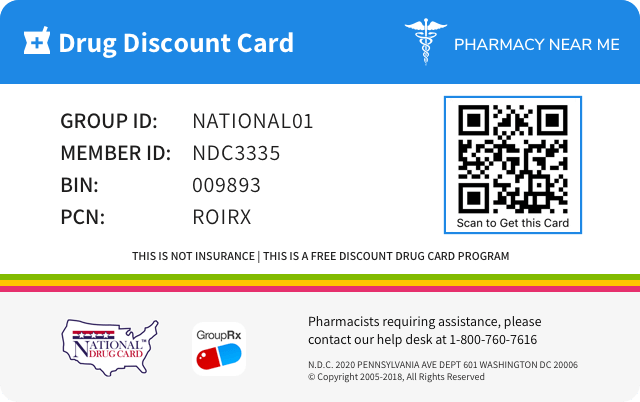
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 68682-299 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug Name | Loteprednol etabonate |
||||||||
| Type | Generic | ||||||||
| Pharm Class | Corticosteroid Hormone Receptor Agonists [MoA], Corticosteroid [EPC] |
||||||||
| Active Ingredients |
|
||||||||
| Route | OPHTHALMIC | ||||||||
| Dosage Form | SUSPENSION/ DROPS | ||||||||
| RxCUI drug identifier | 311382 | ||||||||
| Application Number | NDA020583 | ||||||||
| Labeler Name | Oceanside Pharmaceuticals | ||||||||
| Packages |
|
||||||||
| Check if available Online | Get Medication Prices online with Discount |
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.ADVERSE REACTIONS Reactions associated with ophthalmic steroids include elevated intraocular pressure, which may be associated with optic nerve damage, visual acuity and field defects, posterior subcapsular cataract formation, secondary ocular infection from pathogens including herpes simplex, and perforation of the globe where there is thinning of the cornea or sclera. Ocular adverse reactions occurring in 5%-15% of patients treated with loteprednol etabonate ophthalmic suspension (0.2%-0.5%) in clinical studies included abnormal vision/blurring, burning on instillation, chemosis, discharge, dry eyes, epiphora, foreign body sensation, itching, injection, and photophobia. Other ocular adverse reactions occurring in less than 5% of patients include conjunctivitis, corneal abnormalities, eyelid erythema, keratoconjunctivitis, ocular irritation/pain/discomfort, papillae, and uveitis. Some of these events were similar to the underlying ocular disease being studied. Non-ocular adverse reactions occurred in less than 15% of patients. These include headache, rhinitis and pharyngitis. In a summation of controlled, randomized studies of individuals treated for 28 days or longer with loteprednol etabonate, the incidence of significant elevation of intraocular pressure (≥10 mmHg) was 2% (15/901) among patients receiving loteprednol etabonate, 7% (11/164) among patients receiving 1% prednisolone acetate and 0.5% (3/583) among patients receiving placebo. To report SUSPECTED ADVERSE REACTIONS, contact Oceanside Pharmaceuticals at 1-800-321-4576 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.CLINICAL PHARMACOLOGY Corticosteroids inhibit the inflammatory response to a variety of inciting agents and probably delay or slow healing. They inhibit the edema, fibrin deposition, capillary dilation, leukocyte migration, capillary proliferation, fibroblast proliferation, deposition of collagen, and scar formation associated with inflammation. There is no generally accepted explanation for the mechanism of action of ocular corticosteroids. However, corticosteroids are thought to act by the induction of phospholipase A 2 inhibitory proteins, collectively called lipocortins. It is postulated that these proteins control the biosynthesis of potent mediators of inflammation such as prostaglandins and leukotrienes by inhibiting the release of their common precursor arachidonic acid. Arachidonic acid is released from membrane phospholipids by phospholipase A 2 . Corticosteroids are capable of producing a rise in intraocular pressure (IOP). Loteprednol etabonate is structurally similar to other corticosteroids. However, the number 20 position ketone group is absent. It is highly lipid soluble which enhances its penetration into cells. Loteprednol etabonate is synthesized through structural modifications of prednisolone-related compounds so that it will undergo a predictable transformation to an inactive metabolite. Based upon in vivo and in vitro preclinical metabolism studies, loteprednol etabonate undergoes extensive metabolism to inactive carboxylic acid metabolites. Results from a bioavailability study in normal volunteers established that plasma levels of loteprednol etabonate and Δ 1 cortienic acid etabonate (PJ 91), its primary, inactive metabolite, were below the limit of quantitation (1 ng/mL) at all sampling times. The results were obtained following the ocular administration of one drop in each eye of 0.5% loteprednol etabonate 8 times daily for 2 days or 4 times daily for 42 days. This study suggests that limited (<1 ng/mL) systemic absorption occurs with loteprednol etabonate. Clinical Studies: Post-Operative Inflammation: Placebo-controlled clinical studies demonstrated that loteprednol etabonate is effective for the treatment of anterior chamber inflammation as measured by cell and flare. Giant Papillary Conjunctivitis: Placebo-controlled clinical studies demonstrated that loteprednol etabonate was effective in reducing the signs and symptoms of giant papillary conjunctivitis after 1 week of treatment and continuing for up to 6 weeks while on treatment. Seasonal Allergic Conjunctivitis: A placebo-controlled clinical study demonstrated that loteprednol etabonate was effective in reducing the signs and symptoms of allergic conjunctivitis during peak periods of pollen exposure. Uveitis: Controlled clinical studies of patients with uveitis demonstrated that loteprednol etabonate was less effective than prednisolone acetate 1%. Overall, 72% of patients treated with loteprednol etabonate experienced resolution of anterior chamber cell by day 28, compared to 87% of patients treated with 1% prednisolone acetate. The incidence of patients with clinically significant increases in IOP (≥10 mmHg) was 1% with loteprednol etabonate and 6% with prednisolone acetate 1%.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.CONTRAINDICATIONS Loteprednol etabonate, as with other ophthalmic corticosteroids, is contraindicated in most viral diseases of the cornea and conjunctiva including epithelial herpes simplex keratitis (dendritic keratitis), vaccinia, and varicella, and also in mycobacterial infection of the eye and fungal diseases of ocular structures. Loteprednol etabonate is also contraindicated in individuals with known or suspected hypersensitivity to any of the ingredients of this preparation and to other corticosteroids.
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.DESCRIPTION Loteprednol etabonate ophthalmic suspension contains a sterile, topical anti-inflammatory corticosteroid for ophthalmic use. Loteprednol etabonate is a white to off-white powder. Loteprednol etabonate is represented by the following structural formula: C 24 H 31 ClO 7 Mol. Wt. 466.96 Chemical Name: chloromethyl 17α-[(ethoxycarbonyl)oxy]-11β-hydroxy-3-oxoandrosta-1,4-diene-17β-carboxylate Each mL contains ACTIVE: Loteprednol Etabonate 5 mg (0.5%); INACTIVES: Edetate Disodium, Glycerin, Povidone, Purified Water and Tyloxapol. Hydrochloric Acid and/or Sodium Hydroxide may be added to adjust the pH. The suspension is essentially isotonic with a tonicity of 250 to 310 mOsmol/kg. PRESERVATIVE ADDED: Benzalkonium Chloride 0.01%. Loteprednol etabonate (Structural formula)
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.DOSAGE AND ADMINISTRATION SHAKE VIGOROUSLY BEFORE USING. Steroid-Responsive Disease Treatment: Apply one to two drops of loteprednol etabonate suspension into the conjunctival sac of the affected eye four times daily. During the initial treatment within the first week, the dosing may be increased, up to 1 drop every hour, if necessary. Care should be taken not to discontinue therapy prematurely. If signs and symptoms fail to improve after two days, the patient should be re-evaluated (see PRECAUTIONS ). Post-Operative Inflammation: Apply one to two drops of loteprednol etabonate suspension into the conjunctival sac of the operated eye four times daily beginning 24 hours after surgery and continuing throughout the first 2 weeks of the post-operative period.
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.INDICATIONS AND USAGE Loteprednol etabonate ophthalmic suspension is indicated for the treatment of steroid-responsive inflammatory conditions of the palpebral and bulbar conjunctiva, cornea and anterior segment of the globe such as allergic conjunctivitis, acne rosacea, superficial punctate keratitis, herpes zoster keratitis, iritis, cyclitis, selected infective conjunctivitides, when the inherent hazard of steroid use is accepted to obtain an advisable diminution in edema and inflammation. Loteprednol etabonate is less effective than prednisolone acetate 1% in two 28-day controlled clinical studies in acute anterior uveitis, where 72% of patients treated with loteprednol etabonate experienced resolution of anterior chamber cells, compared to 87% of patients treated with prednisolone acetate 1%. The incidence of patients with clinically significant increases in IOP (≥10 mmHg) was 1% with loteprednol etabonate and 6% with prednisolone acetate 1%. Loteprednol etabonate should not be used in patients who require a more potent corticosteroid for this indication. Loteprednol etabonate ophthalmic suspension is also indicated for the treatment of post-operative inflammation following ocular surgery.
Spl product data elements
Usually a list of ingredients in a drug product.Loteprednol Etabonate loteprednol etabonate LOTEPREDNOL ETABONATE LOTEPREDNOL BENZALKONIUM CHLORIDE EDETATE DISODIUM GLYCERIN WATER TYLOXAPOL HYDROCHLORIC ACID SODIUM HYDROXIDE POVIDONE, UNSPECIFIED
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.Carcinogenesis, Mutagenesis, Impairment of Fertility: Long-term animal studies have not been conducted to evaluate the carcinogenic potential of loteprednol etabonate. Loteprednol etabonate was not genotoxic in vitro in the Ames test, the mouse lymphoma tk assay, or in a chromosome aberration test in human lymphocytes, or in vivo in the single dose mouse micronucleus assay. Treatment of male and female rats with up to 50 mg/kg/day and 25 mg/kg/day of loteprednol etabonate, respectively, (600 and 300 times the maximum clinical dose, respectively) prior to and during mating did not impair fertility in either gender.
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.Principal Display Panel NDC 68682-299-15 Rx only Loteprednol Etabonate Ophthalmic Suspension 0.5% (Sterile) For Ophthalmic Use Only 15 mL Oceanside Pharmaceuticals carton
Spl unclassified section
Information not classified as belonging to one of the other fields. Approximately 40% of labeling with effective_time between June 2009 and August 2014 have information in this field.STERILE OPHTHALMIC SUSPENSION Rx only
Storage: Store upright between 15°to 25°C (59°to77°F). DO NOT FREEZE Keep out of reach of children.
Distributed by: Oceanside Pharmaceuticals, a division of Bausch Health US, LLC, Bridgewater, NJ 08807 USA Manufactured by: Bausch & Lomb Incorporated, Tampa, FL 33637 USA © 2020 Bausch Health Companies Inc. or its affiliates. Revised: May 2020 9646401 (Folded) 9646501 (Flat)
loteprednol etabonate: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.Information for Patients: This product is sterile when packaged. Patients should be advised not to allow the dropper tip to touch any surface, as this may contaminate the suspension. If pain develops, redness, itching or inflammation becomes aggravated, the patient should be advised to consult a physician. As with all ophthalmic preparations containing benzalkonium chloride, patients should be advised not to wear soft contact lenses when using loteprednol etabonate suspension.
Nursing mothers
Information about excretion of the drug in human milk and effects on the nursing infant, including pertinent adverse effects observed in animal offspring.Nursing Mothers: It is not known whether topical ophthalmic administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk. Systemic steroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. Caution should be exercised when loteprednol etabonate is administered to a nursing woman.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.Pediatric Use: Safety and effectiveness in pediatric patients have not been established.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)Pregnancy: Teratogenic effects: Loteprednol etabonate has been shown to be embryotoxic (delayed ossification) and teratogenic (increased incidence of meningocele, abnormal left common carotid artery, and limb flexures) when administered orally to rabbits during organogenesis at a dose of 3 mg/kg/day (35 times the maximum daily clinical dose), a dose which caused no maternal toxicity. The no-observed-effect-level (NOEL) for these effects was 0.5 mg/kg/day (6 times the maximum daily clinical dose). Oral treatment of rats during organogenesis resulted in teratogenicity (absent innominate artery at ≥5 mg/kg/day doses, and cleft palate and umbilical hernia at ≥50 mg/kg/day) and embryotoxicity (increased post-implantation losses at 100 mg/kg/day and decreased fetal body weight and skeletal ossification with ≥50 mg/kg/day). Treatment of rats with 0.5 mg/kg/day (6 times the maximum clinical dose) during organogenesis did not result in any reproductive toxicity. Loteprednol etabonate was maternally toxic (significantly reduced body weight gain during treatment) when administered to pregnant rats during organogenesis at doses of ≥5 mg/kg/day. Oral exposure of female rats to 50 mg/kg/day of loteprednol etabonate from the start of the fetal period through the end of lactation, a maternally toxic treatment regimen (significantly decreased body weight gain), gave rise to decreased growth and survival, and retarded development in the offspring during lactation; the NOEL for these effects was 5 mg/kg/day. Loteprednol etabonate had no effect on the duration of gestation or parturition when administered orally to pregnant rats at doses up to 50 mg/kg/day during the fetal period.
Teratogenic effects
Pregnancy category A: Adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in the first trimester of pregnancy, and there is no evidence of a risk in later trimesters. Pregnancy category B: Animal reproduction studies have failed to demonstrate a risk to the fetus and there are no adequate and well-controlled studies in pregnant women. Pregnancy category C: Animal reproduction studies have shown an adverse effect on the fetus, there are no adequate and well-controlled studies in humans, and the benefits from the use of the drug in pregnant women may be acceptable despite its potential risks. Pregnancy category D: There is positive evidence of human fetal risk based on adverse reaction data from investigational or marketing experience or studies in humans, but the potential benefits from the use of the drug in pregnant women may be acceptable despite its potential risks (for example, if the drug is needed in a life-threatening situation or serious disease for which safer drugs cannot be used or are ineffective). Pregnancy category X: Studies in animals or humans have demonstrated fetal abnormalities or there is positive evidence of fetal risk based on adverse reaction reports from investigational or marketing experience, or both, and the risk of the use of the drug in a pregnant woman clearly outweighs any possible benefit (for example, safer drugs or other forms of therapy are available).Loteprednol etabonate has been shown to be embryotoxic (delayed ossification) and teratogenic (increased incidence of meningocele, abnormal left common carotid artery, and limb flexures) when administered orally to rabbits during organogenesis at a dose of 3 mg/kg/day (35 times the maximum daily clinical dose), a dose which caused no maternal toxicity. The no-observed-effect-level (NOEL) for these effects was 0.5 mg/kg/day (6 times the maximum daily clinical dose). Oral treatment of rats during organogenesis resulted in teratogenicity (absent innominate artery at ≥5 mg/kg/day doses, and cleft palate and umbilical hernia at ≥50 mg/kg/day) and embryotoxicity (increased post-implantation losses at 100 mg/kg/day and decreased fetal body weight and skeletal ossification with ≥50 mg/kg/day). Treatment of rats with 0.5 mg/kg/day (6 times the maximum clinical dose) during organogenesis did not result in any reproductive toxicity. Loteprednol etabonate was maternally toxic (significantly reduced body weight gain during treatment) when administered to pregnant rats during organogenesis at doses of ≥5 mg/kg/day. Oral exposure of female rats to 50 mg/kg/day of loteprednol etabonate from the start of the fetal period through the end of lactation, a maternally toxic treatment regimen (significantly decreased body weight gain), gave rise to decreased growth and survival, and retarded development in the offspring during lactation; the NOEL for these effects was 5 mg/kg/day. Loteprednol etabonate had no effect on the duration of gestation or parturition when administered orally to pregnant rats at doses up to 50 mg/kg/day during the fetal period.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.HOW SUPPLIED Loteprednol etabonate ophthalmic suspension is supplied in a plastic bottle with a controlled drop tip in the following sizes: NDC 68682-299-05 5 mL NDC 68682-299-10 10 mL NDC 68682-299-15 15 mL DO NOT USE IF NECKBAND IMPRINTED WITH "Protective Seal" AND YELLOW IS NOT INTACT. symbol
General precautions
Information about any special care to be exercised for safe and effective use of the drug.General: For ophthalmic use only. The initial prescription and renewal of the medication order beyond 14 days should be made by a physician only after examination of the patient with the aid of magnification, such as slit lamp biomicroscopy and, where appropriate, fluorescein staining. If signs and symptoms fail to improve after two days, the patient should be re-evaluated. If this product is used for 10 days or longer, intraocular pressure should be monitored even though it may be difficult in children and uncooperative patients (see WARNINGS ). Fungal infections of the cornea are particularly prone to develop coincidentally with long-term local steroid application. Fungus invasion must be considered in any persistent corneal ulceration where a steroid has been used or is in use. Fungal cultures should be taken when appropriate.
Precautions
Information about any special care to be exercised for safe and effective use of the drug.PRECAUTIONS General: For ophthalmic use only. The initial prescription and renewal of the medication order beyond 14 days should be made by a physician only after examination of the patient with the aid of magnification, such as slit lamp biomicroscopy and, where appropriate, fluorescein staining. If signs and symptoms fail to improve after two days, the patient should be re-evaluated. If this product is used for 10 days or longer, intraocular pressure should be monitored even though it may be difficult in children and uncooperative patients (see WARNINGS ). Fungal infections of the cornea are particularly prone to develop coincidentally with long-term local steroid application. Fungus invasion must be considered in any persistent corneal ulceration where a steroid has been used or is in use. Fungal cultures should be taken when appropriate. Information for Patients: This product is sterile when packaged. Patients should be advised not to allow the dropper tip to touch any surface, as this may contaminate the suspension. If pain develops, redness, itching or inflammation becomes aggravated, the patient should be advised to consult a physician. As with all ophthalmic preparations containing benzalkonium chloride, patients should be advised not to wear soft contact lenses when using loteprednol etabonate suspension. Carcinogenesis, Mutagenesis, Impairment of Fertility: Long-term animal studies have not been conducted to evaluate the carcinogenic potential of loteprednol etabonate. Loteprednol etabonate was not genotoxic in vitro in the Ames test, the mouse lymphoma tk assay, or in a chromosome aberration test in human lymphocytes, or in vivo in the single dose mouse micronucleus assay. Treatment of male and female rats with up to 50 mg/kg/day and 25 mg/kg/day of loteprednol etabonate, respectively, (600 and 300 times the maximum clinical dose, respectively) prior to and during mating did not impair fertility in either gender. Pregnancy: Teratogenic effects: Loteprednol etabonate has been shown to be embryotoxic (delayed ossification) and teratogenic (increased incidence of meningocele, abnormal left common carotid artery, and limb flexures) when administered orally to rabbits during organogenesis at a dose of 3 mg/kg/day (35 times the maximum daily clinical dose), a dose which caused no maternal toxicity. The no-observed-effect-level (NOEL) for these effects was 0.5 mg/kg/day (6 times the maximum daily clinical dose). Oral treatment of rats during organogenesis resulted in teratogenicity (absent innominate artery at ≥5 mg/kg/day doses, and cleft palate and umbilical hernia at ≥50 mg/kg/day) and embryotoxicity (increased post-implantation losses at 100 mg/kg/day and decreased fetal body weight and skeletal ossification with ≥50 mg/kg/day). Treatment of rats with 0.5 mg/kg/day (6 times the maximum clinical dose) during organogenesis did not result in any reproductive toxicity. Loteprednol etabonate was maternally toxic (significantly reduced body weight gain during treatment) when administered to pregnant rats during organogenesis at doses of ≥5 mg/kg/day. Oral exposure of female rats to 50 mg/kg/day of loteprednol etabonate from the start of the fetal period through the end of lactation, a maternally toxic treatment regimen (significantly decreased body weight gain), gave rise to decreased growth and survival, and retarded development in the offspring during lactation; the NOEL for these effects was 5 mg/kg/day. Loteprednol etabonate had no effect on the duration of gestation or parturition when administered orally to pregnant rats at doses up to 50 mg/kg/day during the fetal period. Nursing Mothers: It is not known whether topical ophthalmic administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk. Systemic steroids appear in human milk and could suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. Caution should be exercised when loteprednol etabonate is administered to a nursing woman. Pediatric Use: Safety and effectiveness in pediatric patients have not been established.
Warnings
Information about serious adverse reactions and potential safety hazards, including limitations in use imposed by those hazards and steps that should be taken if they occur.WARNINGS Prolonged use of corticosteroids may result in glaucoma with damage to the optic nerve, defects in visual acuity and fields of vision, and in posterior subcapsular cataract formation. Steroids should be used with caution in the presence of glaucoma. Prolonged use of corticosteroids may suppress the host response and thus increase the hazard of secondary ocular infections. In those diseases causing thinning of the cornea or sclera, perforations have been known to occur with the use of topical steroids. In acute purulent conditions of the eye, steroids may mask infection or enhance existing infection. Use of ocular steroids may prolong the course and may exacerbate the severity of many viral infections of the eye (including herpes simplex). Employment of a corticosteroid medication in the treatment of patients with a history of herpes simplex requires great caution. The use of steroids after cataract surgery may delay healing and increase the incidence of bleb formation.
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API