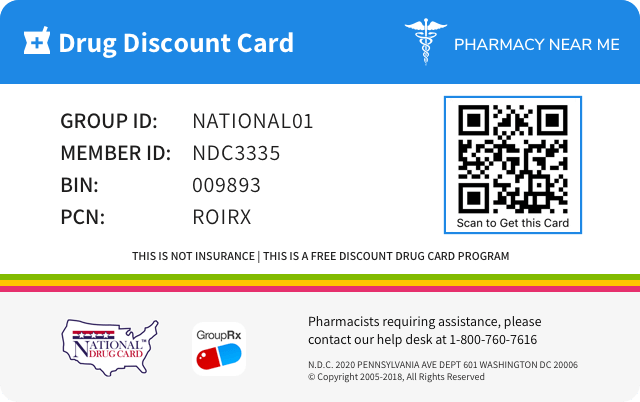
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 68462-427 | ||||
|---|---|---|---|---|---|
| Drug Name | Fluticasone propionate |
||||
| Type | Generic | ||||
| Pharm Class | Corticosteroid Hormone Receptor Agonists [MoA], Corticosteroid [EPC] |
||||
| Active Ingredients |
|
||||
| Route | TOPICAL | ||||
| Dosage Form | LOTION | ||||
| RxCUI drug identifier | 895990 | ||||
| Application Number | ANDA090759 | ||||
| Labeler Name | Glenmark Pharmaceuticals Inc., USA | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS The following adverse reactions are discussed in greater detail in other sections of the labeling: • HPA Axis Suppression and Other Adverse Endocrine Effects [see Warnings and Precautions ( Error! Hyperlink reference not valid. )]. • Local Adverse Reactions [see Warnings and Precautions ( Error! Hyperlink reference not valid. )]. • Concomitant Skin Infections [see Warnings and Precautions ( Error! Hyperlink reference not valid. )]. The most common adverse reactions (2%) were burning/stinging at the application site. ( 6.1 ) To report SUSPECTED ADVERSE REACTIONS, contact Glenmark Pharmaceuticals Inc., USA at 1 (888) 721-7115 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. 6.1 Clinical Trials Experience: Controlled Clinical Trials Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. In 2 multicenter vehicle-controlled clinical trials of once-daily application of fluticasone propionate lotion by 196 adult and 242 pediatric patients, the total incidence of adverse reactions considered drug related by investigators was approximately 4%. These were local cutaneous reactions, usually mild and self-limiting, and consisted primarily of burning/stinging (2%). All other drug-related events occurred with an incidence of less than 1%, and included were contact dermatitis, exacerbation of atopic dermatitis, folliculitis of legs, pruritus, pustules on arm, rash, and skin infection. See Table 1. The incidence of adverse reactions between the 242 pediatric subjects (age 3 months to < 17 years) and 196 adult subjects (17 years or older) was similar (4% and 5%, respectively). Table 1: Adverse Reactions from Controlled Clinical Trials (n=438) ADVERSE REACTIONS Fluticasone Propionate Lotion VEHICLE n=221 n=217 Burning/Stinging skin 4 (2%) 3 (1%) Contact Dermatitis 0 1 (<1%) Exacerbation of Atopic dermatitis 0 1 (<1%) Folliculitis of legs 2 (<1%) 0 Irritant Contact Dermatitis 0 1 (<1%) Pruritus 1 (<1%) 1 (<1%) Pustules on Arms 1 (<1%) 0 Rash 1 (<1%) 2 (<1%) Skin Infection 0 3 (1%) During the clinical trials, eczema herpeticum occurred in a 33-year old male patient treated with fluticasone propionate lotion. Table 2 summarizes all adverse events by body system that occurred in at least 1% of patients in either the drug or vehicle group in the phase 3 controlled clinical trials. Table 2: Adverse Events Occurring in ≥ 1% of Patients from Either Arm from Controlled Clinical Trials (n=438) Body System Fluticasone propionate lotion Vehicle Lotion N = 221 N = 217 Any Adverse Event 77 (35%) 82 (38%) Skin Burning and Stinging 4 (2%) 3 (1%) Pruritus 3 (1%) 5 (2%) Rash 2 (<1%) 3 (1%) Skin Infection 0 3 (1%) Ear, Nose, Throat Common Cold 9 (4%) 5 (2%) Ear Infection 3 (1%) 3 (1%) Nasal Sinus Infection 2 (<1%) 4 (2%) Rhinitis 1 (<1%) 3 (1%) Upper Respiratory Tract Infection 6 (3%) 7 (3%) Gastrointestinal Normal Tooth Eruption 2 (< 1%) 3 (1%) Diarrhea 3 (1%) 0 Vomiting 3 (1%) 2 (<1%) Lower Respiratory Cough 7 (3%) 6 (3%) Influenza 5 (2%) 0 Wheeze 0 3 (1%) Neurology Headache 4 (2%) 5 (2%) Non-Site Specific Fever 8 (4%) 8 (4%) Seasonal Allergy 2 (<1%) 3 (1%) 6.2 Clinical Trials Experience: Pediatric Open Label Trials In an open label HPA axis suppression trial of 44 pediatric subjects (ages ≥3 months to ≤6 years) fluticasone propionate lotion was applied twice daily (rather than the indicated dosing regimen of once daily) to at least 35% of body surface area for 3 or 4 weeks. Subjects whose lesions cleared after 2 or 3 weeks of treatment continued to apply fluticasone propionate lotion for an additional week. The overall incidence of adverse reactions was 14%. These were local, cutaneous reactions and included dry skin (7%), stinging at application site (5%), and excoriation (2%). Additionally, a 4-month-old patient treated with fluticasone propionate lotion had marked elevations of the hepatic enzymes AST and ALT. [see Use in Specific Populations ( 8.4 )] In another open label HPA axis suppression trial in which fluticasone propionate lotion was also applied twice daily (rather than the indicated dosing regimen of once daily), 56 pediatric subjects (ages ≥3 months to 12 months), were enrolled [see Use in Specific Populations ( 8.4 )] . The adverse reactions included 2 cases of Herpes simplex at the application site (3.6%) and 3 cases of bacterial skin infections (5.4%). 6.3Postmarketing Experience The following local adverse reactions have been identified during post-approval use of fluticasone propionate lotion: erythema, edema/swelling, and bleeding. The following systemic adverse reactions have been identified during post-approval use of fluticasone propionate cream and fluticasone propionate ointment: immunosuppression/ Pneumocystis jirovecii pneumonia/leukopenia/ thrombocytopenia; hyperglycemia/glycosuria; Cushing syndrome; generalized body edema/blurred vision; and acute urticarial reaction (edema, urticaria, pruritus, and throat swelling). The following local adverse reactions have also been reported with the use of topical corticosteroids, and they may occur more frequently with the use of occlusive dressings or higher potency corticosteroids. These reactions include: acneiform eruptions, hypopigmentation, perioral dermatitis, skin atrophy, striae, hypertrichosis and miliaria. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Corticosteroids play a role in cellular signaling, immune function, inflammation, and protein regulation; however, the precise mechanism of action of fluticasone propionate lotion in atopic dermatitis is unknown. 12.2 Pharmacodynamics Vasoconstrictor Assay Trials performed with fluticasone propionate lotion indicate that it is in the medium range of potency as demonstrated in vasoconstrictor trials in healthy subjects when compared with other topical corticosteroids. However, similar blanching scores do not necessarily imply therapeutic equivalence. Hypothalamic-Pituitary-Adrenal (HPA) Axis Suppression In an open label HPA axis suppression trial (Trial A), 42 pediatric subjects (ages 4 months to <6 years) with moderate to severe atopic dermatitis covering ≥ 35% Body Surface Area (BSA) who were treated with an exaggerated dosing regimen of fluticasone propionate lotion twice daily (rather than the indicated dosing regimen of once daily) for at least 3 to 4 weeks were assessed for HPA axis suppression. The mean BSA treated was 65%. None of the 40 evaluable subjects were suppressed. The criterion for HPA axis suppression was a serum cortisol level of less than or equal to 18 micrograms per deciliter at 30-minutes after cosyntropin stimulation. Another open label HPA axis suppression trial (Trial B) enrolled 56 pediatric subjects (ages 3 months to 11 months) with moderate to severe atopic dermatitis covering ≥ 35% BSA. Subjects were treated with an exaggerated dosing regimen for of fluticasone propionate lotion twice daily over a period of 3 or 4 weeks. The mean BSA treated was 54%. Out of 56 subjects, 49 were considered evaluable with respect to their adrenal axis function post-treatment. One of 49 subjects showed laboratory evidence of suppression immediately post treatment. The criterion for HPA axis suppression was a serum cortisol level of less than or equal to 18 micrograms per deciliter at 30-minutes after cosyntropin stimulation. Repeated test one week later showed the post cosyntropin stimulation testing serum cortisol returned to normal level (22.1 mcg/dL). This 4-month old subject had a baseline treatment BSA of 94% and was reported to have received 100% of the twice-daily applications of fluticasone propionate lotion over the 27 day treatment period. 12.3 Pharmacokinetics Absorption The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the vehicle and the integrity of the epidermal barrier. Occlusive dressing enhances penetration. Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin increase percutaneous absorption. Plasma fluticasone levels were measured in a subset of subjects 2 to 5 years and 11 months of age in HPA axis suppression trial (Trial A) described above. A total of 13 (62%) of 21 subjects tested had measurable fluticasone at the end of 3 to 4 weeks of treatment. The mean ± SD fluticasone plasma concentration was 0.16 ± 0.23 ng/mL. Three subjects aged 3, 4, and 4 years had fluticasone concentrations over 0.30 ng/mL, with one of them having a concentration of 0.82 ng/mL. No data were obtained for subjects < 2 years of age. Distribution The percentage of fluticasone propionate bound to human plasma proteins averaged 91%. Fluticasone propionate is weakly and reversibly bound to erythrocytes. Fluticasone propionate is not significantly bound to human transcortin. Metabolism No metabolites of fluticasone propionate were detected in an in vitro study of radiolabeled fluticasone propionate incubated in a human skin homogenate. Fluticasone propionate is metabolized in the liver by cytochrome P450 3A4-mediated hydrolysis of the 5-fluoromethyl carbothiolate grouping. This transformation occurs in 1 metabolic step to produce the inactive 17β-carboxylic acid metabolite, the only known metabolite detected in man. This metabolite has approximately 2000 times less affinity than the parent drug for the glucocorticoid receptor of human lung cytosol in vitro and negligible pharmacological activity in animal studies. Other metabolites detected in vitro using cultured human hepatoma cells have not been detected in man.
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action Corticosteroids play a role in cellular signaling, immune function, inflammation, and protein regulation; however, the precise mechanism of action of fluticasone propionate lotion in atopic dermatitis is unknown.
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Vasoconstrictor Assay Trials performed with fluticasone propionate lotion indicate that it is in the medium range of potency as demonstrated in vasoconstrictor trials in healthy subjects when compared with other topical corticosteroids. However, similar blanching scores do not necessarily imply therapeutic equivalence. Hypothalamic-Pituitary-Adrenal (HPA) Axis Suppression In an open label HPA axis suppression trial (Trial A), 42 pediatric subjects (ages 4 months to <6 years) with moderate to severe atopic dermatitis covering ≥ 35% Body Surface Area (BSA) who were treated with an exaggerated dosing regimen of fluticasone propionate lotion twice daily (rather than the indicated dosing regimen of once daily) for at least 3 to 4 weeks were assessed for HPA axis suppression. The mean BSA treated was 65%. None of the 40 evaluable subjects were suppressed. The criterion for HPA axis suppression was a serum cortisol level of less than or equal to 18 micrograms per deciliter at 30-minutes after cosyntropin stimulation. Another open label HPA axis suppression trial (Trial B) enrolled 56 pediatric subjects (ages 3 months to 11 months) with moderate to severe atopic dermatitis covering ≥ 35% BSA. Subjects were treated with an exaggerated dosing regimen for of fluticasone propionate lotion twice daily over a period of 3 or 4 weeks. The mean BSA treated was 54%. Out of 56 subjects, 49 were considered evaluable with respect to their adrenal axis function post-treatment. One of 49 subjects showed laboratory evidence of suppression immediately post treatment. The criterion for HPA axis suppression was a serum cortisol level of less than or equal to 18 micrograms per deciliter at 30-minutes after cosyntropin stimulation. Repeated test one week later showed the post cosyntropin stimulation testing serum cortisol returned to normal level (22.1 mcg/dL). This 4-month old subject had a baseline treatment BSA of 94% and was reported to have received 100% of the twice-daily applications of fluticasone propionate lotion over the 27 day treatment period.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Absorption The extent of percutaneous absorption of topical corticosteroids is determined by many factors, including the vehicle and the integrity of the epidermal barrier. Occlusive dressing enhances penetration. Topical corticosteroids can be absorbed from normal intact skin. Inflammation and/or other disease processes in the skin increase percutaneous absorption. Plasma fluticasone levels were measured in a subset of subjects 2 to 5 years and 11 months of age in HPA axis suppression trial (Trial A) described above. A total of 13 (62%) of 21 subjects tested had measurable fluticasone at the end of 3 to 4 weeks of treatment. The mean ± SD fluticasone plasma concentration was 0.16 ± 0.23 ng/mL. Three subjects aged 3, 4, and 4 years had fluticasone concentrations over 0.30 ng/mL, with one of them having a concentration of 0.82 ng/mL. No data were obtained for subjects < 2 years of age. Distribution The percentage of fluticasone propionate bound to human plasma proteins averaged 91%. Fluticasone propionate is weakly and reversibly bound to erythrocytes. Fluticasone propionate is not significantly bound to human transcortin. Metabolism No metabolites of fluticasone propionate were detected in an in vitro study of radiolabeled fluticasone propionate incubated in a human skin homogenate. Fluticasone propionate is metabolized in the liver by cytochrome P450 3A4-mediated hydrolysis of the 5-fluoromethyl carbothiolate grouping. This transformation occurs in 1 metabolic step to produce the inactive 17β-carboxylic acid metabolite, the only known metabolite detected in man. This metabolite has approximately 2000 times less affinity than the parent drug for the glucocorticoid receptor of human lung cytosol in vitro and negligible pharmacological activity in animal studies. Other metabolites detected in vitro using cultured human hepatoma cells have not been detected in man.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS None. • None ( Error! Hyperlink reference not valid. )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION Fluticasone propionate lotion USP, 0.05% contains fluticasone propionate USP S -Fluoromethyl 6α,9α-difluoro-11β-hydroxy-16α-methyl-3-oxo-17α-propionyloxyandrosta-1,4-diene-17β-carbothioate, a synthetic fluorinated corticosteroid, for topical use. The topical corticosteroids constitute a class of primarily synthetic steroids used as anti-inflammatory and antipruritic agents. Chemically, fluticasone propionate USP is C 25 H 31 F 3 O 5 S. It has the following structural formula: Fluticasone propionate USP is a white or almost white powder with a molecular weight of 500.6 g/mol. It is freely soluble in dimethylformamide; slightly soluble in alcohol; sparingly soluble in acetone and in dichloromethane; insoluble in water. Each gram of fluticasone propionate lotion USP contains 0.5 mg fluticasone propionate USP in a base of cetostearyl alcohol, polyoxyl 20 cetostearyl ether, citric acid anhydrous, dimethicone 360, isopropyl myristate, light mineral oil, propylene glycol, sodium citrate anhydrous, sorbitan monostearate, and purified water, with imidurea, methylparaben, and propylparaben as preservatives. chemical-structure
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION Apply a thin film of fluticasone propionate lotion to the affected skin areas once daily. Rub in gently. Discontinue use when control is achieved. If no improvement is seen within 2 weeks, reassessment of the diagnosis may be necessary. The safety and efficacy of fluticasone propionate lotion have not been established beyond 4 weeks of use. Avoid use with occlusive dressings or application to the diaper area [ see Warnings and Precautions ( Error! Hyperlink reference not valid. ) and ( Error! Hyperlink reference not valid. ) ]. Fluticasone propionate lotion is for topical use only, and not for ophthalmic, oral, or intravaginal use. • Apply a thin film to the affected skin areas once daily. Rub in gently. ( Error! Hyperlink reference not valid. ) • Discontinue use when control is achieved. ( Error! Hyperlink reference not valid. ) • Reassess diagnosis if no improvement in 2 weeks. ( Error! Hyperlink reference not valid. ) • The safety and efficacy of fluticasone propionate lotion have not been established beyond four weeks of use. ( Error! Hyperlink reference not valid. ) • Avoid use under occlusion or application to diaper area. ( Error! Hyperlink reference not valid. ) • Not for ophthalmic, oral, or intravaginal use. ( Error! Hyperlink reference not valid. )
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Lotion, 0.05%. Each gram of fluticasone propionate lotion USP contains 0.5 mg fluticasone propionate USP in a white translucent smooth homogeneous lotion. Fluticasone propionate lotion USP is supplied in 60 mL bottles. • Lotion, 0.05%, supplied in 60 mL bottles. ( Error! Hyperlink reference not valid. )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE Fluticasone propionate lotion is a corticosteroid indicated for the relief of the inflammatory and pruritic manifestations of atopic dermatitis in patients 3 months of age or older. Fluticasone propionate lotion is a corticosteroid indicated for the relief of the inflammatory and pruritic manifestations of atopic dermatitis in patients 3 year of age and older. ( 1 )
Spl product data elements
Usually a list of ingredients in a drug product.Fluticasone Propionate Fluticasone Propionate FLUTICASONE PROPIONATE FLUTICASONE CETOSTEARYL ALCOHOL POLYOXYL 20 CETOSTEARYL ETHER ANHYDROUS CITRIC ACID DIMETHICONE 350 ISOPROPYL MYRISTATE LIGHT MINERAL OIL PROPYLENE GLYCOL ANHYDROUS TRISODIUM CITRATE SORBITAN MONOSTEARATE WATER IMIDUREA METHYLPARABEN PROPYLPARABEN
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility In an oral (gavage) mouse carcinogenicity study, doses of 0.1, 0.3 and 1 mg/kg/day fluticasone propionate were administered to mice for 18 months. Fluticasone propionate demonstrated no tumorigenic potential at oral doses up to 1 mg/kg/day (less than the MRHD in adults based on body surface area comparisons) in this study. In a dermal mouse carcinogenicity study, 0.05% fluticasone propionate ointment (40 μl) was topically administered for 1, 3 or 7 days/week for 80 weeks. Fluticasone propionate demonstrated no tumorigenic potential at dermal doses up to 6.7 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) in this study. Fluticasone propionate revealed no evidence of mutagenic or clastogenic potential based on the results of five in vitro genotoxicity tests (Ames assay, E. coli fluctuation test, S. cerevisiae gene conversion test, Chinese hamster ovary cell chromosome aberration assay and human lymphocyte chromosome aberration assay) and one in vivo genotoxicity test (mouse micronucleus assay). No evidence of impairment of fertility or effect on mating performance was observed in a fertility and general reproductive performance study conducted in male and female rats at subcutaneous doses up to 50 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons).
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility In an oral (gavage) mouse carcinogenicity study, doses of 0.1, 0.3 and 1 mg/kg/day fluticasone propionate were administered to mice for 18 months. Fluticasone propionate demonstrated no tumorigenic potential at oral doses up to 1 mg/kg/day (less than the MRHD in adults based on body surface area comparisons) in this study. In a dermal mouse carcinogenicity study, 0.05% fluticasone propionate ointment (40 μl) was topically administered for 1, 3 or 7 days/week for 80 weeks. Fluticasone propionate demonstrated no tumorigenic potential at dermal doses up to 6.7 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) in this study. Fluticasone propionate revealed no evidence of mutagenic or clastogenic potential based on the results of five in vitro genotoxicity tests (Ames assay, E. coli fluctuation test, S. cerevisiae gene conversion test, Chinese hamster ovary cell chromosome aberration assay and human lymphocyte chromosome aberration assay) and one in vivo genotoxicity test (mouse micronucleus assay). No evidence of impairment of fertility or effect on mating performance was observed in a fertility and general reproductive performance study conducted in male and female rats at subcutaneous doses up to 50 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons).
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PACKAGE LABEL – PRINCIPAL DISPLAY PANEL NDC 68462-427-02 FLUTICASONE PROPIONATE LOTION USP 0.05% PHARMACIST: Dispense with the enclosed Patient Information leaflet For topical use only. Not for ophthalmic, oral or intravaginal use. fluticasone-label
Spl unclassified section
Information not classified as belonging to one of the other fields. Approximately 40% of labeling with effective_time between June 2009 and August 2014 have information in this field.Manufactured by: Glenmark Pharmaceuticals Limited Village Kishanpura, Baddi Nalagarh Road District: Solan, Himachal Pradesh – 173205, India Manufactured for: Glenmark Pharmaceuticals Inc., USA Mahwah, NJ 07430 Questions? 1 (888) 721-7115 www.glenmarkpharma-us.com February 2020
Fluticasone Propionate: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Advise the patient to read the FDA-approved patient labeling (Patient Information). Administration Instructions Advise the patient of appropriate fluticasone propionate lotion administration instructions, including those that will mitigate HPA-Axis suppression [ see Warnings and Precautions ( Error! Hyperlink reference not valid. ) ] and local adverse reactions [ see Warnings and Precautions ( Error! Hyperlink reference not valid. ) ]: • Discontinue therapy when control is achieved in less than 4 weeks; if no improvement is seen within 2 weeks, contact the healthcare provider. • Avoid contact with the eyes. • Do not bandage the treated skin area, or cover or wrap it to cause occlusion unless directed by the healthcare provider. • Do not use fluticasone propionate lotion in the treatment of diaper dermatitis unless directed by the healthcare provider, as diapers or plastic pants may constitute occlusive dressing and enhance absorption. • Do not use on the face, underarms, or groin areas unless directed by the healthcare provider. Local Adverse Reactions Advise the patient to report any signs of local adverse reactions to their healthcare provider [ see Warnings and Precautions ( Error! Hyperlink reference not valid. ) ]. • Advise patients to report to their healthcare provider if they are allergic to formaldehyde.
Spl patient package insert
Information necessary for patients to use the drug safely and effectively.PATIENT INFORMATION Fluticasone Propionate (floo tik’ a sone proe’ pee oh nate) Lotion, 0.05% Important: fluticasone propionate lotion is for use on skin only (topical). Do not get fluticasone propionate lotion near or in your eyes, mouth, or vagina. Read this Patient Information before you start using fluticasone propionate lotion and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. What is fluticasone propionate lotion? Fluticasone propionate lotion is a prescription corticosteroid medicine used on the skin (topical) for the relief of inflammation and itching caused by certain skin conditions, including atopic dermatitis and eczema in people 3 months of age and older. It is not known if fluticasone propionate lotion is safe and effective in children under 3 months of age. Before using fluticasone propionate lotion, tell your healthcare provider about all of your medical conditions, including if you: • have a skin infection at the site to be treated. You may also need medicine to treat the skin infection. • have adrenal gland problems • have liver problems • have diabetes • have thinning skin (atrophy) at the site to be treated • are allergic to formaldehyde. If you are allergic to formaldehyde, fluticasone propionate lotion may cause skin irritation, prevent your skin from healing or worsen your skin condition. • are pregnant or plan to become pregnant. It is not known if fluticasone propionate lotion will harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if fluticasone propionate lotion can pass into your breast milk and harm your baby. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially tell your healthcare provider if you take other corticosteroid medicines by mouth or use other products on your skin that contain corticosteroids. How should I use fluticasone propionate lotion? • Use fluticasone propionate lotion exactly as your healthcare provider tells you to use it. • Apply a thin film of fluticasone propionate lotion to the affected area 1 time each day. Gently rub into your skin. • Do not bandage, cover, or wrap the treated area unless your healthcare provider tells you to. Do not apply fluticasone propionate lotion to dermatitis in the diaper area unless your healthcare provider tells you to. • Wash your hands after applying fluticasone propionate lotion, unless your hands are being treated. • Tell your healthcare provider if your symptoms get worse with fluticasone propionate lotion or if your symptoms do not improve after 2 weeks of treatment. It is not known if fluticasone propionate lotion is safe or effective when used more than 4 weeks. What are possible side effects with fluticasone propionate lotion? Fluticasone propionate lotion may cause serious side effects, including: • Fluticasone propionate lotion can pass through your skin and may cause adrenal gland problems. This is more likely to happen if you use fluticasone propionate lotion for too long, use it over a large treatment area, use it with other topical medicines that contain corticosteroids, cover the treated area, or have liver failure. Your healthcare provider may do blood tests to check your adrenal gland function during and after treatment with fluticasone propionate lotion. • Skin problems, including skin reactions or thinning of your skin (atrophy), skin infections, and allergic reactions (allergic contact dermatitis) at the treatment site. Tell your healthcare provider if you get any skin reactions such as pain, tenderness, swelling, or healing problems. The most common side effects of fluticasone propionate lotion include burning and stinging at the treatment site. These are not all the possible side effects with fluticasone propionate lotion. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store fluticasone propionate lotion? • Store fluticasone propionate lotion at 20ºC to 25º C (68ºF to 77º F) [see USP Controlled Room Temperature]. • Do not refrigerate. • Keep container tightly sealed. Keep fluticasone propionate lotion and all medicines out of the reach of children. General information about the safe and effective use of fluticasone propionate lotion. Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use fluticasone propionate lotion for a condition for which it was not prescribed. Do not give fluticasone propionate lotion to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or healthcare provider for information about fluticasone propionate lotion that is written for health professionals. What are the ingredients in fluticasone propionate lotion? Active ingredient: fluticasone propionate Inactive ingredients: cetostearyl alcohol, polyoxyl 20 cetostearyl ether, citric acid anhydrous, dimethicone 360, isopropyl myristate, light mineral oil, propylene glycol, sodium citrate anhydrous, sorbitan monostearate, and purified water, with imidurea, methylparaben, and propylparaben. This Patient Information has been approved by the U.S. Food and Drug Administration Manufactured by: Glenmark Pharmaceuticals Limited Village Kishanpura, Baddi Nalagarh Road District: Solan, Himachal Pradesh – 173205, India Manufactured for: Glenmark Pharmaceuticals Inc., USA Mahwah, NJ 07430 Questions? 1 (888) 721-7115 www.glenmarkpharma-us.com February 2020
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES Fluticasone propionate lotion applied once daily was superior to vehicle in the treatment of atopic dermatitis in two clinical trials. The two trials enrolled 438 subjects with atopic dermatitis aged 3 months and older, of which 169 subjects were selected as having clinically significant signs of erythema, infiltration/papulation, and erosion/oozing/crusting at baseline. Clinically significant was defined as having moderate or severe involvement for at least two of the three signs (erythema, infiltrations/papulation, or erosion/oozing/crusting), in at least 2 body regions. Subjects who had moderate to severe disease in a single body region were excluded from the analysis. Table 3 presents the percentage of subjects who completely cleared of erythema, infiltration/papulation and erosion/oozing/crusting at Week 4 out of those subjects with clinically significant baseline signs. Table 3: Complete Clearance Rate For Patients with Clinically Significant Signs at Baseline Fluticasone propionate lotion Vehicle Study 1 9/45 (20%) 0/37 (0%) Study 2 7/44 (16%) 1/43 (2%)
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use A limited number of patients above 65 years of age have been treated with fluticasone propionate lotion in US and non-US clinical trials. Specifically only 8 patients above 65 years of age were treated with fluticasone propionate lotion in controlled clinical trials. The number of patients is too small to permit separate analyses of efficacy and safety.
Nursing mothers
Information about excretion of the drug in human milk and effects on the nursing infant, including pertinent adverse effects observed in animal offspring.8.3 Nursing Mothers Systemically administered corticosteroids appear in human milk and can suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when fluticasone propionate lotion is administered to a nursing woman.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use Fluticasone propionate lotion may be used in pediatric patients as young as 3 months of age. The safety and effectiveness of fluticasone propionate lotion in pediatric patients below 3 months of age have not been established. Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of systemic effects when treated with topical drugs. They are, therefore, also at greater risk of HPA axis suppression and adrenal insufficiency upon the use of topical corticosteroids [see Warnings and Precautions ( 5.1 )]. In an HPA axis suppression trial, none of the 40 evaluable pediatric subjects, 4 months old to < 6 years old, with moderate to severe atopic dermatitis covering ≥ 35% Body Surface Area (BSA) who were treated with an exaggerated dosing regimen (twice daily) of fluticasone propionate lotion experienced adrenal suppression (defined as a 30-minute post-stimulation cortisol level ≤18 micrograms/dL) [see Warnings and Precautions ( 5.1 ) and Clinical Pharmacology ( 12.2 )]. In another HPA axis suppression trial, one of 49 (2%) evaluable pediatric subjects, 3 months to 11 months old, with moderate to severe atopic dermatitis covering ≥ 35% Body Surface Area (BSA) who applied an exaggerated dosing regimen (twice daily) of fluticasone propionate lotion experienced reversible adrenal suppression (defined as a 30-minute post-stimulation cortisol level ≤18 micrograms/dL) following 4 weeks of therapy [see Warnings and Precautions ( 5.1 )and Clinical Pharmacology (12.2)]. Systemic effects such as Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in pediatric patients, especially those with prolonged exposure to large doses of high-potency topical corticosteroids, or concomitant use of more than one corticosteroid product. Local adverse reactions including skin atrophy have also been reported with use of topical corticosteroids in pediatric patients. Parents of pediatric patients should be advised not to use this medication in the treatment of diaper dermatitis unless directed by a physician. Fluticasone propionate lotion should not be applied in the diaper areas as diapers or plastic pants may constitute occlusive dressing.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Pregnancy Category C There are no adequate and well-controlled studies in pregnant women. Therefore, fluticasone propionate lotion should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Systemic embryofetal development studies were conducted in mice, rats and rabbits. Subcutaneous doses of 15, 45 and 150 mcg/kg/day of fluticasone propionate were administered to pregnant female mice from gestation days 6 to 15. A teratogenic effect characteristic of corticosteroids (cleft palate) was noted after administration of 45 and 150 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) in this study. No treatment related effects on embryofetal toxicity or teratogenicity were noted at 15 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons). Subcutaneous doses of 10, 30 and 100 mcg/kg/day of fluticasone propionate were administered to pregnant female rats in two embryofetal development studies (one study administered fluticasone propionate from gestation days 6 to 15 and the other study from gestation days 7 to 17). In the presence of maternal toxicity, fetal effects noted at 100 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) included decreased fetal weights, omphalocele, cleft palate, and retarded skeletal ossification. No treatment related effects on embryofetal toxicity or teratogenicity were noted at 10 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons). Subcutaneous doses of 0.08, 0.57 and 4 mcg/kg/day of fluticasone propionate were administered to pregnant female rabbits from gestation days 6 to 18. Fetal effects noted at 4 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) included decreased fetal weights, cleft palate and retarded skeletal ossification. No treatment related effects on embryofetal toxicity or teratogenicity were noted at 0.57 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons). Oral doses of 3, 30 and 300 mcg/kg/day fluticasone propionate were administered to pregnant female rabbits from gestation days 8 to 20. No fetal or teratogenic effects were noted at oral doses up to 300 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) in this study. However, no fluticasone propionate was detected in the plasma in this study, consistent with the established low bioavailability following oral administration. Fluticasone propionate crossed the placenta following administration of a subcutaneous or an oral dose of 100 μg/kg tritiated fluticasone propionate to pregnant rats.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Pregnancy Category C There are no adequate and well-controlled studies in pregnant women. Therefore, fluticasone propionate lotion should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Systemic embryofetal development studies were conducted in mice, rats and rabbits. Subcutaneous doses of 15, 45 and 150 mcg/kg/day of fluticasone propionate were administered to pregnant female mice from gestation days 6 to 15. A teratogenic effect characteristic of corticosteroids (cleft palate) was noted after administration of 45 and 150 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) in this study. No treatment related effects on embryofetal toxicity or teratogenicity were noted at 15 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons). Subcutaneous doses of 10, 30 and 100 mcg/kg/day of fluticasone propionate were administered to pregnant female rats in two embryofetal development studies (one study administered fluticasone propionate from gestation days 6 to 15 and the other study from gestation days 7 to 17). In the presence of maternal toxicity, fetal effects noted at 100 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) included decreased fetal weights, omphalocele, cleft palate, and retarded skeletal ossification. No treatment related effects on embryofetal toxicity or teratogenicity were noted at 10 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons). Subcutaneous doses of 0.08, 0.57 and 4 mcg/kg/day of fluticasone propionate were administered to pregnant female rabbits from gestation days 6 to 18. Fetal effects noted at 4 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) included decreased fetal weights, cleft palate and retarded skeletal ossification. No treatment related effects on embryofetal toxicity or teratogenicity were noted at 0.57 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons). Oral doses of 3, 30 and 300 mcg/kg/day fluticasone propionate were administered to pregnant female rabbits from gestation days 8 to 20. No fetal or teratogenic effects were noted at oral doses up to 300 mcg/kg/day (less than the MRHD in adults based on body surface area comparisons) in this study. However, no fluticasone propionate was detected in the plasma in this study, consistent with the established low bioavailability following oral administration. Fluticasone propionate crossed the placenta following administration of a subcutaneous or an oral dose of 100 μg/kg tritiated fluticasone propionate to pregnant rats. 8.3 Nursing Mothers Systemically administered corticosteroids appear in human milk and can suppress growth, interfere with endogenous corticosteroid production, or cause other untoward effects. It is not known whether topical administration of corticosteroids could result in sufficient systemic absorption to produce detectable quantities in human milk. Because many drugs are excreted in human milk, caution should be exercised when fluticasone propionate lotion is administered to a nursing woman. 8.4 Pediatric Use Fluticasone propionate lotion may be used in pediatric patients as young as 3 months of age. The safety and effectiveness of fluticasone propionate lotion in pediatric patients below 3 months of age have not been established. Because of a higher ratio of skin surface area to body mass, pediatric patients are at a greater risk than adults of systemic effects when treated with topical drugs. They are, therefore, also at greater risk of HPA axis suppression and adrenal insufficiency upon the use of topical corticosteroids [see Warnings and Precautions ( 5.1 )]. In an HPA axis suppression trial, none of the 40 evaluable pediatric subjects, 4 months old to < 6 years old, with moderate to severe atopic dermatitis covering ≥ 35% Body Surface Area (BSA) who were treated with an exaggerated dosing regimen (twice daily) of fluticasone propionate lotion experienced adrenal suppression (defined as a 30-minute post-stimulation cortisol level ≤18 micrograms/dL) [see Warnings and Precautions ( 5.1 ) and Clinical Pharmacology ( 12.2 )]. In another HPA axis suppression trial, one of 49 (2%) evaluable pediatric subjects, 3 months to 11 months old, with moderate to severe atopic dermatitis covering ≥ 35% Body Surface Area (BSA) who applied an exaggerated dosing regimen (twice daily) of fluticasone propionate lotion experienced reversible adrenal suppression (defined as a 30-minute post-stimulation cortisol level ≤18 micrograms/dL) following 4 weeks of therapy [see Warnings and Precautions ( 5.1 )and Clinical Pharmacology (12.2)]. Systemic effects such as Cushing’s syndrome, linear growth retardation, delayed weight gain, and intracranial hypertension have been reported in pediatric patients, especially those with prolonged exposure to large doses of high-potency topical corticosteroids, or concomitant use of more than one corticosteroid product. Local adverse reactions including skin atrophy have also been reported with use of topical corticosteroids in pediatric patients. Parents of pediatric patients should be advised not to use this medication in the treatment of diaper dermatitis unless directed by a physician. Fluticasone propionate lotion should not be applied in the diaper areas as diapers or plastic pants may constitute occlusive dressing. 8.5 Geriatric Use A limited number of patients above 65 years of age have been treated with fluticasone propionate lotion in US and non-US clinical trials. Specifically only 8 patients above 65 years of age were treated with fluticasone propionate lotion in controlled clinical trials. The number of patients is too small to permit separate analyses of efficacy and safety.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING Fluticasone propionate lotion USP, 0.05% is a white translucent smooth homogeneous lotion supplied in HDPE and PP bottles as follows: 60 mL bottles: (NDC 68462-427-02) Store at 20°C to 25°C (68°F to 77°F) [see USP Controlled Room Temperature]. Do not refrigerate. Keep container tightly sealed.
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API