (N=200) mg/day of oral olanzapine in patients with schizophrenia or schizoaffective disorder, differences among 3 dose groups were observed for the following safety outcomes: weight gain, prolactin elevation, fatigue and dizziness. Mean baseline to endpoint increase in weight (10 mg/day: 1.9 kg; 20 mg/day: 2.3 kg; 40 mg/day: 3 kg) was observed with significant differences between 10 vs 40 mg/day. Incidence of treatment-emergent prolactin elevation >24.2 ng/mL (female) or >18.77 ng/mL (male) at any time during the trial (10 mg/day: 31.2%; 20 mg/day: 42.7%; 40 mg/day: 61.1%) with significant differences between 10 vs 40 mg/day and 20 vs 40 mg/day; fatigue (10 mg/day: 1.5%; 20 mg/day: 2.1%; 40 mg/day: 6.6%) with significant differences between 10 vs 40 and 20 vs 40 mg/day; and dizziness (10 mg/day: 2.6%; 20 mg/day: 1.6%; 40 mg/day: 6.6%) with significant differences between 20 vs 40 mg, was observed. Other Adverse Reactions Observed During the Clinical Trial Evaluation of Oral Olanzapine Following is a list of treatment-emergent adverse reactions reported by patients treated with oral olanzapine (at multiple doses ≥1 mg/day) in clinical trials. This listing is not intended to include reactions (1) already listed in previous tables or elsewhere in labeling, (2) for which a drug cause was remote, (3) which were so general as to be uninformative, (4) which were not considered to have significant clinical implications, or (5) which occurred at a rate equal to or less than placebo. Reactions are classified by body system using the following definitions: frequent adverse reactions are those occurring in at least 1/100 patients; infrequent adverse reactions are those occurring in 1/100 to 1/1000 patients; rare reactions are those occurring in fewer than 1/1000 patients. Body as a Whole — Infrequent: chills, face edema, photosensitivity reaction, suicide attempt 1 ; Rare: chills and fever, hangover effect, sudden death 1 . Cardiovascular System — Infrequent: cerebrovascular accident, vasodilatation. Digestive System — Infrequent: nausea and vomiting, tongue edema; Rare: ileus, intestinal obstruction, liver fatty deposit. Hemic and Lymphatic System — Infrequent: leukopenia, thrombocytopenia. Metabolic and Nutritional Disorders — Infrequent: alkaline phosphatase increased, bilirubinemia, hypoproteinemia. Musculoskeletal System — Rare: osteoporosis. Nervous System — Infrequent: ataxia, dysarthria, libido decreased, stupor; Rare: coma. Respiratory System — Infrequent: epistaxis; Rare: lung edema. Skin and Appendages — Infrequent: alopecia. Special Senses — Infrequent: abnormality of accommodation, dry eyes; Rare: mydriasis. Urogenital System — Infrequent: amenorrhea 2 , breast pain, decreased menstruation, impotence 2 , increased menstruation 2 , menorrhagia 2 , metrorrhagia 2 , polyuria 2 , urinary frequency, urinary retention, urinary urgency, urination impaired. 1 These terms represent serious adverse events but do not meet the definition for adverse drug reactions. They are included here because of their seriousness. 2 Adjusted for gender. Clinical Trials in Adolescent Patients (age 13 to 17 years) Commonly Observed Adverse Reactions in Oral Olanzapine Short-Term, Placebo-Controlled Trials Adverse reactions in adolescent patients treated with oral olanzapine (doses ≥2.5 mg) reported with an incidence of 5% or more and reported at least twice as frequently as placebo-treated patients are listed in Table 21 . Table 21: Treatment-Emergent Adverse Reactions of ≥5% Incidence among Adolescents (13 to 17 Years Old) with Schizophrenia or Bipolar I Disorder (Manic or Mixed Episodes) a Patients with the following MedDRA terms were counted in this category: hypersomnia, lethargy, sedation, somnolence. b Patients with the following MedDRA terms were counted in this category: abdominal pain, abdominal pain lower, abdominal pain upper. Adverse Reactions Percentage of Patients Reporting Event 6 Week Trial % Schizophrenia Patients 3 Week Trial % Bipolar Patients Olanzapine (N=72) Placebo (N=35) Olanzapine (N=107) Placebo (N=54) Sedation a 39 9 48 9 Weight increased 31 9 29 4 Headache 17 6 17 17 Increased appetite 17 9 29 4 Dizziness 8 3 7 2 Abdominal pain b 6 3 6 7 Pain in extremity 6 3 5 0 Fatigue 3 3 14 6 Dry mouth 4 0 7 0 Adverse Reactions Occurring at an Incidence of 2% or More among Oral Olanzapine-Treated Patients in Short-Term (3 to 6 weeks), Placebo-Controlled Trials Adverse reactions in adolescent patients treated with oral olanzapine (doses ≥2.5 mg) reported with an incidence of 2% or more and greater than placebo are listed in Table 22 . Table 22: Treatment-Emergent Adverse Reactions of ≥2% Incidence among Adolescents (13 to 17 Years Old) (Combined Incidence from Short-Term, Placebo-Controlled Clinical Trials of Schizophrenia or Bipolar I Disorder [Manic or Mixed Episodes]) a Patients with the following MedDRA terms were counted in this category: hypersomnia, lethargy, sedation, somnolence. b The terms alanine aminotransferase (ALT), aspartate aminotransferase (AST), and hepatic enzyme were combined under liver enzymes. c Patients with the following MedDRA terms were counted in this category: lower respiratory tract infection, respiratory tract infection, respiratory tract infection viral, upper respiratory tract infection, viral upper respiratory tract infection. Adverse Reaction Percentage of Patients Reporting Event Olanzapine (N=179) Placebo (N=89) Sedation a 44 9 Weight increased 30 6 Increased appetite 24 6 Headache 17 12 Fatigue 9 4 Dizziness 7 2 Dry mouth 6 0 Pain in extremity 5 1 Constipation 4 0 Nasopharyngitis 4 2 Diarrhea 3 0 Restlessness 3 2 Liver enzymes increased b 8 1 Dyspepsia 3 1 Epistaxis 3 0 Respiratory tract infection c 3 2 Sinusitis 3 0 Arthralgia 2 0 Musculoskeletal stiffness 2 0 6.2 Vital Signs and Laboratory Studies Vital Sign Changes — Oral olanzapine was associated with orthostatic hypotension and tachycardia in clinical trials [see Warnings and Precautions ( 5 )] . Laboratory Changes Olanzapine Monotherapy in Adults: An assessment of the premarketing experience for olanzapine revealed an association with asymptomatic increases in ALT, AST, and GGT. Within the original premarketing database of about 2400 adult patients with baseline ALT ≤90 IU/L, the incidence of ALT elevations to >200 IU/L was 2% (50/2381). None of these patients experienced jaundice or other symptoms attributable to liver impairment and most had transient changes that tended to normalize while olanzapine treatment was continued. In placebo-controlled olanzapine monotherapy studies in adults, clinically significant ALT elevations (change from <3 times the upper limit of normal [ULN] at baseline to ≥3 times ULN) were observed in 5% (77/1426) of patients exposed to olanzapine compared to 1% (10/1187) of patients exposed to placebo. ALT elevations ≥5 times ULN were observed in 2% (29/1438) of olanzapine-treated patients, compared to 0.3% (4/1196) of placebo-treated patients. ALT values returned to normal, or were decreasing, at last follow-up in the majority of patients who either continued treatment with olanzapine or discontinued olanzapine. No patient with elevated ALT values experienced jaundice, liver failure, or met the criteria for Hy's Rule. Rare postmarketing reports of hepatitis have been received. Very rare cases of cholestatic or mixed liver injury have also been reported in the postmarketing period. Caution should be exercised in patients with signs and symptoms of hepatic impairment, in patients with pre-existing conditions associated with limited hepatic functional reserve, and in patients who are being treated with potentially hepatotoxic drugs. Olanzapine administration was also associated with increases in serum prolactin [see Warnings and Precautions ( 5.15 )] , with an asymptomatic elevation of the eosinophil count in 0.3% of patients, and with an increase in CPK. Olanzapine Monotherapy in Adolescents: In placebo-controlled clinical trials of adolescent patients with schizophrenia or bipolar I disorder (manic or mixed episodes), greater frequencies for the following treatment-emergent findings, at anytime, were observed in laboratory analytes compared to placebo: elevated ALT (≥3X ULN in patients with ALT at baseline <3X ULN), (12% vs 2%); elevated AST (28% vs 4%); low total bilirubin (22% vs 7%); elevated GGT (10% vs 1%); and elevated prolactin (47% vs 7%). In placebo-controlled olanzapine monotherapy studies in adolescents, clinically significant ALT elevations (change from <3 times ULN at baseline to ≥3 times ULN) were observed in 12% (22/192) of patients exposed to olanzapine compared to 2% (2/109) of patients exposed to placebo. ALT elevations ≥5 times ULN were observed in 4% (8/192) of olanzapine-treated patients, compared to 1% (1/109) of placebo-treated patients. ALT values returned to normal, or were decreasing, at last follow-up in the majority of patients who either continued treatment with olanzapine or discontinued olanzapine. No adolescent patient with elevated ALT values experienced jaundice, liver failure, or met the criteria for Hy's Rule. ECG Changes — In pooled studies of adults as well as pooled studies of adolescents, there were no significant differences between olanzapine and placebo in the proportions of patients experiencing potentially important changes in ECG parameters, including QT, QTc (Fridericia corrected), and PR intervals. Olanzapine use was associated with a mean increase in heart rate compared to placebo (adults: +2.4 beats per minute vs no change with placebo; adolescents: +6.3 beats per minute vs -5.1 beats per minute with placebo). This increase in heart rate may be related to olanzapine's potential for inducing orthostatic changes [see Warnings and Precautions ( 5.8 )] . 6.3 Postmarketing Experience The following adverse reactions have been identified during post-approval use of olanzapine. Because these reactions are reported voluntarily from a population of uncertain size, it is difficult to reliably estimate their frequency or evaluate a causal relationship to drug exposure. Adverse reactions reported since market introduction that were temporally (but not necessarily causally) related to olanzapine therapy include the following: allergic reaction (e.g., anaphylactoid reaction, angioedema, pruritus or urticaria), diabetic coma, diabetic ketoacidosis, discontinuation reaction (diaphoresis, nausea or vomiting), jaundice, neutropenia, pancreatitis, priapism, rash, rhabdomyolysis, and venous thromboembolic events (including pulmonary embolism and deep venous thrombosis). Random cholesterol levels of ≥240 mg/dL and random triglyceride levels of ≥1000 mg/dL have been reported.
| a Personality disorder is the COSTART term for designating nonaggressive objectionable behavior. | ||
| a Denominator used was for females only (olanzapine, N=128; placebo, N=51). | ||
| a Percentage of patients with a Simpson-Angus Scale total score >3. | ||||
| b Percentage of patients with a Barnes Akathisia Scale global score ≥2. | ||||
| a Patients with the following COSTART terms were counted in this category: dystonia, generalized spasm, neck rigidity, oculogyric crisis, opisthotonos, torticollis. | |||||||||
| b Patients with the following COSTART terms were counted in this category: akinesia, cogwheel rigidity, extrapyramidal syndrome, hypertonia, hypokinesia, masked facies, tremor. | |||||||||
| c Patients with the following COSTART terms were counted in this category: akathisia, hyperkinesia. | |||||||||
| d Patients with the following COSTART terms were counted in this category: buccoglossal syndrome, choreoathetosis, dyskinesia, tardive dyskinesia. | |||||||||
| e Patients with the following COSTART terms were counted in this category: movement disorder, myoclonus, twitching. | |||||||||
| a Categories are based on Standard MedDRA Queries (SMQ) for extrapyramidal symptoms as defined in MedDRA version 12.0. | ||||||||||||
| a Patients with the following MedDRA terms were counted in this category: hypersomnia, lethargy, sedation, somnolence. | ||||
| b Patients with the following MedDRA terms were counted in this category: abdominal pain, abdominal pain lower, abdominal pain upper. | ||||
| a Patients with the following MedDRA terms were counted in this category: hypersomnia, lethargy, sedation, somnolence. | ||
| b The terms alanine aminotransferase (ALT), aspartate aminotransferase (AST), and hepatic enzyme were combined under liver enzymes. | ||
| c Patients with the following MedDRA terms were counted in this category: lower respiratory tract infection, respiratory tract infection, respiratory tract infection viral, upper respiratory tract infection, viral upper respiratory tract infection. | ||
Olanzapine Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS The risks of using olanzapine in combination with other drugs have not been extensively evaluated in systematic studies. • Diazepam: May potentiate orthostatic hypotension. ( 7.1 , 7.2 ) • Alcohol: May potentiate orthostatic hypotension. ( 7.1 ) • Carbamazepine: Increased clearance of olanzapine. ( 7.1 ) • Fluvoxamine: May increase olanzapine levels. ( 7.1 ) • Olanzapine tablets and Fluoxetine in Combination: Also refer to the Drug Interactions section of the package insert for Symbyax ® . ( 7.1 ) • CNS Acting Drugs: Caution should be used when taken in combination with other centrally acting drugs and alcohol. ( 7.2 ) • Antihypertensive Agents: Enhanced antihypertensive effect. ( 7.2 ) • Levodopa and Dopamine Agonists: May antagonize levodopa/dopamine agonists. ( 7.2 ) • Lorazepam (IM): Increased somnolence with IM olanzapine. (7.2) • Other Concomitant Drug Therapy: When using olanzapine in combination with lithium or valproate, refer to the Drug Interactions sections of the package insert for those products. ( 7.2 ) 7.1 Potential for Other Drugs to Affect Olanzapine Diazepam — The co-administration of diazepam with olanzapine potentiated the orthostatic hypotension observed with olanzapine [see Drug Interactions ( 7.2 )] . Cimetidine and Antacids — Single doses of cimetidine (800 mg) or aluminum- and magnesium-containing antacids did not affect the oral bioavailability of olanzapine. Inducers of CYP1A2 — Carbamazepine therapy (200 mg bid) causes an approximately 50% increase in the clearance of olanzapine. This increase is likely due to the fact that carbamazepine is a potent inducer of CYP1A2 activity. Higher daily doses of carbamazepine may cause an even greater increase in olanzapine clearance. Alcohol — Ethanol (45 mg/70 kg single dose) did not have an effect on olanzapine pharmacokinetics. The co-administration of alcohol (i.e., ethanol) with olanzapine potentiated the orthostatic hypotension observed with olanzapine [see Drug Interactions ( 7.2 )] . Inhibitors of CYP1A2 Fluvoxamine: Fluvoxamine, a CYP1A2 inhibitor, decreases the clearance of olanzapine. This results in a mean increase in olanzapine Cmax following fluvoxamine of 54% in female nonsmokers and 77% in male smokers. The mean increase in olanzapine AUC is 52% and 108%, respectively. Lower doses of olanzapine should be considered in patients receiving concomitant treatment with fluvoxamine. Inhibitors of CYP2D6 Fluoxetine: Fluoxetine (60 mg single dose or 60 mg daily dose for 8 days) causes a small (mean 16%) increase in the maximum concentration of olanzapine and a small (mean 16%) decrease in olanzapine clearance. The magnitude of the impact of this factor is small in comparison to the overall variability between individuals, and therefore dose modification is not routinely recommended. When using olanzapine tablets and fluoxetine in combination, also refer to the Drug Interactions section of the package insert for Symbyax ® . Warfarin — Warfarin (20 mg single dose) did not affect olanzapine pharmacokinetics [see Drug Interactions ( 7.2 )] . Inducers of CYP1A2 or Glucuronyl Transferase — Omeprazole and rifampin may cause an increase in olanzapine clearance. Charcoal — The administration of activated charcoal (1 g) reduced the Cmax and AUC of oral olanzapine by about 60%. As peak olanzapine levels are not typically obtained until about 6 hours after dosing, charcoal may be a useful treatment for olanzapine overdose. 7.2 Potential for Olanzapine to Affect Other Drugs CNS Acting Drugs — Given the primary CNS effects of olanzapine, caution should be used when olanzapine is taken in combination with other centrally acting drugs and alcohol. Antihypertensive Agents — Olanzapine, because of its potential for inducing hypotension, may enhance the effects of certain antihypertensive agents. Levodopa and Dopamine Agonists — Olanzapine may antagonize the effects of levodopa and dopamine agonists. Lithium — Multiple doses of olanzapine (10 mg for 8 days) did not influence the kinetics of lithium. Therefore, concomitant olanzapine administration does not require dosage adjustment of lithium [see Warnings and Precautions ( 5.16 )] . Valproate — Olanzapine (10 mg daily for 2 weeks) did not affect the steady state plasma concentrations of valproate. Therefore, concomitant olanzapine administration does not require dosage adjustment of valproate [see Warnings and Precautions ( 5.16 )] . Effect of Olanzapine on Drug Metabolizing Enzymes — In vitro studies utilizing human liver microsomes suggest that olanzapine has little potential to inhibit CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A. Thus, olanzapine is unlikely to cause clinically important drug interactions mediated by these enzymes. Imipramine — Single doses of olanzapine did not affect the pharmacokinetics of imipramine or its active metabolite desipramine. Warfarin — Single doses of olanzapine did not affect the pharmacokinetics of warfarin [see Drug Interactions ( 7.1 )] . Diazepam — Olanzapine did not influence the pharmacokinetics of diazepam or its active metabolite N-desmethyldiazepam. However, diazepam co-administered with olanzapine increased the orthostatic hypotension observed with either drug given alone [see Drug Interactions ( 7.1 )] . Alcohol — Multiple doses of olanzapine did not influence the kinetics of ethanol [see Drug Interactions ( 7.1 )] . Biperiden — Multiple doses of olanzapine did not influence the kinetics of biperiden. Theophylline — Multiple doses of olanzapine did not affect the pharmacokinetics of theophylline or its metabolites.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action The mechanism of action of olanzapine, as with other drugs having efficacy in schizophrenia, is unknown. However, it has been proposed that this drug's efficacy in schizophrenia is mediated through a combination of dopamine and serotonin type 2 (5HT2) antagonism. The mechanism of action of olanzapine in the treatment of acute manic or mixed episodes associated with bipolar I disorder is unknown. 12.2 Pharmacodynamics Olanzapine binds with high affinity to the following receptors: serotonin 5HT 2A/2C , 5HT 6 (K i =4, 11, and 5 nM, respectively), dopamine D 1-4 (K i =11 to 31 nM), histamine H 1 (K i =7 nM), and adrenergic α 1 receptors (K i =19 nM). Olanzapine is an antagonist with moderate affinity binding for serotonin 5HT 3 (K i =57 nM) and muscarinic M 1-5 (K i =73, 96, 132, 32, and 48 nM, respectively). Olanzapine binds weakly to GABA A , BZD, and β-adrenergic receptors (K i >10 μM). Antagonism at receptors other than dopamine and 5HT 2 may explain some of the other therapeutic and side effects of olanzapine. Olanzapine's antagonism of muscarinic M 1-5 receptors may explain its anticholinergic-like effects. Olanzapine's antagonism of histamine H 1 receptors may explain the somnolence observed with this drug. Olanzapine's antagonism of adrenergic α 1 receptors may explain the orthostatic hypotension observed with this drug. 12.3 Pharmacokinetics Oral Administration, Monotherapy — Olanzapine is well absorbed and reaches peak concentrations in approximately 6 hours following an oral dose. It is eliminated extensively by first pass metabolism, with approximately 40% of the dose metabolized before reaching the systemic circulation. Food does not affect the rate or extent of olanzapine absorption. Pharmacokinetic studies showed that olanzapine tablets and olanzapine orally disintegrating tablets dosage forms of olanzapine are bioequivalent. Olanzapine displays linear kinetics over the clinical dosing range. Its half-life ranges from 21 to 54 hours (5th to 95th percentile; mean of 30 hr), and apparent plasma clearance ranges from 12 to 47 L/hr (5th to 95th percentile; mean of 25 L/hr). Administration of olanzapine once daily leads to steady-state concentrations in about 1 week that are approximately twice the concentrations after single doses. Plasma concentrations, half-life, and clearance of olanzapine may vary between individuals on the basis of smoking status, gender, and age. Olanzapine is extensively distributed throughout the body, with a volume of distribution of approximately 1000 L. It is 93% bound to plasma proteins over the concentration range of 7 to 1100 ng/mL, binding primarily to albumin and α 1 -acid glycoprotein. Metabolism and Elimination — Following a single oral dose of 14 C labeled olanzapine, 7% of the dose of olanzapine was recovered in the urine as unchanged drug, indicating that olanzapine is highly metabolized. Approximately 57% and 30% of the dose was recovered in the urine and feces, respectively. In the plasma, olanzapine accounted for only 12% of the AUC for total radioactivity, indicating significant exposure to metabolites. After multiple dosing, the major circulating metabolites were the 10-N-glucuronide, present at steady state at 44% of the concentration of olanzapine, and 4′-N-desmethyl olanzapine, present at steady state at 31% of the concentration of olanzapine. Both metabolites lack pharmacological activity at the concentrations observed. Direct glucuronidation and cytochrome P450 (CYP) mediated oxidation are the primary metabolic pathways for olanzapine. In vitro studies suggest that CYPs 1A2 and 2D6, and the flavin-containing monooxygenase system are involved in olanzapine oxidation. CYP2D6 mediated oxidation appears to be a minor metabolic pathway in vivo, because the clearance of olanzapine is not reduced in subjects who are deficient in this enzyme. Specific Populations Renal Impairment — Because olanzapine is highly metabolized before excretion and only 7% of the drug is excreted unchanged, renal dysfunction alone is unlikely to have a major impact on the pharmacokinetics of olanzapine. The pharmacokinetic characteristics of olanzapine were similar in patients with severe renal impairment and normal subjects, indicating that dosage adjustment based upon the degree of renal impairment is not required. In addition, olanzapine is not removed by dialysis. The effect of renal impairment on metabolite elimination has not been studied. Hepatic Impairment — Although the presence of hepatic impairment may be expected to reduce the clearance of olanzapine, a study of the effect of impaired liver function in subjects (n=6) with clinically significant (Childs Pugh Classification A and B) cirrhosis revealed little effect on the pharmacokinetics of olanzapine. Geriatric — In a study involving 24 healthy subjects, the mean elimination half-life of olanzapine was about 1.5 times greater in elderly (≥65 years) than in nonelderly subjects (<65 years). Caution should be used in dosing the elderly, especially if there are other factors that might additively influence drug metabolism and/or pharmacodynamic sensitivity [see Dosage and Administration ( 2 )] . Gender — Clearance of olanzapine is approximately 30% lower in women than in men. There were, however, no apparent differences between men and women in effectiveness or adverse effects. Dosage modifications based on gender should not be needed. Smoking Status — Olanzapine clearance is about 40% higher in smokers than in nonsmokers, although dosage modifications are not routinely recommended. Race — In vivo studies have shown that exposures are similar among Japanese, Chinese and Caucasians, especially after normalization for body weight differences. Dosage modifications for race are, therefore, not recommended. Combined Effects — The combined effects of age, smoking, and gender could lead to substantial pharmacokinetic differences in populations. The clearance in young smoking males, for example, may be 3 times higher than that in elderly nonsmoking females. Dosing modification may be necessary in patients who exhibit a combination of factors that may result in slower metabolism of olanzapine [see Dosage and Administration ( 2 )] . Adolescents (ages 13 to 17 years) — Pharmacokinetic information in pediatric patients is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action The mechanism of action of olanzapine, as with other drugs having efficacy in schizophrenia, is unknown. However, it has been proposed that this drug's efficacy in schizophrenia is mediated through a combination of dopamine and serotonin type 2 (5HT2) antagonism. The mechanism of action of olanzapine in the treatment of acute manic or mixed episodes associated with bipolar I disorder is unknown.
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Olanzapine binds with high affinity to the following receptors: serotonin 5HT 2A/2C , 5HT 6 (K i =4, 11, and 5 nM, respectively), dopamine D 1-4 (K i =11 to 31 nM), histamine H 1 (K i =7 nM), and adrenergic α 1 receptors (K i =19 nM). Olanzapine is an antagonist with moderate affinity binding for serotonin 5HT 3 (K i =57 nM) and muscarinic M 1-5 (K i =73, 96, 132, 32, and 48 nM, respectively). Olanzapine binds weakly to GABA A , BZD, and β-adrenergic receptors (K i >10 μM). Antagonism at receptors other than dopamine and 5HT 2 may explain some of the other therapeutic and side effects of olanzapine. Olanzapine's antagonism of muscarinic M 1-5 receptors may explain its anticholinergic-like effects. Olanzapine's antagonism of histamine H 1 receptors may explain the somnolence observed with this drug. Olanzapine's antagonism of adrenergic α 1 receptors may explain the orthostatic hypotension observed with this drug.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Oral Administration, Monotherapy — Olanzapine is well absorbed and reaches peak concentrations in approximately 6 hours following an oral dose. It is eliminated extensively by first pass metabolism, with approximately 40% of the dose metabolized before reaching the systemic circulation. Food does not affect the rate or extent of olanzapine absorption. Pharmacokinetic studies showed that olanzapine tablets and olanzapine orally disintegrating tablets dosage forms of olanzapine are bioequivalent. Olanzapine displays linear kinetics over the clinical dosing range. Its half-life ranges from 21 to 54 hours (5th to 95th percentile; mean of 30 hr), and apparent plasma clearance ranges from 12 to 47 L/hr (5th to 95th percentile; mean of 25 L/hr). Administration of olanzapine once daily leads to steady-state concentrations in about 1 week that are approximately twice the concentrations after single doses. Plasma concentrations, half-life, and clearance of olanzapine may vary between individuals on the basis of smoking status, gender, and age. Olanzapine is extensively distributed throughout the body, with a volume of distribution of approximately 1000 L. It is 93% bound to plasma proteins over the concentration range of 7 to 1100 ng/mL, binding primarily to albumin and α 1 -acid glycoprotein. Metabolism and Elimination — Following a single oral dose of 14 C labeled olanzapine, 7% of the dose of olanzapine was recovered in the urine as unchanged drug, indicating that olanzapine is highly metabolized. Approximately 57% and 30% of the dose was recovered in the urine and feces, respectively. In the plasma, olanzapine accounted for only 12% of the AUC for total radioactivity, indicating significant exposure to metabolites. After multiple dosing, the major circulating metabolites were the 10-N-glucuronide, present at steady state at 44% of the concentration of olanzapine, and 4′-N-desmethyl olanzapine, present at steady state at 31% of the concentration of olanzapine. Both metabolites lack pharmacological activity at the concentrations observed. Direct glucuronidation and cytochrome P450 (CYP) mediated oxidation are the primary metabolic pathways for olanzapine. In vitro studies suggest that CYPs 1A2 and 2D6, and the flavin-containing monooxygenase system are involved in olanzapine oxidation. CYP2D6 mediated oxidation appears to be a minor metabolic pathway in vivo, because the clearance of olanzapine is not reduced in subjects who are deficient in this enzyme. Specific Populations Renal Impairment — Because olanzapine is highly metabolized before excretion and only 7% of the drug is excreted unchanged, renal dysfunction alone is unlikely to have a major impact on the pharmacokinetics of olanzapine. The pharmacokinetic characteristics of olanzapine were similar in patients with severe renal impairment and normal subjects, indicating that dosage adjustment based upon the degree of renal impairment is not required. In addition, olanzapine is not removed by dialysis. The effect of renal impairment on metabolite elimination has not been studied. Hepatic Impairment — Although the presence of hepatic impairment may be expected to reduce the clearance of olanzapine, a study of the effect of impaired liver function in subjects (n=6) with clinically significant (Childs Pugh Classification A and B) cirrhosis revealed little effect on the pharmacokinetics of olanzapine. Geriatric — In a study involving 24 healthy subjects, the mean elimination half-life of olanzapine was about 1.5 times greater in elderly (≥65 years) than in nonelderly subjects (<65 years). Caution should be used in dosing the elderly, especially if there are other factors that might additively influence drug metabolism and/or pharmacodynamic sensitivity [see Dosage and Administration ( 2 )] . Gender — Clearance of olanzapine is approximately 30% lower in women than in men. There were, however, no apparent differences between men and women in effectiveness or adverse effects. Dosage modifications based on gender should not be needed. Smoking Status — Olanzapine clearance is about 40% higher in smokers than in nonsmokers, although dosage modifications are not routinely recommended. Race — In vivo studies have shown that exposures are similar among Japanese, Chinese and Caucasians, especially after normalization for body weight differences. Dosage modifications for race are, therefore, not recommended. Combined Effects — The combined effects of age, smoking, and gender could lead to substantial pharmacokinetic differences in populations. The clearance in young smoking males, for example, may be 3 times higher than that in elderly nonsmoking females. Dosing modification may be necessary in patients who exhibit a combination of factors that may result in slower metabolism of olanzapine [see Dosage and Administration ( 2 )] . Adolescents (ages 13 to 17 years) — Pharmacokinetic information in pediatric patients is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS • None with olanzapine tablets monotherapy. • When using olanzapine tablets and fluoxetine in combination, also refer to the Contraindications section of the package insert for Symbyax ® . • For specific information about the contraindications of lithium or valproate, refer to the Contraindications section of the package inserts for these other products. • None with olanzapine tablets monotherapy. • When using olanzapine tablets and fluoxetine in combination, also refer to the Contraindications section of the package insert for Symbyax ® . ( 4 ) • When using olanzapine tablets in combination with lithium or valproate, refer to the Contraindications section of the package inserts for those products. ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION Olanzapine is an atypical antipsychotic that belongs to the thienobenzodiazepine class. The chemical designation is 2-methyl-4-(4-methyl-1-piperazinyl)-10 H -thieno[2,3- b ] [1,5]benzodiazepine. The molecular formula is C 17 H 20 N 4 S, which corresponds to a molecular weight of 312.43. The chemical structure is: Olanzapine is a yellow powder. Olanzapine Tablets, USP are intended for oral administration only. Each tablet contains olanzapine equivalent to 2.5 mg (8 μmol), 5 mg (16 μmol), 7.5 mg (24 μmol), 10 mg (32 μmol), 15 mg (48 μmol), or 20 mg (64 μmol). Inactive ingredients are lactose, microcrystalline cellulose, starch, magnesium stearate. The color coating contains hypromellose, hydroxypropyl cellulose, polyethylene glycol, titanium dioxide (all strengths), FD&C Blue No.2 Aluminum Lake (15 mg), or red ferric oxide and yellow iron oxide (20 mg). structure
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION Schizophrenia in adults ( 2.1 ) Oral: Start at 5 to 10 mg once daily; Target: 10 mg/day within several days Bipolar I Disorder (manic or mixed episodes) in adults ( 2.2 ) Oral: Start at 10 or 15 mg once daily Bipolar I Disorder (manic or mixed episodes) with lithium or valproate in adults ( 2.2 ) Oral: Start at 10 mg once daily Depressive Episodes associated with Bipolar I Disorder in adults ( 2.5 ) Oral in combination with fluoxetine: Start at 5 mg of oral olanzapine and 20 mg of fluoxetine once daily • Lower starting dose recommended in debilitated or pharmacodynamically sensitive patients or patients with predisposition to hypotensive reactions, or with potential for slowed metabolism. ( 2.1 ) • Olanzapine may be given without regard to meals. ( 2.1 ) Olanzapine tablets and fluoxetine in combination: • Dosage adjustments, if indicated, should be made with the individual components according to efficacy and tolerability. ( 2.5 ) • Olanzapine monotherapy is not indicated for the treatment of depressive episodes associated with bipolar I disorder. ( 2.5 ) • Safety of co-administration of doses above 18 mg olanzapine with 75 mg fluoxetine has not been evaluated. ( 2.5 ) 2.1 Schizophrenia Adults Dose Selection — Oral olanzapine should be administered on a once-a-day schedule without regard to meals, generally beginning with 5 to 10 mg initially, with a target dose of 10 mg/day within several days. Further dosage adjustments, if indicated, should generally occur at intervals of not less than 1 week, since steady state for olanzapine would not be achieved for approximately 1 week in the typical patient. When dosage adjustments are necessary, dose increments/decrements of 5 mg QD are recommended. Efficacy in schizophrenia was demonstrated in a dose range of 10 to 15 mg/day in clinical trials. However, doses above 10 mg/day were not demonstrated to be more efficacious than the 10 mg/day dose. An increase to a dose greater than the target dose of 10 mg/day (i.e., to a dose of 15 mg/day or greater) is recommended only after clinical assessment. Olanzapine is not indicated for use in doses above 20 mg/day. Dosing in Special Populations — The recommended starting dose is 5 mg in patients who are debilitated, who have a predisposition to hypotensive reactions, who otherwise exhibit a combination of factors that may result in slower metabolism of olanzapine (e.g., nonsmoking female patients ≥65 years of age), or who may be more pharmacodynamically sensitive to olanzapine [see Warnings and Precautions ( 5.14 ), Drug Interactions ( 7 ), and Clinical Pharmacology ( 12.3 )] . When indicated, dose escalation should be performed with caution in these patients. Maintenance Treatment — The effectiveness of oral olanzapine, 10 mg/day to 20 mg/day, in maintaining treatment response in schizophrenic patients who had been stable on olanzapine for approximately 8 weeks and were then followed for relapse has been demonstrated in a placebo-controlled trial [see Clinical Studies ( 14.1 )] . The physician who elects to use olanzapine tablets for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient. Adolescents Pediatric dosing information in pediatric patients with schizophrenia is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. 2.2 Bipolar I Disorder (Manic or Mixed Episodes) Adults Dose Selection for Monotherapy — Oral olanzapine should be administered on a once-a-day schedule without regard to meals, generally beginning with 10 or 15 mg. Dosage adjustments, if indicated, should generally occur at intervals of not less than 24 hours, reflecting the procedures in the placebo-controlled trials. When dosage adjustments are necessary, dose increments/decrements of 5 mg QD are recommended. Short-term (3 to 4 weeks) antimanic efficacy was demonstrated in a dose range of 5 mg to 20 mg/day in clinical trials. The safety of doses above 20 mg/day has not been evaluated in clinical trials [see Clinical Studies ( 14.2 )] . Maintenance Monotherapy — The benefit of maintaining bipolar I patients on monotherapy with oral olanzapine at a dose of 5 to 20 mg/day, after achieving a responder status for an average duration of 2 weeks, was demonstrated in a controlled trial [see Clinical Studies ( 14.2 )] . The physician who elects to use olanzapine tablets for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient. Dose Selection for Adjunctive Treatment — When administered as adjunctive treatment to lithium or valproate, oral olanzapine dosing should generally begin with 10 mg once-a-day without regard to meals. Antimanic efficacy was demonstrated in a dose range of 5 mg to 20 mg/day in clinical trials [see Clinical Studies ( 14.2 )] . The safety of doses above 20 mg/day has not been evaluated in clinical trials. Adolescents Pediatric dosing information in pediatric patients with bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. 2.5 Olanzapine tablets and Fluoxetine in Combination: Depressive Episodes Associated with Bipolar I Disorder When using olanzapine tablets and fluoxetine in combination, also refer to the Clinical Studies section of the package insert for Symbyax ® . Oral olanzapine should be administered in combination with fluoxetine once daily in the evening, without regard to meals, generally beginning with 5 mg of oral olanzapine and 20 mg of fluoxetine. Dosage adjustments, if indicated, can be made according to efficacy and tolerability within dose ranges of oral olanzapine 5 to 12.5 mg and fluoxetine 20 to 50 mg. Antidepressant efficacy was demonstrated with olanzapine and fluoxetine in combination in adult patients with a dose range of olanzapine 6 to 12 mg and fluoxetine 25 to 50 mg. Safety and efficacy of olanzapine and fluoxetine in combination was determined in clinical trials supporting approval of Symbyax ® (fixed dose combination of olanzapine and fluoxetine). Symbyax ® is dosed between 3 mg/25 mg (olanzapine/fluoxetine) per day and 12 mg/50 mg (olanzapine/fluoxetine) per day. The following table demonstrates the appropriate individual component doses of olanzapine and fluoxetine versus Symbyax ® . Dosage adjustments, if indicated, should be made with the individual components according to efficacy and tolerability. Table 1: Approximate Dose Correspondence Between Symbyax ®a and the Combination of Olanzapine and Fluoxetine a Symbyax ® (olanzapine/fluoxetine HCl) is a fixed-dose combination of olanzapine and fluoxetine. For Use in Combination Symbyax ® Olanzapine Fluoxetine (mg/day) (mg/day) (mg/day) 3 mg olanzapine/25 mg fluoxetine 2.5 20 6 mg olanzapine/25 mg fluoxetine 5 20 12 mg olanzapine/25 mg fluoxetine 10+2.5 20 6 mg olanzapine/50 mg fluoxetine 5 40+10 12 mg olanzapine/50 mg fluoxetine 10+2.5 40+10 While there is no body of evidence to answer the question of how long a patient treated with olanzapine tablets and fluoxetine in combination should remain on it, it is generally accepted that bipolar I disorder, including the depressive episodes associated with bipolar I disorder, is a chronic illness requiring chronic treatment. The physician should periodically reexamine the need for continued pharmacotherapy. Safety of co-administration of doses above 18 mg olanzapine with 75 mg fluoxetine has not been evaluated in clinical studies. Olanzapine tablets monotherapy is not indicated for the treatment of depressive episodes associated with bipolar I disorder. 2.7 Olanzapine tablets and Fluoxetine in Combination: Dosing in Special Populations The starting dose of oral olanzapine 2.5 to 5 mg with fluoxetine 20 mg should be used for patients with a predisposition to hypotensive reactions, patients with hepatic impairment, or patients who exhibit a combination of factors that may slow the metabolism of olanzapine or fluoxetine in combination (female gender, geriatric age, nonsmoking status), or those patients who may be pharmacodynamically sensitive to olanzapine. Dosing modification may be necessary in patients who exhibit a combination of factors that may slow metabolism. When indicated, dose escalation should be performed with caution in these patients. Olanzapine and fluoxetine in combination have not been systematically studied in patients over 65 years of age or in patients <18 years of age [see Warnings and Precautions ( 5.14 ), Drug Interactions ( 7 ), and Clinical Pharmacology ( 12.3 )] .
| a Symbyax® (olanzapine/fluoxetine HCl) is a fixed-dose combination of olanzapine and fluoxetine. | ||
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Olanzapine Tablets, USP are available as follows: Olanzapine Tablets, USP 2.5 mg are white, round, biconvex film-coated tablets, engraved "APO" on one side, "OLA" over "2.5" on the other side. Olanzapine Tablets, USP 5 mg are white, round, biconvex film-coated tablets, engraved “APO” on one side, “OLA” over “5” on the other side. Olanzapine Tablets, USP 7.5 mg are white, round, biconvex film-coated tablets, engraved “APO” on one side, “OLA” over “7.5” on the other side. Olanzapine Tablets, USP 10 mg are white, round, biconvex film-coated tablets, engraved “APO” on one side, “OLA” over “10” on the other side. Olanzapine Tablets, USP 15 mg are light blue, elliptical, biconvex film-coated tablets, engraved “APO” on one side, “OLA 15” on the other side. Olanzapine Tablets, USP 20 mg are light pink, elliptical, biconvex film-coated tablets, engraved “APO” on one side, “OLA 20” on the other side. • Tablets (not scored): 2.5, 5, 7.5, 10, 15, 20 mg ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE Olanzapine Tablets, USP are an atypical antipsychotic indicated: As oral formulation for the: • Treatment of schizophrenia. ( 1.1 ) • Adults: Efficacy was established in three clinical trials in patients with schizophrenia: two 6-week trials and one maintenance trial. ( 14.1 ) • Acute treatment of manic or mixed episodes associated with bipolar I disorder and maintenance treatment of bipolar I disorder. ( 1.2 ) • Adults: Efficacy was established in three clinical trials in patients with manic or mixed episodes of bipolar I disorder: two 3- to 4-week trials and one maintenance trial. ( 14.2 ) • Adjunct to valproate or lithium in the treatment of manic or mixed episodes associated with bipolar I disorder. ( 1.2 ) • Efficacy was established in two 6-week clinical trials in adults ( 14.2 ). Maintenance efficacy has not been systematically evaluated. As olanzapine tablets and fluoxetine in combination for the: • Treatment of depressive episodes associated with bipolar I disorder. ( 1.5 ) • Efficacy was established with Symbyax ® (olanzapine and fluoxetine in combination) in adults; refer to the product label for Symbyax ® . 1.1 Schizophrenia Olanzapine Tablets, USP are indicated for the treatment of schizophrenia. Efficacy was established in three clinical trials in adult patients with schizophrenia: two 6-week trials and one maintenance trial. [see Clinical Studies ( 14.1 )] . When deciding among the alternative treatments available for adolescents, clinicians should consider the increased potential (in adolescents as compared with adults) for weight gain and hyperlipidemia. Clinicians should consider the potential long-term risks when prescribing to adolescents, and in many cases this may lead them to consider prescribing other drugs first in adolescents [see Warnings and Precautions ( 5.5 , 5.6 )] . Information describing the use of olanzapine tablets and olanzapine orally disintegrating tablets in pediatric patients with schizophrenia is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. 1.2 Bipolar I Disorder (Manic or Mixed Episodes) Monotherapy — Olanzapine Tablets, USP are indicated for the acute treatment of manic or mixed episodes associated with bipolar I disorder and maintenance treatment of bipolar I disorder. Efficacy was established in three clinical trials in adult patients with manic or mixed episodes of bipolar I disorder: two 3- to 4-week trials and one monotherapy maintenance trial. [see Clinical Studies ( 14.2 )] . When deciding among the alternative treatments available for adolescents, clinicians should consider the increased potential (in adolescents as compared with adults) for weight gain and hyperlipidemia. Clinicians should consider the potential long-term risks when prescribing to adolescents, and in many cases this may lead them to consider prescribing other drugs first in adolescents [see Warnings and Precautions ( 5.5 , 5.6 )] . Information describing the use of olanzapine tablets and olanzapine orally disintegrating tablets in pediatric patients with bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. Adjunctive Therapy to Lithium or Valproate — Olanzapine Tablets, USP are indicated for the treatment of manic or mixed episodes associated with bipolar I disorder as an adjunct to lithium or valproate. Efficacy was established in two 6-week clinical trials in adults. The effectiveness of adjunctive therapy for longer-term use has not been systematically evaluated in controlled trials [see Clinical Studies ( 14.2 )] . 1.3 Special Considerations in Treating Pediatric Schizophrenia and Bipolar I Disorder Information on treating pediatric patients with schizophrenia and bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. 1.5 Olanzapine tablets and Fluoxetine in Combination: Depressive Episodes Associated with Bipolar I Disorder Olanzapine tablets and fluoxetine in combination is indicated for the treatment of depressive episodes associated with bipolar I disorder, based on clinical studies in adult patients. When using olanzapine tablets and fluoxetine in combination, refer to the Clinical Studies section of the package insert for Symbyax ® . Olanzapine tablets monotherapy is not indicated for the treatment of depressive episodes associated with bipolar I disorder.
Spl product data elements
Usually a list of ingredients in a drug product.Olanzapine Olanzapine OLANZAPINE OLANZAPINE LACTOSE MONOHYDRATE MICROCRYSTALLINE CELLULOSE STARCH, CORN HYPROMELLOSE 2910 (6 MPA.S) MAGNESIUM STEARATE HYDROXYPROPYL CELLULOSE (1600000 WAMW) POLYETHYLENE GLYCOL, UNSPECIFIED TITANIUM DIOXIDE APO;OLA;2;5 Olanzapine Olanzapine OLANZAPINE OLANZAPINE LACTOSE MONOHYDRATE MICROCRYSTALLINE CELLULOSE STARCH, CORN HYPROMELLOSE 2910 (6 MPA.S) MAGNESIUM STEARATE HYDROXYPROPYL CELLULOSE (1600000 WAMW) POLYETHYLENE GLYCOL, UNSPECIFIED TITANIUM DIOXIDE APO;OLA;10
Animal pharmacology and or toxicology
Information from studies of the drug in animals, if the data were not relevant to nor included in other parts of the labeling. Most labels do not contain this field.13.2 Animal Toxicology and/or Pharmacology In animal studies with olanzapine, the principal hematologic findings were reversible peripheral cytopenias in individual dogs dosed at 10 mg/kg (17 times the maximum recommended human daily oral dose on a mg/m 2 basis), dose-related decreases in lymphocytes and neutrophils in mice, and lymphopenia in rats. A few dogs treated with 10 mg/kg developed reversible neutropenia and/or reversible hemolytic anemia between 1 and 10 months of treatment. Dose-related decreases in lymphocytes and neutrophils were seen in mice given doses of 10 mg/kg (equal to 2 times the maximum recommended human daily oral dose on a mg/m 2 basis) in studies of 3 months' duration. Nonspecific lymphopenia, consistent with decreased body weight gain, occurred in rats receiving 22.5 mg/kg (11 times the maximum recommended human daily oral dose on a mg/m 2 basis) for 3 months or 16 mg/kg (8 times the maximum recommended human daily oral dose on a mg/m 2 basis) for 6 or 12 months. No evidence of bone marrow cytotoxicity was found in any of the species examined. Bone marrows were normocellular or hypercellular, indicating that the reductions in circulating blood cells were probably due to peripheral (non-marrow) factors.
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis — Oral carcinogenicity studies were conducted in mice and rats. Olanzapine was administered to mice in two 78-week studies at doses of 3, 10, 30/20 mg/kg/day (equivalent to 0.8 to 5 times the maximum recommended human daily oral dose on a mg/m 2 basis) and 0.25, 2, 8 mg/kg/day (equivalent to 0.06 to 2 times the maximum recommended human daily oral dose on a mg/m 2 basis). Rats were dosed for 2 years at doses of 0.25, 1, 2.5, 4 mg/kg/day (males) and 0.25, 1, 4, 8 mg/kg/day (females) (equivalent to 0.13 to 2 and 0.13 to 4 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively). The incidence of liver hemangiomas and hemangiosarcomas was significantly increased in 1 mouse study in female mice dosed at 8 mg/kg/day (2 times the maximum recommended human daily oral dose on a mg/m 2 basis). These tumors were not increased in another mouse study in females dosed at 10 or 30/20 mg/kg/day (2 to 5 times the maximum recommended human daily oral dose on a mg/m 2 basis); in this study, there was a high incidence of early mortalities in males of the 30/20 mg/kg/day group. The incidence of mammary gland adenomas and adenocarcinomas was significantly increased in female mice dosed at ≥2 mg/kg/day and in female rats dosed at ≥4 mg/kg/day (0.5 and 2 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively). Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the olanzapine carcinogenicity studies; however, measurements during subchronic toxicity studies showed that olanzapine elevated serum prolactin levels up to 4-fold in rats at the same doses used in the carcinogenicity study. An increase in mammary gland neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin mediated. The relevance for human risk of the finding of prolactin mediated endocrine tumors in rodents is unknown [see Warnings and Precautions ( 5.15 )] . Mutagenesis — No evidence of genotoxic potential for olanzapine was found in the Ames reverse mutation test, in vivo micronucleus test in mice, the chromosomal aberration test in Chinese hamster ovary cells, unscheduled DNA synthesis test in rat hepatocytes, induction of forward mutation test in mouse lymphoma cells, or in vivo sister chromatid exchange test in bone marrow of Chinese hamsters. Impairment of Fertility — In an oral fertility and reproductive performance study in rats, male mating performance, but not fertility, was impaired at a dose of 22.4 mg/kg/day and female fertility was decreased at a dose of 3 mg/kg/day (11 and 1.5 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively). Discontinuance of olanzapine treatment reversed the effects on male mating performance. In female rats, the precoital period was increased and the mating index reduced at 5 mg/kg/day (2.5 times the maximum recommended human daily oral dose on a mg/m 2 basis). Diestrous was prolonged and estrous delayed at 1.1 mg/kg/day (0.6 times the maximum recommended human daily oral dose on a mg/m 2 basis); therefore olanzapine may produce a delay in ovulation.
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis — Oral carcinogenicity studies were conducted in mice and rats. Olanzapine was administered to mice in two 78-week studies at doses of 3, 10, 30/20 mg/kg/day (equivalent to 0.8 to 5 times the maximum recommended human daily oral dose on a mg/m 2 basis) and 0.25, 2, 8 mg/kg/day (equivalent to 0.06 to 2 times the maximum recommended human daily oral dose on a mg/m 2 basis). Rats were dosed for 2 years at doses of 0.25, 1, 2.5, 4 mg/kg/day (males) and 0.25, 1, 4, 8 mg/kg/day (females) (equivalent to 0.13 to 2 and 0.13 to 4 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively). The incidence of liver hemangiomas and hemangiosarcomas was significantly increased in 1 mouse study in female mice dosed at 8 mg/kg/day (2 times the maximum recommended human daily oral dose on a mg/m 2 basis). These tumors were not increased in another mouse study in females dosed at 10 or 30/20 mg/kg/day (2 to 5 times the maximum recommended human daily oral dose on a mg/m 2 basis); in this study, there was a high incidence of early mortalities in males of the 30/20 mg/kg/day group. The incidence of mammary gland adenomas and adenocarcinomas was significantly increased in female mice dosed at ≥2 mg/kg/day and in female rats dosed at ≥4 mg/kg/day (0.5 and 2 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively). Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the olanzapine carcinogenicity studies; however, measurements during subchronic toxicity studies showed that olanzapine elevated serum prolactin levels up to 4-fold in rats at the same doses used in the carcinogenicity study. An increase in mammary gland neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin mediated. The relevance for human risk of the finding of prolactin mediated endocrine tumors in rodents is unknown [see Warnings and Precautions ( 5.15 )] . Mutagenesis — No evidence of genotoxic potential for olanzapine was found in the Ames reverse mutation test, in vivo micronucleus test in mice, the chromosomal aberration test in Chinese hamster ovary cells, unscheduled DNA synthesis test in rat hepatocytes, induction of forward mutation test in mouse lymphoma cells, or in vivo sister chromatid exchange test in bone marrow of Chinese hamsters. Impairment of Fertility — In an oral fertility and reproductive performance study in rats, male mating performance, but not fertility, was impaired at a dose of 22.4 mg/kg/day and female fertility was decreased at a dose of 3 mg/kg/day (11 and 1.5 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively). Discontinuance of olanzapine treatment reversed the effects on male mating performance. In female rats, the precoital period was increased and the mating index reduced at 5 mg/kg/day (2.5 times the maximum recommended human daily oral dose on a mg/m 2 basis). Diestrous was prolonged and estrous delayed at 1.1 mg/kg/day (0.6 times the maximum recommended human daily oral dose on a mg/m 2 basis); therefore olanzapine may produce a delay in ovulation. 13.2 Animal Toxicology and/or Pharmacology In animal studies with olanzapine, the principal hematologic findings were reversible peripheral cytopenias in individual dogs dosed at 10 mg/kg (17 times the maximum recommended human daily oral dose on a mg/m 2 basis), dose-related decreases in lymphocytes and neutrophils in mice, and lymphopenia in rats. A few dogs treated with 10 mg/kg developed reversible neutropenia and/or reversible hemolytic anemia between 1 and 10 months of treatment. Dose-related decreases in lymphocytes and neutrophils were seen in mice given doses of 10 mg/kg (equal to 2 times the maximum recommended human daily oral dose on a mg/m 2 basis) in studies of 3 months' duration. Nonspecific lymphopenia, consistent with decreased body weight gain, occurred in rats receiving 22.5 mg/kg (11 times the maximum recommended human daily oral dose on a mg/m 2 basis) for 3 months or 16 mg/kg (8 times the maximum recommended human daily oral dose on a mg/m 2 basis) for 6 or 12 months. No evidence of bone marrow cytotoxicity was found in any of the species examined. Bone marrows were normocellular or hypercellular, indicating that the reductions in circulating blood cells were probably due to peripheral (non-marrow) factors.
Laboratory tests
Information on laboratory tests helpful in following the patient’s response to the drug or in identifying possible adverse reactions. If appropriate, information may be provided on such factors as the range of normal and abnormal values expected in the particular situation and the recommended frequency with which tests should be performed before, during, and after therapy.5.17 Laboratory Tests Fasting blood glucose testing and lipid profile at the beginning of, and periodically during, treatment is recommended [see Warnings and Precautions ( 5.4 , 5.5 ) and Patient Counseling Information ( 17.4 , 17.5 )] .
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PRINCIPAL DISPLAY PANEL - 2.5 MG LABEL NDC 63187-453-30 Olanzapine Tablets, USP 2.5 mg Rx only 30 Tablets 63187-453-30
PRINCIPAL DISPLAY PANEL - 10 MG LABEL NDC 63187-429-30 Olanzapine Tablets, USP 10 mg Rx only 30 Tablets 63187-429-30
Recent major changes
A list of the section(s) that contain substantive changes that have been approved by FDA in the product labeling. The headings and subheadings, if appropriate, affected by the change are listed together with each section’s identifying number and the month and year on which the change was incorporated in the labeling.• None
Spl unclassified section
Information not classified as belonging to one of the other fields. Approximately 40% of labeling with effective_time between June 2009 and August 2014 have information in this field.APOTEX INC. Olanzapine Tablets, USP 2.5 mg, 5.0 mg, 7.5 mg, 10 mg, 15 mg and 20 mg Manufactured by: Apotex Inc. Toronto, Ontario Canada M9L 1T9 Manufactured for: Apotex Corp. Weston, Florida USA 33326 Repackaged by: Proficient Rx LP Thousand Oaks, CA 91320 Revision 2 Revised: February 2012
Olanzapine: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION See FDA-approved Medication Guide . Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking olanzapine tablets as monotherapy or in combination with fluoxetine. If you do not think you are getting better or have any concerns about your condition while taking olanzapine tablets, call your doctor. When using olanzapine tablets and fluoxetine in combination, also refer to the Patient Counseling Information section of the package insert for Symbyax ® . 17.1 Information on Medication Guide Prescribers or other health professionals should inform patients, their families, and their caregivers about the potential benefits and potential risks associated with treatment with olanzapine tablets, and should counsel them in its appropriate use. A patient Medication Guide is available for olanzapine tablets. Prescribers or other health professionals should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. When using olanzapine tablets and fluoxetine in combination, also refer to the Medication Guide for Symbyax ® . 17.2 Elderly Patients with Dementia-Related Psychosis: Increased Mortality and Cerebrovascular Adverse Events (CVAE), Including Stroke Patients and caregivers should be advised that elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Patients and caregivers should be advised that elderly patients with dementia-related psychosis treated with olanzapine had a significantly higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack) compared with placebo. Olanzapine tablets are not approved for elderly patients with dementia-related psychosis [see Boxed Warning and Warnings and Precautions ( 5.1 )] . 17.3 Neuroleptic Malignant Syndrome (NMS) Patients and caregivers should be counseled that a potentially fatal symptom complex sometimes referred to as NMS has been reported in association with administration of antipsychotic drugs, including olanzapine. Signs and symptoms of NMS include hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia) [see Warnings and Precautions ( 5.3 )] . 17.4 Hyperglycemia Patients should be advised of the potential risk of hyperglycemia-related adverse reactions. Patients should be monitored regularly for worsening of glucose control. Patients who have diabetes should follow their doctor's instructions about how often to check their blood sugar while taking olanzapine tablets [see Warnings and Precautions ( 5.4 )] . 17.5 Hyperlipidemia Patients should be counseled that hyperlipidemia has occurred during treatment with olanzapine. Patients should have their lipid profile monitored regularly [see Warnings and Precautions ( 5.5 )] . 17.6 Weight Gain Patients should be counseled that weight gain has occurred during treatment with olanzapine. Patients should have their weight monitored regularly [see Warnings and Precautions ( 5.6 )] . 17.7 Orthostatic Hypotension Patients should be advised of the risk of orthostatic hypotension, especially during the period of initial dose titration and in association with the use of concomitant drugs that may potentiate the orthostatic effect of olanzapine tablets, e.g., diazepam or alcohol [see Warnings and Precautions ( 5.8 ) and Drug Interactions ( 7 )] . Patients should be advised to change positions carefully to help prevent orthostatic hypotension, and to lie down if they feel dizzy or faint, until they feel better. Patients should be advised to call their doctor if they experience any of the following signs and symptoms associated with orthostatic hypotension: dizziness, fast or slow heart beat, or fainting. 17.8 Potential for Cognitive and Motor Impairment Because olanzapine tablets have the potential to impair judgment, thinking, or motor skills, patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that olanzapine tablets therapy does not affect them adversely [see Warnings and Precautions ( 5.12 )] . 17.9 Body Temperature Regulation Patients should be advised regarding appropriate care in avoiding overheating and dehydration. Patients should be advised to call their doctor right away if they become severely ill and have some or all of these symptoms of dehydration: sweating too much or not at all, dry mouth, feeling very hot, feeling thirsty, not able to produce urine [see Warnings and Precautions ( 5.13 )] . 17.10 Concomitant Medication Patients should be advised to inform their physicians if they are taking, or plan to take, Symbyax ® . Patients should also be advised to inform their physicians if they are taking, plan to take, or have stopped taking any prescription or over-the-counter drugs, including herbal supplements, since there is a potential for interactions [see Drug Interactions ( 7 )] . 17.11 Alcohol Patients should be advised to avoid alcohol while taking olanzapine tablets [see Drug Interactions ( 7 )] . 17.13 Use in Specific Populations Pregnancy — Patients should be advised to notify their physician if they become pregnant or intend to become pregnant during therapy with olanzapine tablets [see Use in Specific Populations ( 8.1 )] . Nursing Mothers — Patients should be advised not to breast-feed an infant if they are taking olanzapine tablets [see Use in Specific Populations ( 8.3 )] . Pediatric Use — Compared to patients from adult clinical trials, adolescents were likely to gain more weight, experience increased sedation, and have greater increases in total cholesterol, triglycerides, LDL cholesterol, prolactin, and hepatic transaminase levels. Safety and effectiveness of olanzapine tablets in patients under 13 years of age have not been established. Safety and effectiveness of olanzapine tablets and fluoxetine in combination in patients <18 years of age have not been established [see Warnings and Precautions ( 5.5 , 5.6 ) and Use in Specific Populations ( 8.4 )] . Pediatric use information in pediatric patients with schizophrenia and bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. 17.14 Need for Comprehensive Treatment Program in Pediatric Patients Pediatric use information in pediatric patients with schizophrenia and bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. Symbyax ® is a registered trademark of Eli Lilly and Company. Prozac ® is a registered trademark of Eli Lilly and Company.
Spl medguide
Information about the patient medication guide that accompanies the drug product. Certain drugs must be dispensed with an accompanying medication guide. This field may contain information about when to consult the medication guide and the contents of the medication guide.Medication Guide Olanzapine Tablets, USP 2.5 mg, 5 mg, 7.5 mg, 10 mg, 15 mg and 20 mg Read the Medication Guide that comes with olanzapine tablets before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking to your doctor about your medical condition or treatment. Talk with your doctor or pharmacist if there is something you do not understand or you want to learn more about olanzapine tablets. What is the most important information I should know about olanzapine tablets? Olanzapine tablets may cause serious side effects, including: • Increased risk of death in elderly people who are confused, have memory loss and have lost touch with reality (dementia-related psychosis). • High blood sugar (hyperglycemia) . • High fat levels in your blood (increased cholesterol and triglycerides), especially in teenagers age 13 to 17. • Weight gain, especially in teenagers age 13 to 17. These serious side effects are described below. • Increased risk of death in elderly people who are confused, have memory loss and have lost touch with reality (dementia-related psychosis). Olanzapine tablets are not approved for treating psychosis in elderly people with dementia. • High blood sugar (hyperglycemia). High blood sugar can happen if you have diabetes already or if you have never had diabetes. High blood sugar could lead to: Your doctor should do tests to check your blood sugar before you start taking olanzapine tablets and during treatment. In people who do not have diabetes, sometimes high blood sugar goes away when olanzapine tablets are stopped. People with diabetes and some people who did not have diabetes before taking olanzapine tablets need to take medicine for high blood sugar even after they stop taking olanzapine tablets. If you have diabetes, follow your doctor’s instructions about how often to check your blood sugar while taking olanzapine tablets. Call your doctor if you have any of these symptoms of high blood sugar (hyperglycemia) while taking olanzapine tablets: • a build up of acid in your blood due to ketones (ketoacidosis) • coma • death • feel very thirsty • need to urinate more than usual • feel very hungry • feel weak or tired • feel sick to your stomach • feel confused, or your breath smells fruity • High fat level in your blood (cholesterol and triglycerides). High fat levels may happen in people treated with olanzapine tablets, especially in teenagers (13 to 17 years old). You may not have any symptoms, so your doctor should do blood tests to check your cholesterol and triglyceride levels before you start taking olanzapine tablets and during treatment. • Weight gain. Weight gain is very common in people who take olanzapine tablets. Teenagers (13 to 17 years old) are more likely to gain weight and to gain more weight than adults. Some people may gain a lot of weight while taking olanzapine tablets, so you and your doctor should check your weight regularly. Talk to your doctor about ways to control weight gain, such as eating a healthy, balanced diet, and exercising. What are olanzapine tablets? Olanzapine tablets are a prescription medicine used to treat: • schizophrenia. • bipolar disorder, including: • manic or mixed episodes that happen with bipolar I disorder. • manic or mixed episodes that happen with bipolar I disorder, when used with the medicine lithium or valproate, in adults. • long-term treatment of bipolar I disorder in adults. • episodes of depression that happen with bipolar I disorder, when used with the medicine fluoxetine (Prozac ® ), in adults. Olanzapine tablets have not been approved for use in children under 13 years of age. The symptoms of schizophrenia include hearing voices, seeing things that are not there, having beliefs that are not true, and being suspicious or withdrawn. The symptoms of bipolar I disorder include alternating periods of depression and high or irritable mood, increased activity and restlessness, racing thoughts, talking fast, impulsive behavior, and a decreased need for sleep. Some of your symptoms may improve with treatment. If you do not think you are getting better, call your doctor. Pediatric use information is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. What should I tell my doctor before taking olanzapine tablets? Olanzapine tablets may not be right for you. Before starting olanzapine tablets, tell your doctor if you have or had: • heart problems • seizures • diabetes or high blood sugar levels (hyperglycemia) • high cholesterol or triglyceride levels in your blood • liver problems • low or high blood pressure • strokes or “mini-strokes” also called transient ischemic attacks (TIAs) • Alzheimer's disease • narrow-angle glaucoma • enlarged prostate in men • bowel obstruction • breast cancer • thoughts of suicide or hurting yourself • any other medical condition • are pregnant or plan to become pregnant. It is not known if olanzapine tablets will harm your unborn baby. • are breast-feeding or plan to breast-feed. Olanzapine can pass into your breast milk and may harm your baby. You should not breast-feed while taking olanzapine tablets. Talk to your doctor about the best way to feed your baby if you take olanzapine tablets. Tell your doctor if you exercise a lot or are in hot places often. The symptoms of bipolar I disorder or schizophrenia may include thoughts of suicide or of hurting yourself or others. If you have these thoughts at any time, tell your doctor or go to an emergency room right away. Tell your doctor about all the medicines that you take, including prescription and nonprescription medicines, vitamins, and herbal supplements. Olanzapine tablets and some medicines may interact with each other and may not work as well, or cause possible serious side effects. Your doctor can tell you if it is safe to take olanzapine tablets with your other medicines. Do not start or stop any medicine while taking olanzapine tablets without talking to your doctor first. How should I take olanzapine tablets? • Take olanzapine tablets exactly as prescribed. Your doctor may need to change (adjust) the dose of olanzapine tablets until it is right for you. • If you miss a dose of olanzapine tablets, take the missed dose as soon as you remember. If it is almost time for the next dose, just skip the missed dose and take your next dose at the regular time. Do not take two doses of olanzapine tablets at the same time. • To prevent serious side effects, do not stop taking olanzapine tablets suddenly. If you need to stop taking olanzapine tablets, your doctor can tell you how to safely stop taking it. • If you take too much olanzapine, call your doctor or poison control center at 1-800-222-1222 right away, or get emergency treatment. • Olanzapine tablets can be taken with or without food. • Olanzapine tablets are usually taken one time each day. • Call your doctor if you do not think you are getting better or have any concerns about your condition while taking olanzapine tablets. What should I avoid while taking olanzapine tablets? • Olanzapine tablets can cause sleepiness and may affect your ability to make decisions, think clearly, or react quickly. You should not drive, operate heavy machinery, or do other dangerous activities until you know how olanzapine tablets affect you. • Avoid drinking alcohol while taking olanzapine tablets. Drinking alcohol while you take olanzapine tablets may make you sleepier than if you take olanzapine tablets alone. What are the possible side effects of olanzapine tablets? Serious side effects may happen when you take olanzapine tablets, including: • See “What is the most important information I should know about olanzapine tablets?”, which describes the increased risk of death in elderly people with dementia-related psychosis and the risks of high blood sugar, high cholesterol and triglyceride levels, and weight gain. • Increased incidence of stroke or “mini-strokes” called transient ischemic attacks (TIAs) in elderly people with dementia-related psychosis (elderly people who have lost touch with reality due to confusion and memory loss). Olanzapine tablets are not approved for these patients. • Neuroleptic Malignant Syndrome (NMS): NMS is a rare but very serious condition that can happen in people who take antipsychotic medicines, including olanzapine tablets. NMS can cause death and must be treated in a hospital. Call your doctor right away if you become severely ill and have any of these symptoms: • high fever • excessive sweating • rigid muscles • confusion • changes in your breathing, heartbeat, and blood pressure. • Tardive Dyskinesia: This condition causes body movements that keep happening and that you can not control. These movements usually affect the face and tongue. Tardive dyskinesia may not go away, even if you stop taking olanzapine tablets. It may also start after you stop taking olanzapine tablets. Tell your doctor if you get any body movements that you can not control. • Decreased blood pressure when you change positions, with symptoms of dizziness, fast or slow heartbeat, or fainting. • Difficulty swallowing, that can cause food or liquid to get into your lungs. • Seizures: Tell your doctor if you have a seizure during treatment with olanzapine tablets. • Problems with control of body temperature: You could become very hot, for instance when you exercise a lot or stay in an area that is very hot. It is important for you to drink water to avoid dehydration. Call your doctor right away if you become severely ill and have any of these symptoms of dehydration: • sweating too much or not at all • dry mouth • feeling very hot • feeling thirsty • not able to produce urine. Common side effects of olanzapine tablets include: lack of energy, dry mouth, increased appetite, sleepiness, tremor (shakes), having hard or infrequent stools, dizziness, changes in behavior, or restlessness. Other common side effects in teenagers (13 to 17 years old) include: headache, stomach-area (abdominal) pain, pain in your arms or legs, or tiredness. Teenagers experienced greater increases in prolactin, liver enzymes, and sleepiness, as compared with adults. Tell your doctor about any side effect that bothers you or that does not go away. These are not all the possible side effects with olanzapine tablets. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store olanzapine tablets? • Store olanzapine tablets at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F). • Keep olanzapine tablets away from light. • Keep olanzapine tablets dry and away from moisture. Keep olanzapine tablets and all medicines out of the reach of children. General information about olanzapine tablets Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use olanzapine tablets for a condition for which it was not prescribed. Do not give olanzapine tablets to other people, even if they have the same condition. It may harm them. This Medication Guide summarizes the most important information about olanzapine tablets. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about olanzapine tablets that was written for healthcare professionals. For more information about olanzapine tablets call Apotex Corp. at 1-800-706-5575 or visit www.apotexcorp.com/products. What are the ingredients in olanzapine tablets? Active ingredient: olanzapine Inactive ingredients: lactose, microcrystalline cellulose, starch, magnesium stearate. The color coating contains hypromellose, hydroxypropyl cellulose, polyethylene glycol, titanium dioxide (all strengths), FD&C Blue No.2 Aluminum Lake (15 mg), or red ferric oxide and yellow iron oxide (20 mg). This Medication Guide has been approved by the U.S. Food and Drug Administration. Symbyax ® is a registered trademark of Eli Lilly and Company. Prozac ® is a registered trademark of Eli Lilly and Company. Manufactured by: Apotex Inc. Toronto, Ontario Canada M9L 1T9 Manufactured for: Apotex Corp. Weston, Florida USA 33326 Repackaged By: Proficient Rx LP Thousand Oaks, CA 91320 Revision 2 Revised: February 2012
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES When using olanzapine tablets and fluoxetine in combination, also refer to the Clinical Studies section of the package insert for Symbyax ® . 14.1 Schizophrenia Adults The efficacy of oral olanzapine in the treatment of schizophrenia was established in 2 short-term (6-week) controlled trials of adult inpatients who met DSM III-R criteria for schizophrenia. A single haloperidol arm was included as a comparative treatment in 1 of the 2 trials, but this trial did not compare these 2 drugs on the full range of clinically relevant doses for both. Several instruments were used for assessing psychiatric signs and symptoms in these studies, among them the Brief Psychiatric Rating Scale (BPRS), a multi-item inventory of general psychopathology traditionally used to evaluate the effects of drug treatment in schizophrenia. The BPRS psychosis cluster (conceptual disorganization, hallucinatory behavior, suspiciousness, and unusual thought content) is considered a particularly useful subset for assessing actively psychotic schizophrenic patients. A second traditional assessment, the Clinical Global Impression (CGI), reflects the impression of a skilled observer, fully familiar with the manifestations of schizophrenia, about the overall clinical state of the patient. In addition, 2 more recently developed scales were employed; these included the 30-item Positive and Negative Symptoms Scale (PANSS), in which are embedded the 18 items of the BPRS, and the Scale for Assessing Negative Symptoms (SANS). The trial summaries below focus on the following outcomes: PANSS total and/or BPRS total; BPRS psychosis cluster; PANSS negative subscale or SANS; and CGI Severity. The results of the trials follow: (1) In a 6-week, placebo-controlled trial (n=149) involving 2 fixed olanzapine doses of 1 and 10 mg/day (once daily schedule), olanzapine, at 10 mg/day (but not at 1 mg/day), was superior to placebo on the PANSS total score (also on the extracted BPRS total), on the BPRS psychosis cluster, on the PANSS Negative subscale, and on CGI Severity. (2) In a 6-week, placebo-controlled trial (n=253) involving 3 fixed dose ranges of olanzapine (5 ± 2.5 mg/day, 10 ± 2.5 mg/day, and 15 ± 2.5 mg/day) on a once daily schedule, the 2 highest olanzapine dose groups (actual mean doses of 12 and 16 mg/day, respectively) were superior to placebo on BPRS total score, BPRS psychosis cluster, and CGI severity score; the highest olanzapine dose group was superior to placebo on the SANS. There was no clear advantage for the high-dose group over the medium-dose group. (3) In a longer-term trial, adult outpatients (n=326) who predominantly met DSM-IV criteria for schizophrenia and who remained stable on olanzapine during open-label treatment for at least 8 weeks were randomized to continuation on their current olanzapine doses (ranging from 10 to 20 mg/day) or to placebo. The follow-up period to observe patients for relapse, defined in terms of increases in BPRS positive symptoms or hospitalization, was planned for 12 months, however, criteria were met for stopping the trial early due to an excess of placebo relapses compared to olanzapine relapses, and olanzapine was superior to placebo on time to relapse, the primary outcome for this study. Thus, olanzapine was more effective than placebo at maintaining efficacy in patients stabilized for approximately 8 weeks and followed for an observation period of up to 8 months. Examination of population subsets (race and gender) did not reveal any differential responsiveness on the basis of these subgroupings. Adolescents Clinical trial information in pediatric patients with schizophrenia is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. 14.2 Bipolar I Disorder (Manic or Mixed Episodes) Adults Monotherapy — The efficacy of oral olanzapine in the treatment of manic or mixed episodes was established in 2 short-term (one 3-week and one 4-week) placebo-controlled trials in adult patients who met the DSM-IV criteria for bipolar I disorder with manic or mixed episodes. These trials included patients with or without psychotic features and with or without a rapid-cycling course. The primary rating instrument used for assessing manic symptoms in these trials was the Young Mania Rating Scale (Y-MRS), an 11-item clinician-rated scale traditionally used to assess the degree of manic symptomatology (irritability, disruptive/aggressive behavior, sleep, elevated mood, speech, increased activity, sexual interest, language/thought disorder, thought content, appearance, and insight) in a range from 0 (no manic features) to 60 (maximum score). The primary outcome in these trials was change from baseline in the Y-MRS total score. The results of the trials follow: (1) In one 3-week placebo-controlled trial (n=67) which involved a dose range of olanzapine (5 to 20 mg/day, once daily, starting at 10 mg/day), olanzapine was superior to placebo in the reduction of Y-MRS total score. In an identically designed trial conducted simultaneously with the first trial, olanzapine demonstrated a similar treatment difference, but possibly due to sample size and site variability, was not shown to be superior to placebo on this outcome. (2) In a 4-week placebo-controlled trial (n=115) which involved a dose range of olanzapine (5 to 20 mg/day, once daily, starting at 15 mg/day), olanzapine was superior to placebo in the reduction of Y-MRS total score. (3) In another trial, 361 patients meeting DSM-IV criteria for a manic or mixed episode of bipolar I disorder who had responded during an initial open-label treatment phase for about 2 weeks, on average, to olanzapine 5 to 20 mg/day were randomized to either continuation of olanzapine at their same dose (n=225) or to placebo (n=136), for observation of relapse. Approximately 50% of the patients had discontinued from the olanzapine group by day 59 and 50% of the placebo group had discontinued by day 23 of double-blind treatment. Response during the open-label phase was defined by having a decrease of the Y-MRS total score to ≤12 and HAM-D 21 to ≤8. Relapse during the double-blind phase was defined as an increase of the Y-MRS or HAM-D 21 total score to ≥15, or being hospitalized for either mania or depression. In the randomized phase, patients receiving continued olanzapine experienced a significantly longer time to relapse. Adjunct to Lithium or Valproate — The efficacy of oral olanzapine with concomitant lithium or valproate in the treatment of manic or mixed episodes was established in 2 controlled trials in patients who met the DSM-IV criteria for bipolar I disorder with manic or mixed episodes. These trials included patients with or without psychotic features and with or without a rapid-cycling course. The results of the trials follow: (1) In one 6-week placebo-controlled combination trial, 175 outpatients on lithium or valproate therapy with inadequately controlled manic or mixed symptoms (Y-MRS ≥16) were randomized to receive either olanzapine or placebo, in combination with their original therapy. Olanzapine (in a dose range of 5 to 20 mg/day, once daily, starting at 10 mg/day) combined with lithium or valproate (in a therapeutic range of 0.6 mEq/L to 1.2 mEq/L or 50 μg/mL to 125 μg/mL, respectively) was superior to lithium or valproate alone in the reduction of Y-MRS total score. (2) In a second 6-week placebo-controlled combination trial, 169 outpatients on lithium or valproate therapy with inadequately controlled manic or mixed symptoms (Y-MRS ≥16) were randomized to receive either olanzapine or placebo, in combination with their original therapy. Olanzapine (in a dose range of 5 to 20 mg/day, once daily, starting at 10 mg/day) combined with lithium or valproate (in a therapeutic range of 0.6 mEq/L to 1.2 mEq/L or 50 μg/mL to 125 μg/mL, respectively) was superior to lithium or valproate alone in the reduction of Y-MRS total score. Adolescents Clinical trial information in pediatric patients with bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use Of the 2500 patients in premarketing clinical studies with oral olanzapine, 11% (263) were 65 years of age or over. In patients with schizophrenia, there was no indication of any different tolerability of olanzapine in the elderly compared to younger patients. Studies in elderly patients with dementia-related psychosis have suggested that there may be a different tolerability profile in this population compared to younger patients with schizophrenia. Elderly patients with dementia-related psychosis treated with olanzapine are at an increased risk of death compared to placebo. In placebo-controlled studies of olanzapine in elderly patients with dementia-related psychosis, there was a higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack) in patients treated with olanzapine compared to patients treated with placebo. Olanzapine is not approved for the treatment of patients with dementia-related psychosis. Also, the presence of factors that might decrease pharmacokinetic clearance or increase the pharmacodynamic response to olanzapine should lead to consideration of a lower starting dose for any geriatric patient [see Boxed Warning , Dosage and Administration ( 2.1 ), and Warnings and Precautions ( 5.1 )] . Clinical studies of olanzapine and fluoxetine in combination did not include sufficient numbers of patients ≥65 years of age to determine whether they respond differently from younger patients.
Labor and delivery
Information about the drug’s use during labor or delivery, whether or not the use is stated in the indications section of the labeling, including the effect of the drug on the mother and fetus, on the duration of labor or delivery, on the possibility of delivery-related interventions, and the effect of the drug on the later growth, development, and functional maturation of the child.8.2 Labor and Delivery The effect of olanzapine on labor and delivery in humans is unknown. Parturition in rats was not affected by olanzapine.
Nursing mothers
Information about excretion of the drug in human milk and effects on the nursing infant, including pertinent adverse effects observed in animal offspring.8.3 Nursing Mothers In a study in lactating, healthy women, olanzapine was excreted in breast milk. Mean infant dose at steady state was estimated to be 1.8% of the maternal olanzapine dose. It is recommended that women receiving olanzapine should not breast-feed.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use Compared to patients from adult clinical trials, adolescents were likely to gain more weight, experience increased sedation, and have greater increases in total cholesterol, triglycerides, LDL cholesterol, prolactin and hepatic transaminase levels [see Warnings and Precautions ( 5.5 , 5.6 , 5.15 , 5.17 ) and Adverse Reactions ( 6.2 )] . When deciding among the alternative treatments available for adolescents, clinicians should consider the increased potential (in adolescents as compared with adults) for weight gain and hyperlipidemia. Safety and effectiveness of olanzapine in children <13 years of age have not been established [see Patient Counseling Information ( 17.13 )] . Safety and effectiveness of olanzapine and fluoxetine in combination in children and adolescents <18 years of age have not been established. Pediatric use information in pediatric patients with schizophrenia and bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Teratogenic Effects, Pregnancy Category C — In oral reproduction studies in rats at doses up to 18 mg/kg/day and in rabbits at doses up to 30 mg/kg/day (9 and 30 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively) no evidence of teratogenicity was observed. In an oral rat teratology study, early resorptions and increased numbers of nonviable fetuses were observed at a dose of 18 mg/kg/day (9 times the maximum recommended human daily oral dose on a mg/m 2 basis). Gestation was prolonged at 10 mg/kg/day (5 times the maximum recommended human daily oral dose on a mg/m 2 basis). In an oral rabbit teratology study, fetal toxicity (manifested as increased resorptions and decreased fetal weight) occurred at a maternally toxic dose of 30 mg/kg/day (30 times the maximum recommended human daily oral dose on a mg/m 2 basis). Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Placental transfer of olanzapine occurs in rat pups. There are no adequate and well-controlled trials with olanzapine in pregnant females. Seven pregnancies were observed during clinical trials with olanzapine, including 2 resulting in normal births, 1 resulting in neonatal death due to a cardiovascular defect, 3 therapeutic abortions, and 1 spontaneous abortion. Nonteratogenic Effects, Class Effect - Extrapyramidal and/or withdrawal symptoms have been reported following delivery in neonates exposed to antipsychotic drugs (including olanzapine), during the third trimester of pregnancy. These reports include: agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder in these neonates. These complications have varied in severity; while in some cases symptoms have been self-limited, in other cases neonates have required intensive care unit support and prolonged hospitalization. Olanzapine tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Teratogenic effects
Pregnancy category A: Adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in the first trimester of pregnancy, and there is no evidence of a risk in later trimesters. Pregnancy category B: Animal reproduction studies have failed to demonstrate a risk to the fetus and there are no adequate and well-controlled studies in pregnant women. Pregnancy category C: Animal reproduction studies have shown an adverse effect on the fetus, there are no adequate and well-controlled studies in humans, and the benefits from the use of the drug in pregnant women may be acceptable despite its potential risks. Pregnancy category D: There is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but the potential benefits from the use of the drug in pregnant women may be acceptable despite its potential risks (for example, if the drug is needed in a life-threatening situation or serious disease for which safer drugs cannot be used or are ineffective). Pregnancy category X: Studies in animals or humans have demonstrated fetal abnormalities or there is positive evidence of fetal risk based on adverse reaction reports from investigational or marketing experience, or both, and the risk of the use of the drug in a pregnant woman clearly outweighs any possible benefit (for example, safer drugs or other forms of therapy are available).Teratogenic Effects, Pregnancy Category C — In oral reproduction studies in rats at doses up to 18 mg/kg/day and in rabbits at doses up to 30 mg/kg/day (9 and 30 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively) no evidence of teratogenicity was observed. In an oral rat teratology study, early resorptions and increased numbers of nonviable fetuses were observed at a dose of 18 mg/kg/day (9 times the maximum recommended human daily oral dose on a mg/m 2 basis). Gestation was prolonged at 10 mg/kg/day (5 times the maximum recommended human daily oral dose on a mg/m 2 basis). In an oral rabbit teratology study, fetal toxicity (manifested as increased resorptions and decreased fetal weight) occurred at a maternally toxic dose of 30 mg/kg/day (30 times the maximum recommended human daily oral dose on a mg/m 2 basis). Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Placental transfer of olanzapine occurs in rat pups. There are no adequate and well-controlled trials with olanzapine in pregnant females. Seven pregnancies were observed during clinical trials with olanzapine, including 2 resulting in normal births, 1 resulting in neonatal death due to a cardiovascular defect, 3 therapeutic abortions, and 1 spontaneous abortion.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS When using olanzapine tablets and fluoxetine in combination, also refer to the Use in Specific Populations section of the package insert for Symbyax ® . • Pregnancy: Olanzapine tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. ( 8.1 ) • Nursing Mothers: Breast-feeding is not recommended. ( 8.3 ) • Pediatric Use: Safety and effectiveness of olanzapine tablets in children <13 years of age have not been established. ( 8.4 ) Information describing the use of olanzapine tablets and olanzapine orally disintegrating tablets in pediatric patients with schizophrenia and bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. 8.1 Pregnancy Teratogenic Effects, Pregnancy Category C — In oral reproduction studies in rats at doses up to 18 mg/kg/day and in rabbits at doses up to 30 mg/kg/day (9 and 30 times the maximum recommended human daily oral dose on a mg/m 2 basis, respectively) no evidence of teratogenicity was observed. In an oral rat teratology study, early resorptions and increased numbers of nonviable fetuses were observed at a dose of 18 mg/kg/day (9 times the maximum recommended human daily oral dose on a mg/m 2 basis). Gestation was prolonged at 10 mg/kg/day (5 times the maximum recommended human daily oral dose on a mg/m 2 basis). In an oral rabbit teratology study, fetal toxicity (manifested as increased resorptions and decreased fetal weight) occurred at a maternally toxic dose of 30 mg/kg/day (30 times the maximum recommended human daily oral dose on a mg/m 2 basis). Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Placental transfer of olanzapine occurs in rat pups. There are no adequate and well-controlled trials with olanzapine in pregnant females. Seven pregnancies were observed during clinical trials with olanzapine, including 2 resulting in normal births, 1 resulting in neonatal death due to a cardiovascular defect, 3 therapeutic abortions, and 1 spontaneous abortion. Nonteratogenic Effects, Class Effect - Extrapyramidal and/or withdrawal symptoms have been reported following delivery in neonates exposed to antipsychotic drugs (including olanzapine), during the third trimester of pregnancy. These reports include: agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder in these neonates. These complications have varied in severity; while in some cases symptoms have been self-limited, in other cases neonates have required intensive care unit support and prolonged hospitalization. Olanzapine tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. 8.2 Labor and Delivery The effect of olanzapine on labor and delivery in humans is unknown. Parturition in rats was not affected by olanzapine. 8.3 Nursing Mothers In a study in lactating, healthy women, olanzapine was excreted in breast milk. Mean infant dose at steady state was estimated to be 1.8% of the maternal olanzapine dose. It is recommended that women receiving olanzapine should not breast-feed. 8.4 Pediatric Use Compared to patients from adult clinical trials, adolescents were likely to gain more weight, experience increased sedation, and have greater increases in total cholesterol, triglycerides, LDL cholesterol, prolactin and hepatic transaminase levels [see Warnings and Precautions ( 5.5 , 5.6 , 5.15 , 5.17 ) and Adverse Reactions ( 6.2 )] . When deciding among the alternative treatments available for adolescents, clinicians should consider the increased potential (in adolescents as compared with adults) for weight gain and hyperlipidemia. Safety and effectiveness of olanzapine in children <13 years of age have not been established [see Patient Counseling Information ( 17.13 )] . Safety and effectiveness of olanzapine and fluoxetine in combination in children and adolescents <18 years of age have not been established. Pediatric use information in pediatric patients with schizophrenia and bipolar I disorder is approved for Eli Lilly and Company’s olanzapine drug product labeling. However, due to Eli Lilly and Company’s marketing exclusivity rights, this drug product is not labeled with that pediatric information. 8.5 Geriatric Use Of the 2500 patients in premarketing clinical studies with oral olanzapine, 11% (263) were 65 years of age or over. In patients with schizophrenia, there was no indication of any different tolerability of olanzapine in the elderly compared to younger patients. Studies in elderly patients with dementia-related psychosis have suggested that there may be a different tolerability profile in this population compared to younger patients with schizophrenia. Elderly patients with dementia-related psychosis treated with olanzapine are at an increased risk of death compared to placebo. In placebo-controlled studies of olanzapine in elderly patients with dementia-related psychosis, there was a higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack) in patients treated with olanzapine compared to patients treated with placebo. Olanzapine is not approved for the treatment of patients with dementia-related psychosis. Also, the presence of factors that might decrease pharmacokinetic clearance or increase the pharmacodynamic response to olanzapine should lead to consideration of a lower starting dose for any geriatric patient [see Boxed Warning , Dosage and Administration ( 2.1 ), and Warnings and Precautions ( 5.1 )] . Clinical studies of olanzapine and fluoxetine in combination did not include sufficient numbers of patients ≥65 years of age to determine whether they respond differently from younger patients.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING 16.1 How Supplied Olanzapine Tablets, USP 2.5 mg are white, round, biconvex film-coated tablets, engraved “APO” on one side, “OLA” over “2.5” on the other side. They are supplied as follows: Bottles of 30s (NDC 63187-453-30) Olanzapine Tablets, USP 10 mg are white, round, biconvex film-coated tablets, engraved “APO” on one side, “OLA” over “10” on the other side. They are supplied as follows: Bottles of 30s (NDC 63187-429-30) 16.2 Storage and Handling Store olanzapine tablets at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. Protect olanzapine tablets from light and moisture.
16.1 How Supplied Olanzapine Tablets, USP 2.5 mg are white, round, biconvex film-coated tablets, engraved “APO” on one side, “OLA” over “2.5” on the other side. They are supplied as follows: Bottles of 30s (NDC 63187-453-30) Olanzapine Tablets, USP 10 mg are white, round, biconvex film-coated tablets, engraved “APO” on one side, “OLA” over “10” on the other side. They are supplied as follows: Bottles of 30s (NDC 63187-429-30)
Storage and handling
Information about safe storage and handling of the drug product.16.2 Storage and Handling Store olanzapine tablets at 20° to 25°C (68° to 77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature]. Protect olanzapine tablets from light and moisture.
Boxed warning
Information about contraindications or serious warnings, particularly those that may lead to death or serious injury.WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Olanzapine tablets are not approved for the treatment of patients with dementia-related psychosis [see Warnings and Precautions ( 5.1 , 5.14 ) and Patient Counseling Information ( 17.2 )] . When using olanzapine tablets and fluoxetine in combination, also refer to the Boxed Warning section of the package insert for Symbyax ® . WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS See full prescribing information for complete boxed warning. • Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Olanzapine tablets are not approved for the treatment of patients with dementia-related psychosis. ( 5.1 , 5.14 , 17.2 ) When using olanzapine tablets and fluoxetine in combination, also refer to the Boxed Warning section of the package insert for Symbyax ® .
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API