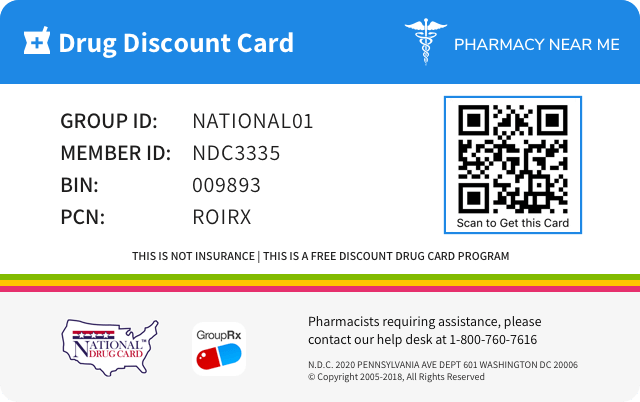
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 72572-440 | ||||
|---|---|---|---|---|---|
| Drug Name | Morphine sulfate |
||||
| Type | Generic | ||||
| Pharm Class | Full Opioid Agonists [MoA], Opioid Agonist [EPC] |
||||
| Active Ingredients |
|
||||
| Route | INTRAVENOUS | ||||
| Dosage Form | INJECTION | ||||
| RxCUI drug identifier | 1732006 | ||||
| Application Number | ANDA205758 | ||||
| Labeler Name | Civica, Inc. | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Drug abuse and dependence
Information about whether the drug is a controlled substance, the types of abuse that can occur with the drug, and adverse reactions pertinent to those types of abuse.9 DRUG ABUSE AND DEPENDENCE 9.1 Controlled Substance Morphine sulfate is a mu-opioid agonist and a Schedule II controlled substance. Morphine sulfate, like other opioids, can be abused and is subject to criminal diversion. 9.2 Abuse Morphine sulfate injection contains a potent narcotic which has been associated with abuse and dependence. Abuse is defined as the intentional non-therapeutic use of a drug, even once, for its rewarding psychological or physiological effects. Due to the risk of overdosage and the risk of its diversion and abuse, it is recommended that special measures be taken to control this product within the hospital or clinic. Morphine sulfate injection should be subject to rigid accounting, rigorous control of wastage and restricted access. “Drug-seeking” behavior is very common in addicts and drug abusers. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing or referral, repeated “loss” of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other treating physician(s). “Doctor shopping” to obtain additional prescriptions is common among drug abusers and people suffering from untreated addiction. Drug addiction is characterized by compulsive use, use for non-medical purposes, and continued use despite harm or risk of harm. Drug addiction is a treatable disease, utilizing a multidisciplinary approach, but relapse is common. Abuse and addiction are separate and distinct from physical dependence and tolerance. Physicians should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence. The converse is also true. In addition, abuse of opioids can occur in the absence of true addiction and is characterized by misuse for non-medical purposes, often in combination with other psychoactive substances. Careful recordkeeping of prescribing information, including quantity, frequency, and renewal requests is strongly advised. Proper assessment of the patient, proper prescribing practices, periodic reevaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs. Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal symptoms. [ See Use in Specific Populations ( 8.2 ) .] 9.3 Dependence Physical dependence is manifested by withdrawal symptoms after abrupt discontinuation of a drug or upon administration of an antagonist. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors) and euphoria. Physical dependence and tolerance are frequent during chronic opioid therapy. The opioid abstinence or withdrawal syndrome is characterized by some or all of the following: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate. Withdrawal symptoms may occur when morphine is discontinued abruptly or upon administration of a narcotic antagonist. In general, taper morphine rather than abruptly discontinue, especially when used for more than a few days.
Overdosage of Morphine Sulfate
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE 10.1 Symptoms Acute overdosage of morphine is characterized by respiratory depression, with or without concomitant CNS depression. In severe overdosage, apnea, circulatory collapse, cardiac arrest and death may occur. Morphine sulfate may cause miosis, even in total darkness. Pinpoint pupils are a sign of opioid overdosage but are not pathognomonic (e.g., pontine lesions of hemorrhagic or ischemic origin may produce similar findings). Marked mydriasis rather than miosis may be seen with hypoxia in overdose situations. 10.2 Treatment Give primary attention to the reestablishment of adequate respiratory exchange through provision of a patent airway and institution of assisted, or controlled, ventilation. Employ supportive measures (including oxygen and vasopressors) in the management of circulatory shock and pulmonary edema accompanying overdose as indicated. Cardiac arrest or arrhythmias may require cardiac massage or defibrillation. The pure opioid antagonist naloxone is a specific antidote to respiratory depression resulting from opioid overdose. Since the duration of reversal is expected to be less than the duration of action of morphine sulfate injection, carefully monitor the patient until spontaneous respiration is reliably reestablished. If the response to opioid antagonists is sub-optimal or only brief in nature, administer additional antagonist as directed by the manufacturer of the product. Do not administer opioid antagonists in the absence of clinically significant respiratory or circulatory depression secondary to morphine sulfate injection overdose. Administer such agents cautiously to persons who are known, or suspected to be physically dependent on morphine sulfate injection. In such cases, an abrupt or complete reversal of opioid effects may precipitate an acute abstinence syndrome. In an individual physically dependent on opioids, administration of the usual dose of the antagonist will precipitate an acute withdrawal syndrome. The severity of the withdrawal symptoms experienced will depend on the degree of physical dependence and the dose of the antagonist administered. Reserve use of an opioid antagonist for cases where such treatment is clearly needed. If it is necessary to treat serious respiratory depression in the physically dependent patient, initiate administration of the antagonist with care and titrate with smaller than usual doses.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS Serious adverse reactions associated with morphine sulfate injection include, respiratory depression, apnea, and to a lesser degree, circulatory depression, respiratory arrest, shock, and cardiac arrest. Rarely, anaphylactoid reactions have been reported when morphine or other phenanthrene alkaloids of opium are administered intravenously. The most frequently observed adverse reactions include sedation, lightheadedness, dizziness, nausea, vomiting, constipation, and diaphoresis. These effects seem to be more prominent in ambulatory patients and in those who are not experiencing severe pain. Some adverse reactions in ambulatory patients may be alleviated if the patient lies down. Other possible adverse reactions include: Central Nervous System – Euphoria, dysphoria, weakness, headache, agitation, tremor, uncoordinated muscle movements, visual disturbances, transient hallucinations and disorientation. Gastrointestinal – Constipation, biliary tract spasm. Cardiovascular – Tachycardia, bradycardia, palpitation, faintness, syncope, and orthostatic hypotension. Genitourinary – Oliguria and urinary retention; an antidiuretic effect has been reported. Allergic – Pruritus, urticaria, and skin rashes. Anaphylactoid reactions have been reported following intravenous administration. Other – Opiate-induced histamine release may be responsible for the flushing of the face, diaphoresis, and pruritus often seen with these drugs. Wheals and urticaria at the site of injection are probably related to histamine release. Local tissue irritation, pain and induration have been reported following repeated subcutaneous injection. Morphine may alter temperature regulation in susceptible individuals and will depress the cough reflex. The most serious adverse reactions encountered are respiratory depression, apnea, circulatory depression, respiratory arrest, shock, and cardiac arrest. Other common frequently observed adverse reactions include: sedation, lightheadedness, dizziness, nausea, vomiting, and constipation. ( 6 ) To report SUSPECTED ADVERSE REACTIONS, contact Hikma Pharmaceuticals USA Inc. at 1-877-845-0689 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .
Morphine Sulfate Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS CNS depressants: May increase the risk of respiratory depression ( 7.1 ) Muscle relaxants: May enhance the neuromuscular blocking action of skeletal muscle relaxants and produce respiratory depression ( 7.2 ) Mixed agonist/antagonist opioid analgesics: May reduce the analgesic effect and/or may precipitate withdrawal symptoms ( 7.3 ) Cimetidine: May increase respiratory and CNS depression ( 7.4 ) Anticholinergics: May increase the risk of urinary retention, severe constipation, or paralytic ileus ( 7.6 ) 7.1 Central Nervous System (CNS) Depressants Morphine should be administered cautiously to avoid additive effects when other central nervous system depressants, including other narcotic analgesics, general anesthetics, phenothiazines, tricyclic antidepressants, tranquilizers, sedatives, hypnotics, antiemetics, and alcohol are given concomitantly. When given concomitantly the risks of respiratory depression, hypotension, profound sedation and coma are increased. 7.2 Muscle Relaxants Morphine sulfate may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. 7.3 Mixed Agonist/Antagonist Opioid Analgesics Do not administer mixed agonist/antagonist analgesics (i.e., pentazocine, nalbuphine, and butorphanol) to patients who have received or are receiving a course of therapy with a pure opioid agonist analgesic such as morphine sulfate injection. In these patients, mixed agonist/antagonist analgesics may reduce the analgesic effect and/or may precipitate withdrawal symptoms. 7.4 Cimetidine Concomitant administration of morphine sulfate injection and cimetidine has been reported to precipitate apnea, confusion, and muscle twitching in an isolated report. Monitor patients for increased respiratory and CNS depression when receiving cimetidine concomitantly with morphine sulfate injection. 7.5 Monoamine Oxidase Inhibitors (MAOIs) MAOIs markedly potentiate the action of morphine sulfate injection. Allow at least 14 days after stopping treatment with MAOIs before initiating treatment with morphine sulfate injection. 7.6 Anticholinergics Anticholinergics or other medications with anticholinergic activity when used concurrently with opioid analgesics may result in increased risk of urinary retention, severe constipation, or paralyltic ileus.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Morphine, a full opioid agonist, is relatively selective for the mu receptor, although it can interact with other opioid receptors at higher doses. In addition to analgesia, the widely diverse effects of morphine sulfate include drowsiness, changes in mood, respiratory depression, decreased gastrointestinal motility, nausea, vomiting, and alterations of the endocrine and autonomic nervous system. Effects on the Central Nervous System (CNS) The principle therapeutic action of morphine is analgesia. Other therapeutic effects of morphine include anxiolysis, euphoria and feelings of relaxation. Although the precise mechanism of the analgesic action is unknown, specific CNS opiate receptors and endogenous compounds with morphine-like activity have been identified throughout the brain and spinal cord and are likely to play a role in the expression and perception of analgesic effects. In common with other opioids, morphine causes respiratory depression, in part by a direct effect on the brainstem respiratory centers. Morphine and related opioids depress the cough reflex by direct effect on the cough center in the medulla. Morphine causes miosis, even in total darkness. Effects on the Gastrointestinal Tract and on Other Smooth Muscle Gastric, biliary and pancreatic secretions are decreased by morphine. Morphine causes a reduction in motility and is associated with an increase in tone in the antrum of the stomach duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone is increased to the point of spasm. The end result may be constipation. Morphine can cause a marked increase in biliary tract pressure as a result of spasm of the sphincter of Oddi. Morphine may also cause spasm of the sphincter of the urinary bladder. Effects of the Cardiovascular System In therapeutic doses, morphine does not usually exert major effects on the cardiovascular system. Morphine produces peripheral vasodilation which may result in orthostatic hypotension and fainting. Release of histamine can occur, which may play a role in opioid-induced hypotension. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, and sweating. Endocrine System Opioid agonists have been shown to have a variety of effects on the secretion of hormones. Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormones (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon in humans and other species, rats and dogs. Thyroid stimulating hormone (TSH) has been shown to be both inhibited and stimulated by opioids. Immune System Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown. 12.2 Pharmacodynamics Morphine concentrations are not predictive of analgesic response, especially in patients previously treated with opioids. The minimum effective concentration varies widely and is influenced by a variety of factors, including the extent of previous opioid use, age and general medical condition. Effective doses in tolerant patients may be significantly higher than in opioid-naïve patients. 12.3 Pharmacokinetics Morphine has an apparent volume of distribution ranging from 1.0 to 4.7 L/kg after parenteral administration. Protein binding is low, about 36%, and muscle tissue binding is reported as 54%. A blood-brain barrier exists, and when morphine is introduced outside of the CNS, plasma concentrations of morphine remain higher than the corresponding CSF morphine levels. Morphine has a total plasma clearance which ranges from 0.9 to 1.2 L/kg/h in postoperative patients, but shows considerable interindividual variation. The major pathway of clearance is hepatic glucuronidation to morphine-3-glucuronide, which is pharmacologically inactive. The major excretion path of the conjugate is through the kidneys, with about 10% in the feces. Morphine is also eliminated by the kidneys, 2 to 12% being excreted unchanged in the urine. Terminal half-life is commonly reported to vary from 1.5 to 4.5 hours, although the longer half-lives were obtained when morphine levels were monitored over protracted periods with very sensitive radioimmunoassay methods. The accepted elimination half-life in normal subjects is 1.5 to 2 hours.
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action Morphine, a full opioid agonist, is relatively selective for the mu receptor, although it can interact with other opioid receptors at higher doses. In addition to analgesia, the widely diverse effects of morphine sulfate include drowsiness, changes in mood, respiratory depression, decreased gastrointestinal motility, nausea, vomiting, and alterations of the endocrine and autonomic nervous system. Effects on the Central Nervous System (CNS) The principle therapeutic action of morphine is analgesia. Other therapeutic effects of morphine include anxiolysis, euphoria and feelings of relaxation. Although the precise mechanism of the analgesic action is unknown, specific CNS opiate receptors and endogenous compounds with morphine-like activity have been identified throughout the brain and spinal cord and are likely to play a role in the expression and perception of analgesic effects. In common with other opioids, morphine causes respiratory depression, in part by a direct effect on the brainstem respiratory centers. Morphine and related opioids depress the cough reflex by direct effect on the cough center in the medulla. Morphine causes miosis, even in total darkness. Effects on the Gastrointestinal Tract and on Other Smooth Muscle Gastric, biliary and pancreatic secretions are decreased by morphine. Morphine causes a reduction in motility and is associated with an increase in tone in the antrum of the stomach duodenum. Digestion of food in the small intestine is delayed and propulsive contractions are decreased. Propulsive peristaltic waves in the colon are decreased, while tone is increased to the point of spasm. The end result may be constipation. Morphine can cause a marked increase in biliary tract pressure as a result of spasm of the sphincter of Oddi. Morphine may also cause spasm of the sphincter of the urinary bladder. Effects of the Cardiovascular System In therapeutic doses, morphine does not usually exert major effects on the cardiovascular system. Morphine produces peripheral vasodilation which may result in orthostatic hypotension and fainting. Release of histamine can occur, which may play a role in opioid-induced hypotension. Manifestations of histamine release and/or peripheral vasodilation may include pruritus, flushing, red eyes, and sweating. Endocrine System Opioid agonists have been shown to have a variety of effects on the secretion of hormones. Opioids inhibit the secretion of ACTH, cortisol, and luteinizing hormones (LH) in humans. They also stimulate prolactin, growth hormone (GH) secretion, and pancreatic secretion of insulin and glucagon in humans and other species, rats and dogs. Thyroid stimulating hormone (TSH) has been shown to be both inhibited and stimulated by opioids. Immune System Opioids have been shown to have a variety of effects on components of the immune system in in vitro and animal models. The clinical significance of these findings is unknown.
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Morphine concentrations are not predictive of analgesic response, especially in patients previously treated with opioids. The minimum effective concentration varies widely and is influenced by a variety of factors, including the extent of previous opioid use, age and general medical condition. Effective doses in tolerant patients may be significantly higher than in opioid-naïve patients.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Morphine has an apparent volume of distribution ranging from 1.0 to 4.7 L/kg after parenteral administration. Protein binding is low, about 36%, and muscle tissue binding is reported as 54%. A blood-brain barrier exists, and when morphine is introduced outside of the CNS, plasma concentrations of morphine remain higher than the corresponding CSF morphine levels. Morphine has a total plasma clearance which ranges from 0.9 to 1.2 L/kg/h in postoperative patients, but shows considerable interindividual variation. The major pathway of clearance is hepatic glucuronidation to morphine-3-glucuronide, which is pharmacologically inactive. The major excretion path of the conjugate is through the kidneys, with about 10% in the feces. Morphine is also eliminated by the kidneys, 2 to 12% being excreted unchanged in the urine. Terminal half-life is commonly reported to vary from 1.5 to 4.5 hours, although the longer half-lives were obtained when morphine levels were monitored over protracted periods with very sensitive radioimmunoassay methods. The accepted elimination half-life in normal subjects is 1.5 to 2 hours.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS Morphine sulfate is contraindicated in patients with known hypersensitivity to morphine. Morphine sulfate is contraindicated in patients with respiratory depression in the absence of resuscitative equipment. Morphine sulfate is contraindicated in patients with acute or severe bronchial asthma or hypercarbia. Morphine sulfate is contraindicated in any patient who has or is suspected of having a paralytic ileus. Known hypersensitivity or allergy to morphine ( 4 ) Bronchial asthma or upper airway obstruction ( 4 ) Respiratory depression in the absence of resuscitative equipment ( 4 ) Paralytic ilieus ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION Morphine is a phenanthrene-derivative opiate agonist. It is the principal alkaloid of opium and is considered to be the prototype of the opiate agonists. Morphine sulfate occurs as white, feathery, silky crystals; cubical masses of crystals; or a white, crystalline powder. When exposed to air it gradually loses water of hydration, and darkens on prolonged exposure to light. It is soluble in water and ethanol at room temperature. The chemical name of morphine sulfate is 7,8-Didehydro-4,5-epoxy-17-methyl-(5α,6α)-morphinan-3,6-diol sulfate (2:1) (salt), pentahydrate, with the following structural formula: (C 17 H 19 NO 3 ) 2 • H 2 SO 4 • 5H 2 O Molecular Weight is 758.83 Morphine sulfate injection, USP is a sterile, nonpyrogenic solution, free of antioxidants and preservatives, intended for intravenous administration. Each milliliter of sterile solution contains 4 mg morphine sulfate and the following inactive ingredients: 0.2 mg edetate disodium, 0.4 mg citric acid monohydrate, sodium chloride to adjust isotonicity and water for injection. Hydrochloric acid and/or sodium hydroxide may be added to adjust pH. The pH range is 2.5 to 4.0. Chemical Structure
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION Morphine sulfate injection is intended for intravenous administration. Direct Intravenous Injection: The usual starting dose in adults is 0.1 mg to 0.2 mg per kg every 4 hours as needed for pain management. The dose should be adjusted according to the severity of pain, the occurrence of adverse events, as well as the patient’s underlying disease, age, and size. ( 2.2 , 2.3 ) 2.1 General Dosing Considerations Morphine sulfate injection is available in three concentrations for direct injection. Take care when prescribing and administering morphine sulfate injection to avoid dosing errors due to confusion between different concentrations and between mg and mL, which could result in accidental overdose and death. Take care to ensure the proper dose is communicated and dispensed. When writing prescriptions, include both the total dose in mg and total dose in volume. Administration of morphine sulfate injection should be limited to use by those familiar with the management of respiratory depression. Morphine must be injected slowly; rapid intravenous administration may result in chest wall rigidity. Selection of patients for treatment with morphine sulfate injection should be governed by the same principles that apply to the use of similar opioid analgesics. Individualize treatment in every case, using non-opioid analgesics, opioids on an as needed basis and/or combination products, and chronic opioid therapy in a progressive plan of pain management such as outlined by the World Health Organization, the Agency for Healthcare Research and Quality, and the American Pain Society. 2.2 Individualization of Dosage Adjust the dosing regimen for each patient individually, taking into account the patient’s prior analgesic treatment experience. In the selection of the initial dose of morphine sulfate injection, give attention to the following: the total daily dose, potency and specific characteristics of the opioid the patient has been taking previously; the reliability of the relative potency estimate used to calculate the equivalent morphine sulfate injection dose needed; the patient’s degree of opioid tolerance; the general condition and medical status of the patient; concurrent medications; the type and severity of the patient’s pain; risk factors for abuse, addiction or diversion, including prior history of abuse, addiction or diversion The following dosing recommendations, therefore, can only be considered suggested approaches to what is actually a series of clinical decisions over time in the management of the pain of each individual patient. Continual reevaluation of the patient receiving morphine sulfate injection is important, with special attention to the management of pain and the relative incidence of side effects associated with therapy. During periods of changing analgesic requirements, including initial titration, frequent contact is recommended between the physician, other members of the healthcare team, the patient, and the caregiver/family. 2.3 Direct Intravenous Injection The usual starting dose in adults is 0.1 mg to 0.2 mg per kg every 4 hours as needed to manage pain. Administer the injection slowly. 2.4 Dosing with Hepatic and Renal Impairment Morphine sulfate pharmacokinetics have been reported to be significantly altered in patients with cirrhosis and renal failure. Start these patients cautiously with lower doses of morphine sulfate injection and titrate slowly while carefully monitoring for side effects. [ See Use in Specific Populations ( 8.7 and 8.8 ) .]
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Single Dose 1 mL Vials: Morphine sulfate injection is available as 4 mg/mL sterile solution in single dose vials for intravenous administration. Morphine sulfate injection, 4 mg/mL is available in 1 mL single dose vials for intravenous administration. ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE Morphine sulfate is an opioid agonist indicated for the management of pain not responsive to non-narcotic analgesics. Morphine sulfate is an opioid agonist indicated for the management of pain not responsive to non-narcotic analgesics.
Spl product data elements
Usually a list of ingredients in a drug product.Morphine Sulfate Morphine Sulfate MORPHINE SULFATE MORPHINE EDETATE DISODIUM CITRIC ACID MONOHYDRATE SODIUM CHLORIDE WATER HYDROCHLORIC ACID SODIUM HYDROXIDE
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis Studies in animals to evaluate the carcinogenic potential of morphine have not been conducted. Mutagenesis No formal studies to assess the mutagenic potential of morphine have been conducted. In the published literature, morphine was found to be mutagenic in vitro increasing DNA fragmentation in human T-cells. Morphine was also reported to be mutagenic in the in vivo mouse micronucleus assay and positive for the induction of chromosomal aberrations in mouse spermatids and murine lymphocytes. Mechanistic studies suggest that the in vivo clastogenic effects reported with morphine in mice may be related to increases in glucocorticoid levels produced by morphine in these species. In contrast to the above positive findings, in vitro studies in the literature have also shown that morphine did not induce chromosomal aberrations in human leukocytes or translocations or lethal mutations in Drosophila . Impairment of Fertility No formal nonclinical studies to assess the potential of morphine to impair fertility have been conducted. Several nonclinical studies from the literature have demonstrated adverse effects on male fertility in the rat from exposure to morphine. One study in which male rats were administered morphine sulfate subcutaneously prior to mating (up to 30 mg/kg twice daily) and during mating (20 mg/kg twice daily) with untreated females, a number of adverse reproductive effects including reduction in total pregnancies, higher incidence of pseudopregnancies, and reduction in implantation sites were seen. Studies from the literature have also reported changes in hormonal levels (i.e. testosterone, luteinizing hormone, serum corticosterone) following treatment with morphine. These changes may be associated with the reported effects on fertility in the rat.
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis Studies in animals to evaluate the carcinogenic potential of morphine have not been conducted. Mutagenesis No formal studies to assess the mutagenic potential of morphine have been conducted. In the published literature, morphine was found to be mutagenic in vitro increasing DNA fragmentation in human T-cells. Morphine was also reported to be mutagenic in the in vivo mouse micronucleus assay and positive for the induction of chromosomal aberrations in mouse spermatids and murine lymphocytes. Mechanistic studies suggest that the in vivo clastogenic effects reported with morphine in mice may be related to increases in glucocorticoid levels produced by morphine in these species. In contrast to the above positive findings, in vitro studies in the literature have also shown that morphine did not induce chromosomal aberrations in human leukocytes or translocations or lethal mutations in Drosophila . Impairment of Fertility No formal nonclinical studies to assess the potential of morphine to impair fertility have been conducted. Several nonclinical studies from the literature have demonstrated adverse effects on male fertility in the rat from exposure to morphine. One study in which male rats were administered morphine sulfate subcutaneously prior to mating (up to 30 mg/kg twice daily) and during mating (20 mg/kg twice daily) with untreated females, a number of adverse reproductive effects including reduction in total pregnancies, higher incidence of pseudopregnancies, and reduction in implantation sites were seen. Studies from the literature have also reported changes in hormonal levels (i.e. testosterone, luteinizing hormone, serum corticosterone) following treatment with morphine. These changes may be associated with the reported effects on fertility in the rat.
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PRINCIPAL DISPLAY PANELS NDC 72572- 440 -01 Morphine Sulfate Inj., USP 4 mg/mL CII For IV use ONLY Protect from light Discard if precipitated 1 mL Single Dose Vial Rx only NDC 72572- 440 -25 Rx Only Morphine Sulfate Injection, USP 4 mg/mL CII For intravenous use only Protect from light 25 x 1 mL Single Dose Vials 462-800-00 462-801-00
SERIALIZATION IMAGE Layout 1
Morphine Sulfate: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Patients receiving parenteral morphine should be given the following instructions by the physician: The most common adverse events that may occur while taking morphine include nausea, somnolence, lightheadedness, dizziness, sedation, vomiting, diaphoresis, and constipation. Morphine analgesics may produce orthostatic hypotension in ambulatory patients. There is potential for severe constipation; appropriate laxatives and/or stool softeners as well as other appropriate treatments should be initiated from the onset of opioid therapy. Analgesic doses of morphine cloud judgment and impair the mental and/or physical abilities which are required for the performance of tasks such as driving a vehicle or operating machinery. Morphine will add to the effect of alcohol and other CNS depressants, including sedatives, hypnotics, tranquilizers, phenothiazines and antihistamines. Mfd for: Civica, Inc. Lehi, Utah 84043 Mfd by: Hikma Pharmaceuticals USA Inc. Cherry Hill, New Jersey 08003 Revised August 2019 462-802-00
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use The pharmacodynamic effects of morphine in the elderly are more variable than in the younger population. Older patients will vary widely in the effective initial dose, rate of development of tolerance and the frequency and magnitude of associated adverse effects as the dose is increased. Initial doses should be based on careful clinical observation following “test doses”, after making due allowances for the effects of the patient’s age and infirmity on his/her ability to clear the drug. Elderly patients may be more susceptible to respiratory depression and/or respiratory arrest following administration of morphine. In general, use caution when selecting a dose for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy.
Labor and delivery
Information about the drug’s use during labor or delivery, whether or not the use is stated in the indications section of the labeling, including the effect of the drug on the mother and fetus, on the duration of labor or delivery, on the possibility of delivery-related interventions, and the effect of the drug on the later growth, development, and functional maturation of the child.8.2 Labor and Delivery Morphine readily passes into the fetal circulation and may result in respiratory depression and psycho-physiologic effects in neonates. Naloxone and resuscitative equipment should be available for reversal of narcotic-induced respiratory depression in the neonate. In addition, parenteral morphine may reduce the strength, duration and frequency of uterine contractions resulting in prolonged labor. However, this effect is not consistent and may be offset by an increased rate of cervical dilatation, which tends to shorten labor. Closely observe neonates whose mothers received opioid analgesics during labor for signs of respiratory depression.
Nursing mothers
Information about excretion of the drug in human milk and effects on the nursing infant, including pertinent adverse effects observed in animal offspring.8.3 Nursing Mothers Low levels of morphine sulfate injection have been detected in maternal milk. The milk:plasma morphine AUC ratio is about 2:5:1. The amount of morphine sulfate injection delivered to the infant depends on the plasma concentration of the mother, the amount of milk ingested by the infant, and the extent of first-pass metabolism. Because of the potential for serious adverse reactions in nursing infants from morphine sulfate injection including respiratory depression, sedation and possibly withdrawal symptoms, upon cessation of morphine sulfate injection administration to the mother, decide whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use The safety and effectiveness of morphine sulfate injection in pediatric patients below the age of 18 have not been established.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Teratogenic Effects (Pregnancy Category C) No formal studies to assess the teratogenic effects of morphine in animals have been conducted. It is also not known whether morphine can cause fetal harm when administered to a pregnant woman or can affect reproductive capacity. Morphine should be given to a pregnant woman only if clearly needed. In humans, the frequency of congenital anomalies have been reported to be no greater than expected among the children of 70 women who were treated with morphine during the first four months of pregnancy or in 448 women treated with morphine anytime during pregnancy. Furthermore, no malformations were observed in the infant of a woman who attempted suicide by taking an overdose of morphine and other medication during the first trimester of pregnancy. Several literature reports indicate that morphine administered subcutaneously during the early gestational period in mice and hamsters produced neurological, soft tissue and skeletal abnormalities. With one exception, the effects that have been reported were following doses that were maternally toxic and the abnormalities noted were characteristic of those observed when maternal toxicity is present. In one study, following subcutaneous infusion of doses greater than or equal to 0.15 mg/kg to mice, exencephaly, hydronephrosis, intestinal hemorrhage, split subpraoccipital, malformed sternebrae, and malformed xiphoid were noted in the absence of maternal toxicity. In the hamster, morphine sulfate given subcutaneously on gestation day 8 produced exencephaly and cranioschisis. In rats treated with subcutaneous infusions of morphine during the period of organogenesis, no teratogenicity was observed. No maternal toxicity was observed in this study, however, increased mortality and growth retardation were seen in the offspring. In two studies performed in the rabbit, no evidence of teratogenicity was reported at subcutaneous doses up to 100 mg/kg. Nonteratogenic Effects Controlled studies of chronic in utero morphine exposure in pregnant women have not been conducted. Infants born to mothers who have taken opioids chronically may exhibit withdrawal symptoms, reversible reduction in brain volume, small size, decreased ventilatory response to CO 2 and increased risk of sudden infant death syndrome. Morphine sulfate should be used by a pregnant woman only if the need for opioid analgesia clearly outweighs the potential risks to the fetus. Published literature has reported that exposure to morphine during pregnancy is associated with reduction in growth and a host of behavioral abnormalities in the offspring of animals. Morphine treatment during gestational periods of organogenesis in rats, hamsters, guinea pigs and rabbits resulted in the following treatment-related embryotoxicity and neonatal toxicity in one or more studies: decreased litter size, embryo-fetal viability, fetal and neonatal body weights, absolute brain and cerebellar weights, delayed motor and sexual maturation, and increased neonatal mortality, cyanosis and hypothermia. Decreased fertility in female offspring, and decreased plasma and testicular levels of luteinizing hormone and testosterone, decreased testes weights, seminiferous tubule shrinkage, germinal cell aplasia, and decreased spermatogenesis in male offspring were also observed. Decreased litter size and viability were observed in the offspring of male rats administered morphine (25 mg/kg, ip) for 1 day prior to mating. Behavioral abnormalities resulting from chronic morphine exposure of fetal animals included altered reflex and motor skill development, mild withdrawal, and altered responsiveness to morphine persisting into adulthood.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS Pregnancy: Based on animal data, may cause fetal harm ( 8.1 ) Pediatric patients: Safety and effectiveness and the pharmacokinetics of morphine sulfate injection in pediatric patients below the age of 18 have not been established. ( 8.4 ) Geriatric patients: Use caution during dose selection, starting at the low end of the dosing range while carefully monitoring for side effects. ( 8.5 ) Renal and hepatic impairment: Start patients at lower doses and titrate cautiously ( 8.7 , 8.8 ) 8.1 Pregnancy Teratogenic Effects (Pregnancy Category C) No formal studies to assess the teratogenic effects of morphine in animals have been conducted. It is also not known whether morphine can cause fetal harm when administered to a pregnant woman or can affect reproductive capacity. Morphine should be given to a pregnant woman only if clearly needed. In humans, the frequency of congenital anomalies have been reported to be no greater than expected among the children of 70 women who were treated with morphine during the first four months of pregnancy or in 448 women treated with morphine anytime during pregnancy. Furthermore, no malformations were observed in the infant of a woman who attempted suicide by taking an overdose of morphine and other medication during the first trimester of pregnancy. Several literature reports indicate that morphine administered subcutaneously during the early gestational period in mice and hamsters produced neurological, soft tissue and skeletal abnormalities. With one exception, the effects that have been reported were following doses that were maternally toxic and the abnormalities noted were characteristic of those observed when maternal toxicity is present. In one study, following subcutaneous infusion of doses greater than or equal to 0.15 mg/kg to mice, exencephaly, hydronephrosis, intestinal hemorrhage, split subpraoccipital, malformed sternebrae, and malformed xiphoid were noted in the absence of maternal toxicity. In the hamster, morphine sulfate given subcutaneously on gestation day 8 produced exencephaly and cranioschisis. In rats treated with subcutaneous infusions of morphine during the period of organogenesis, no teratogenicity was observed. No maternal toxicity was observed in this study, however, increased mortality and growth retardation were seen in the offspring. In two studies performed in the rabbit, no evidence of teratogenicity was reported at subcutaneous doses up to 100 mg/kg. Nonteratogenic Effects Controlled studies of chronic in utero morphine exposure in pregnant women have not been conducted. Infants born to mothers who have taken opioids chronically may exhibit withdrawal symptoms, reversible reduction in brain volume, small size, decreased ventilatory response to CO 2 and increased risk of sudden infant death syndrome. Morphine sulfate should be used by a pregnant woman only if the need for opioid analgesia clearly outweighs the potential risks to the fetus. Published literature has reported that exposure to morphine during pregnancy is associated with reduction in growth and a host of behavioral abnormalities in the offspring of animals. Morphine treatment during gestational periods of organogenesis in rats, hamsters, guinea pigs and rabbits resulted in the following treatment-related embryotoxicity and neonatal toxicity in one or more studies: decreased litter size, embryo-fetal viability, fetal and neonatal body weights, absolute brain and cerebellar weights, delayed motor and sexual maturation, and increased neonatal mortality, cyanosis and hypothermia. Decreased fertility in female offspring, and decreased plasma and testicular levels of luteinizing hormone and testosterone, decreased testes weights, seminiferous tubule shrinkage, germinal cell aplasia, and decreased spermatogenesis in male offspring were also observed. Decreased litter size and viability were observed in the offspring of male rats administered morphine (25 mg/kg, ip) for 1 day prior to mating. Behavioral abnormalities resulting from chronic morphine exposure of fetal animals included altered reflex and motor skill development, mild withdrawal, and altered responsiveness to morphine persisting into adulthood. 8.2 Labor and Delivery Morphine readily passes into the fetal circulation and may result in respiratory depression and psycho-physiologic effects in neonates. Naloxone and resuscitative equipment should be available for reversal of narcotic-induced respiratory depression in the neonate. In addition, parenteral morphine may reduce the strength, duration and frequency of uterine contractions resulting in prolonged labor. However, this effect is not consistent and may be offset by an increased rate of cervical dilatation, which tends to shorten labor. Closely observe neonates whose mothers received opioid analgesics during labor for signs of respiratory depression. 8.3 Nursing Mothers Low levels of morphine sulfate injection have been detected in maternal milk. The milk:plasma morphine AUC ratio is about 2:5:1. The amount of morphine sulfate injection delivered to the infant depends on the plasma concentration of the mother, the amount of milk ingested by the infant, and the extent of first-pass metabolism. Because of the potential for serious adverse reactions in nursing infants from morphine sulfate injection including respiratory depression, sedation and possibly withdrawal symptoms, upon cessation of morphine sulfate injection administration to the mother, decide whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. 8.4 Pediatric Use The safety and effectiveness of morphine sulfate injection in pediatric patients below the age of 18 have not been established. 8.5 Geriatric Use The pharmacodynamic effects of morphine in the elderly are more variable than in the younger population. Older patients will vary widely in the effective initial dose, rate of development of tolerance and the frequency and magnitude of associated adverse effects as the dose is increased. Initial doses should be based on careful clinical observation following “test doses”, after making due allowances for the effects of the patient’s age and infirmity on his/her ability to clear the drug. Elderly patients may be more susceptible to respiratory depression and/or respiratory arrest following administration of morphine. In general, use caution when selecting a dose for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or other drug therapy. 8.6 Gender While evidence of greater post-operative morphine sulfate injection consumption in men compared to women is present in the literature, clinically significant differences in analgesic outcomes and pharmacokinetic parameters have not been consistently demonstrated. Some studies have shown an increased sensitivity to the adverse effects of morphine sulfate injection, including respiratory depression, in women compared to men. 8.7 Hepatic Impairment Morphine sulfate pharmacokinetics have been reported to be significantly altered in patients with cirrhosis. Clearance was found to decrease with a corresponding increase in half-life. The M3G and M6G to morphine AUC ratios also decreased in these subjects, indicating diminished metabolic activity. Start these patients cautiously with lower doses of morphine sulfate injection and titrate slowly while carefully monitoring for side effects. 8.8 Renal Impairment Morphine sulfate pharmacokinetics are altered in patients with renal failure. Clearance is decreased and the metabolites, M3G and M6G, may accumulate to much higher plasma levels in patients with renal failure as compared to patients with normal renal function. Start these patients cautiously with lower doses of morphine sulfate injection and titrate slowly while carefully monitoring for side effects.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING Morphine sulfate injection, USP is supplied in single-dose 1 mL vials for intravenous administration: 4 mg/mL packaged in 25s (NDC 72572-440-25) Store at 20ºC to 25°C (68°F to 77°F) [See USP Controlled Room Temperature] until ready to use. PROTECT FROM LIGHT . DO NOT FREEZE . Contains no preservative or antioxidant. DISCARD ANY UNUSED PORTION. DO NOT HEAT-STERILIZE. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if color is darker than pale yellow, if it is discolored in any other way, or if it contains a precipitate. To report SUSPECTED ADVERSE REACTIONS, contact Hikma Pharmaceuticals USA Inc. at 1-877-845-0689, or the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch . For Product Inquiry call 1-877-845-0689.
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API