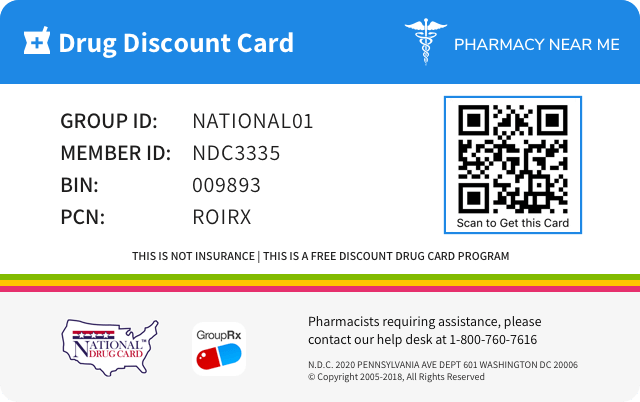
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 0378-4500 | ||||
|---|---|---|---|---|---|
| Drug Name | Budesonide |
||||
| Type | Generic | ||||
| Pharm Class | Corticosteroid Hormone Receptor Agonists [MoA], Corticosteroid [EPC] |
||||
| Active Ingredients |
|
||||
| Route | ORAL | ||||
| Dosage Form | TABLET, FILM COATED, EXTENDED RELEASE | ||||
| RxCUI drug identifier | 1366550 | ||||
| Application Number | ANDA208851 | ||||
| Labeler Name | Mylan Pharmaceuticals Inc. | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Overdosage of Budesonide
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE Reports of acute toxicity and/or death following overdosage of glucocorticosteroids are rare. Treatment consists of immediate gastric lavage or emesis followed by supportive and symptomatic therapy. If glucocorticosteroids are used at excessive doses for prolonged periods, systemic glucocorticosteroid effects, such as hypercorticism and adrenal suppression may occur. For chronic overdosage in the face of severe disease requiring continuous steroid therapy, the dosage may be reduced temporarily. Single oral budesonide doses of 200 and 400 mg/kg were lethal in female and male mice, respectively. The signs of acute toxicity were decreased motor activity, piloerection and generalized edema.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS Systemic glucocorticosteroid use may result in the following: • Hypercorticism and Adrenal Suppression [see Warnings and Precautions (5.1) ] • Symptoms of steroid withdrawal in those patients transferring from Systemic Glucocorticosteroid Therapy [see Warnings and Precautions (5.2) ] • Immunosuppression and Increased Risk of Infection [see Warnings and Precautions (5.3) ] • Kaposi’s Sarcoma [see Warnings and Precautions (5.4) ] • Increased Systemic Glucocorticoid Susceptibility [see Warnings and Precautions (5.5) ] • Other Glucocorticosteroid Effects [see Warnings and Precautions (5.6) ] Most common adverse reactions (incidence ≥ 2%) are headache, nausea, decreased blood cortisol, upper abdominal pain, fatigue, flatulence, abdominal distension, acne, urinary tract infection, arthralgia, and constipation. ( 6.1 ) To report SUSPECTED ADVERSE REACTIONS, contact Viatris at 1-877-446-3679 (1-877-4-INFO-RX) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The safety of budesonide extended-release tablets has been evaluated in controlled and open-label clinical trials which enrolled a combined total of 1,105 patients with ulcerative colitis. In two 8-week, placebo-controlled studies in patients with active disease (Study 1 and Study 2), a total of 255 patients received budesonide extended-release tablets 9 mg, 254 patients received budesonide extended-release tablets 6 mg, and 258 patients received placebo. They ranged in age from 18-77 years (mean = 43), 56% were male, and 75% were Caucasian. The most common adverse reactions were headache, nausea, decreased blood cortisol, upper abdominal pain, fatigue, flatulence, abdominal distension, acne, urinary tract infection, arthralgia, and constipation. The adverse reactions occurring in 2% or more of patients on therapy with budesonide extended-release tablets 9 mg are summarized in Table 1. Table 1. Summary of Adverse Reactions in Two Placebo-Controlled Trials Experienced by at Least 2% of the Budesonide Extended-Release Tablets 9 mg Group (Studies 1 and 2) Budesonide Extended- Release Tablets 9 mg (N = 255) n (%) Budesonide Extended- Release Tablets 6 mg (N = 254) n (%) Placebo (N = 258) n (%) Headache 29 (11.4) 37 (14.6) 27 (10.5) Nausea 13 (5.1) 12 (4.7) 11 (4.3) Decreased blood cortisol 11 (4.3) 6 (2.4) 1 (0.4) Upper abdominal pain 10 (3.9) 8 (3.1) 5 (1.9) Fatigue 8 (3.1) 5 (2.0) 5 (1.9) Flatulence 6 (2.4) 8 (3.1) 5 (1.9) Abdominal distension 6 (2.4) 4 (1.6) 2 (0.8) Acne 6 (2.4) 2 (0.8) 5 (1.9) Urinary tract infection 5 (2.0) 1 (0.4) 1 (0.4) Arthralgia 5 (2.0) 5 (2.0) 4 (1.6) Constipation 5 (2.0) 1 (0.4) 2 (0.8) Of budesonide extended-release tablets 9 mg patients, a total of 15% discontinued treatment due to any adverse event (including adverse reactions) compared with 17% in the placebo group. Table 2 summarizes the percentages of patients reporting glucocorticoid-related effects in the 2 placebo-controlled studies. Table 2. Summary of Glucocorticoid-Related Effects in Two Placebo-Controlled Trials (Studies 1 and 2) Budesonide Extended-Release Tablets 9 mg (N = 255) n (%) Budesonide Extended-Release Tablets 6 mg (N = 254) n (%) Placebo (N = 258) n (%) Overall 26 (10.2) 19 (7.5) 27 (10.5) Mood changes 9 (3.5) 10 (3.9) 11 (4.3) Sleep changes 7 (2.7) 10 (3.9) 12 (4.7) Insomnia 6 (2.4) 6 (2.4) 8 (3.1) Acne 6 (2.4) 2 (0.8) 5 (1.9) Moon face 3 (1.2) 3 (1.2) 4 (1.6) Fluid retention 2 (0.8) 3 (1.2) 3 (1.2) Hirsutism 1 (0.4) 0 0 Striae rubrae 0 0 2 (0.8) Flushing 0 1 (0.4) 3 (1.2) No clinically significant differences were observed with respect to the overall percentages of patients with any glucocorticoid-related effects between budesonide extended-release tablets and placebo after 8 weeks of induction therapy. Study 3 was an open-label study evaluating budesonide extended-release tablets 9 mg once daily for 8 weeks in 60 patients who had previously completed an 8-week induction study (Study 1) but had not achieved remission. Among patients who took budesonide extended-release tablets 9 mg up to 16 weeks cumulatively across Study 1 and Study 3 combined, similar rates of adverse reactions and glucocorticoid-related effects were seen compared to those who took budesonide extended-release tablets 9 mg for 8 weeks in Study 1. In Study 4, the safety of long-term treatment with budesonide extended-release tablets 6 mg was evaluated in a placebo-controlled 12-month maintenance study of 123 patients. Patients who had previously completed 8 weeks of therapy in any induction study (Study 1, 2, or 3) and were in remission were randomized to budesonide extended-release tablets 6 mg or placebo once daily for 12 months. In patients who took budesonide extended-release tablets 6 mg for up to 12 months, similar rates of adverse reactions were seen between placebo and budesonide extended-release tablets 6 mg. After up to 12 months of study treatment, 77% (27/35) of the patients in the budesonide extended-release tablets 6 mg and 74% (29/39) of the patients in the placebo treatment groups had normal bone density scans. In Study 4, the glucocorticoid-related effects were similar in patients with up to 12 months of therapy with budesonide extended-release tablets 6 mg and placebo (Table 3). Table 3. Summary of Glucocorticoid-Related Effects Over 12-Month Treatment (Study 4) Budesonide Extended- Release Tablets 6 mg (N = 62) n (%) Placebo (N = 61) n (%) Overall 9 (14.5) 7 (11.5) Insomnia 4 (6.5) 4 (6.6) Mood changes 4 (6.5) 2 (3.3) Moon face 3 (4.8) 3 (4.9) Sleep changes 3 (4.8) 3 (4.9) Acne 3 (4.8) 0 Hirsutism 3 (4.8) 0 Flushing 1 (1.6) 1 (1.6) Fluid retention 1 (1.6) 1 (1.6) 6.2 Postmarketing Experience In addition to adverse events reported from clinical trials, the following adverse reactions have been identified during post-approval use of oral budesonide. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. These events have been chosen for inclusion due to either their seriousness, frequency of reporting or causal connection to budesonide extended-release tablets, or a combination of these factors. Gastrointestinal Disorders: diarrhea, rectal bleeding General Disorders and Administrative Site Conditions: peripheral edema Immune System Disorders: anaphylactic reactions Musculoskeletal and Connective Tissue Disorders: muscle cramps/spasms Nervous System Disorders: benign intracranial hypertension, dizziness Psychiatric Disorders: mood swings Skin and Subcutaneous Tissue Disorders: rash Vascular Disorders: increased blood pressure
Budesonide Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS • Avoid cytochrome P450 3A4 inhibitors (e.g., ketoconazole, grapefruit juice). May cause increased systemic corticosteroid effects. ( 2.2 , 7 , 12.3 ) 7.1 Interaction with CYP3A4 Inhibitors Concomitant oral administration of ketoconazole (a known inhibitor of CYP3A4 activity in the liver and in the intestinal mucosa) caused an eight-fold increase of the systemic exposure to oral budesonide. If treatment with inhibitors of CYP3A4 activity (such as ketoconazole, itraconazole, ritonavir, indinavir, saquinavir, erythromycin) is indicated, discontinuation of budesonide extended-release tablets should be considered. After extensive intake of grapefruit juice (which inhibits CYP3A4 activity predominantly in the intestinal mucosa), the systemic exposure for oral budesonide increased about two times. Ingestion of grapefruit or grapefruit juice should be avoided in connection with budesonide extended-release tablets administration [see Dosage and Administration (2) and Clinical Pharmacology (12.3) ] . 7.2 Inhibitors of Gastric Acid Secretion Since the dissolution of the coating of budesonide extended-release tablets is pH dependent, the release properties and uptake of the compound may be altered when budesonide extended-release tablets are used after treatment with gastric acid reducing agents (e.g., proton pump inhibitors (PPIs), H 2 blockers and antacids).
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Budesonide has a high topical glucocorticosteroid (GCS) activity and substantial first-pass elimination. The formulation contains budesonide in an extended-release tablet core. The tablet core is enteric coated to protect dissolution in gastric juice which delays budesonide release until exposure to a pH ≥ 7 in the small intestine. Upon disintegration of the coating, the core matrix provides extended release of budesonide in a time dependent manner. 12.2 Pharmacodynamics Budesonide has a high glucocorticoid effect and a weak mineralocorticoid effect, and the affinity of budesonide to GCS receptors, which reflects the intrinsic potency of the drug, is about 200-fold that of cortisol and 15-fold that of prednisolone. Treatment with systemically active GCS, including budesonide extended-release tablets, is associated with a suppression of endogenous cortisol concentrations and an impairment of the hypothalamus-pituitary-adrenal (HPA) axis function. Markers, indirect and direct, of this are cortisol levels in plasma or urine and response to ACTH stimulation. In a study assessing the response to ACTH stimulation test in patients treated with budesonide extended-release tablets 9 mg once daily, the proportion of patients with abnormal response was 47% at 4 weeks and 79% at 8 weeks. 12.3 Pharmacokinetics Absorption Following single oral administration of budesonide extended-release tablets 9 mg in healthy subjects, peak plasma concentration (C max ) was 1.35 ± 0.96 ng/mL, the time to peak concentration (T max ) on average was 13.3 ± 5.9 hours, although it varied across different individual patients, and the area under the plasma concentration time curve (AUC) was approximately 16.43 ± 10.52 ng•hr/mL. The pharmacokinetic parameters of budesonide extended-release tablets 9 mg have a high degree of variability among subjects. There was no accumulation of budesonide with respect to both AUC and C max following 7 days of budesonide extended-release tablets 9 mg once daily dosing. Food Effect A food-effect study involving administration of budesonide extended-release tablets to healthy volunteers under fasting conditions and with a high-fat meal indicated that the C max was decreased by 27% while there was no significant decrease in AUC. Additionally, a mean delay in absorption lag time of 2.4 hours was observed under fed conditions. Distribution The mean volume of distribution (V SS ) of budesonide varies between 2.2 and 3.9 L/kg in healthy subjects and in patients. Plasma protein binding is estimated to be 85 to 90% in the concentration range 1 to 230 nmol/L, independent of gender. The erythrocyte/plasma partition ratio at clinically relevant concentrations is about 0.8. Elimination Metabolism Following absorption, budesonide is subject to high first-pass metabolism (80-90%). In vitro experiments in human liver microsomes demonstrate that budesonide is rapidly and extensively biotransformed, mainly by CYP3A4, to its 2 major metabolites, 6β-hydroxy budesonide and 16α-hydroxy prednisolone. The glucocorticoid activity of these metabolites is negligible (< 1/100) in relation to that of the parent compound. In vivo investigations with intravenous doses in healthy subjects are in agreement with the in vitro findings and demonstrate that budesonide has a high plasma clearance, 0.9-1.8 L/min. These high plasma clearance values approach the estimated liver blood flow, and, accordingly, suggest that budesonide is a high hepatic clearance drug. The plasma elimination half-life, t 1/2 , after administration of intravenous doses ranges between 2 and 3.6 hours. Excretion Budesonide is excreted in urine and feces in the form of metabolites. After oral as well as intravenous administration of micronized [ 3 H]-budesonide, approximately 60% of the recovered radioactivity is found in urine. The major metabolites, including 6β-hydroxy budesonide and 16α-hydroxy prednisolone, are mainly renally excreted, intact or in conjugated forms. No unchanged budesonide is detected in urine. Specific Populations Patients with Renal Impairment The pharmacokinetics of budesonide in patients with renal impairment have not been studied. Intact budesonide is not renally excreted, but metabolites are to a large extent, and might therefore reach higher levels in patients with impaired renal function. However, these metabolites have negligible corticosteroid activity as compared with budesonide (< 1/100). Patients with Hepatic Impairment In patients with liver cirrhosis, systemic availability of orally administered budesonide correlates with disease severity and is, on average, 2.5-fold higher compared with healthy controls. Patients with mild liver disease are minimally affected. Patients with severe liver dysfunction were not studied. Absorption parameters were not altered, and for the intravenous dose, no significant differences in CL or V SS were observed. Drug Interaction Studies Budesonide is metabolized via CYP3A4. Potent inhibitors of CYP3A4 can increase the plasma levels of budesonide several-fold. Co-administration of ketoconazole results in an eight-fold increase in AUC of budesonide, compared to budesonide alone. Grapefruit juice, an inhibitor of gut mucosal CYP3A, approximately doubles the systemic exposure of oral budesonide. Conversely, induction of CYP3A4 can result in the lowering of budesonide plasma levels [see Dosage and Administration (2) and Drug Interactions (7) ]. Oral contraceptives containing ethinyl estradiol, which are also metabolized by CYP3A4, do not affect the pharmacokinetics of budesonide. Budesonide does not affect the plasma levels of oral contraceptives (i.e., ethinyl estradiol).
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action Budesonide has a high topical glucocorticosteroid (GCS) activity and substantial first-pass elimination. The formulation contains budesonide in an extended-release tablet core. The tablet core is enteric coated to protect dissolution in gastric juice which delays budesonide release until exposure to a pH ≥ 7 in the small intestine. Upon disintegration of the coating, the core matrix provides extended release of budesonide in a time dependent manner.
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Budesonide has a high glucocorticoid effect and a weak mineralocorticoid effect, and the affinity of budesonide to GCS receptors, which reflects the intrinsic potency of the drug, is about 200-fold that of cortisol and 15-fold that of prednisolone. Treatment with systemically active GCS, including budesonide extended-release tablets, is associated with a suppression of endogenous cortisol concentrations and an impairment of the hypothalamus-pituitary-adrenal (HPA) axis function. Markers, indirect and direct, of this are cortisol levels in plasma or urine and response to ACTH stimulation. In a study assessing the response to ACTH stimulation test in patients treated with budesonide extended-release tablets 9 mg once daily, the proportion of patients with abnormal response was 47% at 4 weeks and 79% at 8 weeks.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Absorption Following single oral administration of budesonide extended-release tablets 9 mg in healthy subjects, peak plasma concentration (C max ) was 1.35 ± 0.96 ng/mL, the time to peak concentration (T max ) on average was 13.3 ± 5.9 hours, although it varied across different individual patients, and the area under the plasma concentration time curve (AUC) was approximately 16.43 ± 10.52 ng•hr/mL. The pharmacokinetic parameters of budesonide extended-release tablets 9 mg have a high degree of variability among subjects. There was no accumulation of budesonide with respect to both AUC and C max following 7 days of budesonide extended-release tablets 9 mg once daily dosing. Food Effect A food-effect study involving administration of budesonide extended-release tablets to healthy volunteers under fasting conditions and with a high-fat meal indicated that the C max was decreased by 27% while there was no significant decrease in AUC. Additionally, a mean delay in absorption lag time of 2.4 hours was observed under fed conditions. Distribution The mean volume of distribution (V SS ) of budesonide varies between 2.2 and 3.9 L/kg in healthy subjects and in patients. Plasma protein binding is estimated to be 85 to 90% in the concentration range 1 to 230 nmol/L, independent of gender. The erythrocyte/plasma partition ratio at clinically relevant concentrations is about 0.8. Elimination Metabolism Following absorption, budesonide is subject to high first-pass metabolism (80-90%). In vitro experiments in human liver microsomes demonstrate that budesonide is rapidly and extensively biotransformed, mainly by CYP3A4, to its 2 major metabolites, 6β-hydroxy budesonide and 16α-hydroxy prednisolone. The glucocorticoid activity of these metabolites is negligible (< 1/100) in relation to that of the parent compound. In vivo investigations with intravenous doses in healthy subjects are in agreement with the in vitro findings and demonstrate that budesonide has a high plasma clearance, 0.9-1.8 L/min. These high plasma clearance values approach the estimated liver blood flow, and, accordingly, suggest that budesonide is a high hepatic clearance drug. The plasma elimination half-life, t 1/2 , after administration of intravenous doses ranges between 2 and 3.6 hours. Excretion Budesonide is excreted in urine and feces in the form of metabolites. After oral as well as intravenous administration of micronized [ 3 H]-budesonide, approximately 60% of the recovered radioactivity is found in urine. The major metabolites, including 6β-hydroxy budesonide and 16α-hydroxy prednisolone, are mainly renally excreted, intact or in conjugated forms. No unchanged budesonide is detected in urine. Specific Populations Patients with Renal Impairment The pharmacokinetics of budesonide in patients with renal impairment have not been studied. Intact budesonide is not renally excreted, but metabolites are to a large extent, and might therefore reach higher levels in patients with impaired renal function. However, these metabolites have negligible corticosteroid activity as compared with budesonide (< 1/100). Patients with Hepatic Impairment In patients with liver cirrhosis, systemic availability of orally administered budesonide correlates with disease severity and is, on average, 2.5-fold higher compared with healthy controls. Patients with mild liver disease are minimally affected. Patients with severe liver dysfunction were not studied. Absorption parameters were not altered, and for the intravenous dose, no significant differences in CL or V SS were observed. Drug Interaction Studies Budesonide is metabolized via CYP3A4. Potent inhibitors of CYP3A4 can increase the plasma levels of budesonide several-fold. Co-administration of ketoconazole results in an eight-fold increase in AUC of budesonide, compared to budesonide alone. Grapefruit juice, an inhibitor of gut mucosal CYP3A, approximately doubles the systemic exposure of oral budesonide. Conversely, induction of CYP3A4 can result in the lowering of budesonide plasma levels [see Dosage and Administration (2) and Drug Interactions (7) ]. Oral contraceptives containing ethinyl estradiol, which are also metabolized by CYP3A4, do not affect the pharmacokinetics of budesonide. Budesonide does not affect the plasma levels of oral contraceptives (i.e., ethinyl estradiol).
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS Budesonide extended-release tablets are contraindicated in patients with hypersensitivity to budesonide or any of the ingredients of budesonide extended-release tablets. Anaphylactic reactions have occurred with other budesonide formulations [see Adverse Reactions (6.2) ] . • Known hypersensitivity to budesonide or any of the ingredients in budesonide extended-release tablets ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION Budesonide extended-release tablets, for oral administration, contain budesonide, a synthetic corticosteroid, as the active ingredient. Budesonide is designated chemically as (R,S)-11ß,16α,17,21-tetrahydroxypregna-1,4-diene-3,20-dionecyclic-16,17-acetal with butyraldehyde. Budesonide is provided as a mixture of two epimers (22R and 22S). The empirical formula of budesonide is C 25 H 34 O 6 and its molecular weight is 430.53. Its structural formula is: Budesonide, USP is a white or almost white crystalline odorless powder that is practically insoluble in water, sparingly soluble in alcohol, and freely soluble in chloroform. Budesonide, a delayed and extended-release tablet, is coated with a polymer film, which breaks down at or above pH 7. The tablet core contains budesonide with polymers that provide for extended release of budesonide. Each tablet contains the following inactive ingredients: colloidal silicon dioxide, hydroxypropyl cellulose, hypromellose, lactose monohydrate, magnesium stearate, methacrylic acid copolymer type A and type B, microcrystalline cellulose, polyethylene glycol, polydextrose, talc, titanium dioxide, triacetin and triethyl citrate. In addition, the black imprinting ink contains black iron oxide, hypromellose and propylene glycol. Budesonide Structural Formula
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION The recommended dosage for the induction of remission in adult patients with active, mild to moderate ulcerative colitis is one 9 mg tablet to be taken once daily in the morning with or without food for up to 8 weeks. ( 2.1 ) 2.1 Mild to Moderate Ulcerative Colitis The recommended dosage for the induction of remission in adult patients with active, mild to moderate ulcerative colitis is 9 mg taken orally once daily in the morning with or without food for up to 8 weeks. Budesonide extended-release tablets should be swallowed whole and not chewed, crushed or broken. 2.2 CYP3A4 Inhibitors If concomitant administration with ketoconazole, or any other CYP3A4 inhibitor, is indicated, patients should be closely monitored for increased signs and/or symptoms of hypercorticism. Avoid grapefruit juice, which is known to inhibit CYP3A4, when taking budesonide extended-release tablets. In these cases, discontinuation of budesonide extended-release tablets or the CYP3A4 inhibitor should be considered [see Drug Interactions (7) and Clinical Pharmacology (12.3) ] .
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Budesonide Extended-Release Tablets are available containing 9 mg of budesonide, USP. • The 9 mg tablets are white, film-coated, round, unscored tablets with M over BE9 imprinted in black ink on one side of the tablet and blank on the other side. Extended-release tablets: 9 mg ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE Budesonide extended-release tablets are indicated for the induction of remission in patients with active, mild to moderate ulcerative colitis. Budesonide extended-release tablets are a glucocorticosteroid indicated for the induction of remission in patients with active, mild to moderate ulcerative colitis. ( 1 )
Spl product data elements
Usually a list of ingredients in a drug product.Budesonide Budesonide BUDESONIDE BUDESONIDE FERROSOFERRIC OXIDE SILICON DIOXIDE HYDROXYPROPYL CELLULOSE (90000 WAMW) HYPROMELLOSE 2910 (6 MPA.S) HYPROMELLOSE 2910 (3 MPA.S) HYPROMELLOSE 2910 (50 MPA.S) LACTOSE MONOHYDRATE MAGNESIUM STEARATE METHACRYLIC ACID - METHYL METHACRYLATE COPOLYMER (1:1) METHACRYLIC ACID - METHYL METHACRYLATE COPOLYMER (1:2) MICROCRYSTALLINE CELLULOSE 101 MICROCRYSTALLINE CELLULOSE 102 POLYETHYLENE GLYCOL 8000 POLYETHYLENE GLYCOL 400 POLYDEXTROSE PROPYLENE GLYCOL TALC TITANIUM DIOXIDE TRIACETIN TRIETHYL CITRATE M;BE9
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenicity Carcinogenicity studies with budesonide were conducted in rats and mice. In a two-year study in Sprague-Dawley rats, budesonide caused a statistically significant increase in the incidence of gliomas in male rats at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). In addition, there were increased incidences of primary hepatocellular tumors in male rats at 25 mcg/kg (approximately 0.023 times the maximum recommended human dose on a body surface area basis) and above. No tumorigenicity was seen in female rats at oral doses up to 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). In an additional two-year study in male Sprague-Dawley rats, budesonide caused no gliomas at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). However, it caused a statistically significant increase in the incidence of hepatocellular tumors at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). The concurrent reference glucocorticosteroids (prednisolone and triamcinolone acetonide) showed similar findings. In a 91-week study in mice, budesonide caused no treatment-related carcinogenicity at oral doses up to 200 mcg/kg (approximately 0.1 times the maximum recommended human dose on a body surface area basis). Mutagenesis Budesonide was not genotoxic in the Ames test, the mouse lymphoma cell forward gene mutation (TK +/- ) test, the human lymphocyte chromosome aberration test, the Drosophila melanogaster sex-linked recessive lethality test, the rat hepatocycte unscheduled DNA synthesis (UDS) test and the mouse micronucleus test. Impairment of Fertility In rats, budesonide had no effect on fertility at subcutaneous doses up to 80 mcg/kg (approximately 0.07 times the maximum recommended human dose on a body surface area basis). However, it caused a decrease in prenatal viability and viability in pups at birth and during lactation, along with a decrease in maternal body weight gain, at subcutaneous doses of 20 mcg/kg (approximately 0.02 times the maximum recommended human dose on a body surface area basis) and above. No such effects were noted at 5 mcg/kg (approximately 0.005 times the maximum recommended human dose on a body surface area basis).
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenicity Carcinogenicity studies with budesonide were conducted in rats and mice. In a two-year study in Sprague-Dawley rats, budesonide caused a statistically significant increase in the incidence of gliomas in male rats at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). In addition, there were increased incidences of primary hepatocellular tumors in male rats at 25 mcg/kg (approximately 0.023 times the maximum recommended human dose on a body surface area basis) and above. No tumorigenicity was seen in female rats at oral doses up to 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). In an additional two-year study in male Sprague-Dawley rats, budesonide caused no gliomas at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). However, it caused a statistically significant increase in the incidence of hepatocellular tumors at an oral dose of 50 mcg/kg (approximately 0.05 times the maximum recommended human dose on a body surface area basis). The concurrent reference glucocorticosteroids (prednisolone and triamcinolone acetonide) showed similar findings. In a 91-week study in mice, budesonide caused no treatment-related carcinogenicity at oral doses up to 200 mcg/kg (approximately 0.1 times the maximum recommended human dose on a body surface area basis). Mutagenesis Budesonide was not genotoxic in the Ames test, the mouse lymphoma cell forward gene mutation (TK +/- ) test, the human lymphocyte chromosome aberration test, the Drosophila melanogaster sex-linked recessive lethality test, the rat hepatocycte unscheduled DNA synthesis (UDS) test and the mouse micronucleus test. Impairment of Fertility In rats, budesonide had no effect on fertility at subcutaneous doses up to 80 mcg/kg (approximately 0.07 times the maximum recommended human dose on a body surface area basis). However, it caused a decrease in prenatal viability and viability in pups at birth and during lactation, along with a decrease in maternal body weight gain, at subcutaneous doses of 20 mcg/kg (approximately 0.02 times the maximum recommended human dose on a body surface area basis) and above. No such effects were noted at 5 mcg/kg (approximately 0.005 times the maximum recommended human dose on a body surface area basis).
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PRINCIPAL DISPLAY PANEL – 9 mg NDC 0378-4500-93 Budesonide Extended-Release Tablets 9 mg Swallow tablet whole, do not chew, crush, or break. Rx only 30 Tablets Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure. Keep container tightly closed. Keep this and all medication out of the reach of children. Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.] Protect from light and moisture. Usual Dosage: One tablet daily. See accompanying prescribing information. Budesonide extended-release tablets should be swallowed whole and not chewed, crushed, or broken. Manufactured for: Mylan Pharmaceuticals Inc., a Viatris Company Morgantown, WV 26505 U.S.A. Each extended-release tablet contains: Budesonide, USP 9 mg RM4500HX Budesonide Extended-Release Tablets 9 mg Carton Label
Recent major changes
A list of the section(s) that contain substantive changes that have been approved by FDA in the product labeling. The headings and subheadings, if appropriate, affected by the change are listed together with each section’s identifying number and the month and year on which the change was incorporated in the labeling.Warnings and Precautions, Immunosuppression and Increased Risk of Infection ( 5.3 ) 06/2024 Kaposi’s Sarcoma ( 5.4 ) 06/2024
Budesonide: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Advise the patient to read the FDA-approved patient labeling (Patient Information). Patients treated with budesonide extended-release tablets should receive the following information and instructions. This information is intended to aid the patient in the safe and effective use of budesonide extended-release tablets. Hypercorticism and Adrenal Suppression Advise patients that budesonide extended-release tablets may cause systemic glucocorticosteroid effects of hypercorticism and adrenal suppression. Taper slowly from systemic corticosteroids if transferring to budesonide extended-release tablets [see Warnings and Precautions (5.1) and (5.2) ] . Immunosuppression and Increased Risk of Infection Advise patients to avoid exposure to people with varicella (chicken pox) or measles. Advise patients to inform their healthcare provider if they are exposed to varicella or measles or develop a new or worsening infection [(see Warnings and Precautions (5.3) ] . Kaposi’s Sarcoma Advise patients that Kaposi’s sarcoma has been reported in patients receiving corticosteroids for chronic conditions and to inform their healthcare provider if they experience signs or symptoms of Kaposi’s sarcoma [see Warnings and Precautions (5.4) ]. How to Take Budesonide Extended-Release Tablets Advise patients to swallow budesonide extended-release tablets whole with water. Do not chew or crush. Avoid the consumption of grapefruit juice for the duration of budesonide extended-release tablets therapy [see Dosage and Administration (2) ] . Pregnancy Advise female patients that budesonide extended-release tablets may cause fetal harm and to inform their healthcare provider with a known or suspected pregnancy [see Use in Specific Populations (8.1) ] .
Spl patient package insert
Information necessary for patients to use the drug safely and effectively.Patient Information Budesonide Extended-Release Tablets (bue desʹ oh nide) What are budesonide extended-release tablets? • Budesonide extended-release tablets are a prescription corticosteroid medicine used to help get active mild to moderate ulcerative colitis (UC) under control (induce remission). • It is not known if budesonide extended-release tablets are safe and effective in children. Who should not take budesonide extended-release tablets? Do not take budesonide extended-release tablets if: • you are allergic to budesonide or any of the ingredients in budesonide extended-release tablets. See the end of this leaflet for a complete list of ingredients in budesonide extended-release tablets. What should I tell my healthcare provider before taking budesonide extended-release tablets? Before you take budesonide extended-release tablets tell your healthcare provider about all of your medical conditions, including if you: • have liver problems. • are planning to have surgery. • have chickenpox or measles or have recently been near anyone with chickenpox or measles. • have an infection, including fungal and threadworm ( Strongyloides ) infections. • have or had a family history of diabetes, cataracts or glaucoma. • have or had tuberculosis. • have high blood pressure (hypertension). • have decreased bone mineral density (osteoporosis). • have stomach ulcers. • have malaria of the brain (cerebral malaria). • are pregnant or plan to become pregnant. Budesonide extended-release tablets may harm your unborn baby. Tell your healthcare provider if you are pregnant or think you are pregnant. • are breastfeeding or plan to breastfeed. Budesonide can pass into your breast milk and may harm your baby. You and your healthcare provider should decide if you will take budesonide extended-release tablets or breastfeed. You should not do both. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Budesonide extended-release tablets and other medicines may affect each other causing side effects. Especially tell your healthcare provider if you take another medicine that contains corticosteroids for other conditions, such as allergies or asthma. Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine. How should I take budesonide extended-release tablets? • Take budesonide extended-release tablets exactly as your healthcare provider tells you to take them. • Take budesonide extended-release tablets 1 time each day in the morning with or without food. • Take budesonide extended-release tablets whole with water. Do not chew, crush, or break budesonide extended-release tablets before swallowing. • If you take too many budesonide extended-release tablets, call your healthcare provider right away or go to the nearest hospital emergency room. What should I avoid while taking budesonide extended-release tablets? • Do not eat grapefruit or drink grapefruit juice while taking budesonide extended-release tablets. Eating grapefruit or drinking grapefruit juice can increase the level of budesonide in your blood. What are the possible side effects of budesonide extended-release tablets? Budesonide extended-release tablets may cause serious side effects, including: • Effects of having too much corticosteroid medicine in your blood (hypercorticism). Long-time use of budesonide extended-release tablets can cause you to have too much glucocorticosteroid medicine in your blood. Tell your healthcare provider if you have any of the following signs and symptoms of hypercorticism: o acne o bruise easily o rounding of your face (moon face) o ankle swelling o thicker or more hair on your body and face o a fatty pad or hump between your shoulders (buffalo hump) o pink or purple stretch marks on the skin of your abdomen, thighs, breasts and arms • Adrenal suppression. When budesonide extended-release tablets are taken for a long period of time (chronic use), the adrenal glands do not make enough steroid hormones (adrenal suppression). Tell your healthcare provider if you are under stress or have any symptoms of adrenal suppression during treatment with budesonide extended-release tablets including: o tiredness o weakness o nausea o vomiting o low blood pressure • Decreased ability of your body to fight infections (immunosuppression) and increased risk of infection. Corticosteroid medicines, including budesonide extended-release tablets, lower the ability of your immune system to fight infections and increase the risk of infections caused by viruses, bacteria, fungi, protozoan, or certain parasites. Corticosteroid medicines, including budesonide extended-release tablets, can also: o make current infections worse o increase the risk of infections spreading (disseminated) o increase the risk of making infections active again or making infections worse that have not been active (latent) o hide (mask) some signs of infection These infections can be mild but can be severe and lead to death. Your healthcare provider should check you closely for signs and symptoms of an infection while taking budesonide extended-release tablets. Tell you healthcare provider right away about any signs or symptoms of a new or worsening infection while taking budesonide extended-release tablets, including flu-like symptoms such as: o fever o chills o stomach area (abdominal) pain o aches o diarrhea o cough o pain o feeling tired o nausea and vomiting o Tuberculosis: If you have inactive (latent) tuberculosis, your tuberculosis may become active again while taking budesonide extended-release tablets. Your healthcare provider should check you closely for signs and symptoms of tuberculosis while taking budesonide extended-release tablets. o Chickenpox and measles: People taking corticosteroid medicines, including budesonide extended-release tablets, who have not had chickenpox or measles, should avoid contact with people who have these diseases. Tell your healthcare provider right away if you come in contact with anyone who has chickenpox or measles. o Hepatitis B virus (HBV) reactivation: If you are a carrier of HBV, the virus can become an active infection again while taking budesonide extended-release tablets. Your healthcare provider will test you for HBV before you start taking budesonide extended-release tablets. o Amebiasis: Inactive (latent) amebiasis may become an active infection while taking budesonide extended-release tablets. Your healthcare provider should check you for amebiasis before you start taking budesonide extended-release tablets in people who have spent time in the tropics or have unexplained diarrhea. • Kaposi’s sarcoma. Kaposi’s sarcoma has happened in people who received corticosteroid therapy, most often for treatment of long-lasting (chronic) conditions. • Worsening of allergies. If you take certain other corticosteroid medicines to treat allergies, switching to budesonide extended-release tablets may cause your allergies to come back. These allergies may include eczema (a skin disease) or rhinitis (inflammation inside your nose). Tell your healthcare provider if any of your allergies become worse while taking budesonide extended-release tablets. The most common side effects of budesonide extended-release tablets include: • headache • nausea • decreased blood • cortisol levels • stomach-area pain • tiredness • stomach or intestinal gas • bloating • acne • urinary tract infection • joint pain • constipation Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of budesonide extended-release tablets. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. How should I store budesonide extended-release tablets? • Store budesonide extended-release tablets at room temperature, between 20° to 25°C (68° to 77°F). • Keep the bottle tightly closed to protect budesonide extended-release tablets from light and moisture. Keep budesonide extended-release tablets and all medicines out of the reach of children. General information about the safe and effective use of budesonide extended-release tablets. Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use budesonide extended-release tablets for a condition for which they were not prescribed. Do not give budesonide extended-release tablets to other people, even if they have the same symptoms you have. They may harm them. You can ask your healthcare provider or pharmacist for information about budesonide extended-release tablets that is written for health professionals. For more information, call Viatris at 1-877-446-3679 (1-877-4-INFO-RX). What are the ingredients in budesonide extended-release tablets? Active ingredient: budesonide Inactive ingredients: colloidal silicon dioxide, hydroxypropyl cellulose, hypromellose, lactose monohydrate, magnesium stearate, methacrylic acid copolymer type A and type B, microcrystalline cellulose, polyethylene glycol, polydextrose, talc, titanium dioxide, triacetin and triethyl citrate. In addition, the black imprinting ink contains black iron oxide, hypromellose and propylene glycol. Manufactured for: Mylan Pharmaceuticals Inc., a Viatris Company, Morgantown, WV 26505 U.S.A. This Patient Information has been approved by the U.S. Food and Drug Administration. Manufactured for: Mylan Pharmaceuticals Inc., a Viatris Company Morgantown, WV 26505 U.S.A. Revised: 8/2024 BUDEERT:RX
| |
| |
| |
| |
| |
| |
|
|
| |
|
|
| |
|
|
| |
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES Induction of Remission in Active, Mild to Moderate Ulcerative Colitis Two similarly designed, randomized, double-blind, placebo-controlled studies were conducted in a total of 970 adult patients with active, mild to moderate ulcerative colitis (UC) which was defined as an Ulcerative Colitis Disease Activity Index (UCDAI of ≥ 4 and ≤ 10). Eight hundred ninety-nine of these patients had histology consistent with active UC; this was considered the primary analysis population. UCDAI is a four-component scale (total score of 0 to 12) that encompasses the clinical assessments of stool frequency, rectal bleeding, mucosal appearance and physician’s rating of disease activity (score of 0 to 3 for each of the components). The baseline median UCDAI score in both studies was 7. In Study 1, 56% of patients were male, and the median age was 42 years. In Study 2, 57% of patients were male, and the median age was 44 years. In Study 1, 50% of patients were Caucasian, 7% were African American, and 34% were Asian. In Study 2, more than 99% were Caucasian. Both studies compared budesonide extended-release tablets 9 mg and 6 mg with placebo and included an active reference arm (a mesalamine 2.4 g in Study 1 and a budesonide * 9 mg not approved for the treatment of UC in Study 2). The primary endpoint was induction of remission after 8 weeks of treatment. Remission was defined as a UCDAI score of ≤ 1, with subscores of 0 for rectal bleeding, stool frequency, and mucosal appearance and with a ≥ 1 point reduction in an endoscopy-only score. In both studies, budesonide 9 mg extended-release tablets demonstrated superiority to placebo in inducing remission (Table 4). Table 4. Induction of Remission in Studies 1 and 2 Treatment Group The primary analysis population included only patients that had histology consistent with active UC. CI = Confidence Interval Treatment Group Study 1 n/N (%) Study 2 n/N (%) Budesonide Extended-Release Tablets 9 mg 22/123 (17.9) 19/109 (17.4) Budesonide Extended-Release Tablets 6 mg 16/121 (13.2) 9/109 (8.3) Reference arm The reference arm in Study 1 is a delayed release mesalamine 2.4 g; the reference arm in Study 2 is a budesonide 9 mg not approved for the treatment of UC. 15/124 (12.1) 13/103 (12.6) Placebo 9/121 (7.4) 4/89 (4.5) Treatment difference between budesonide extended-release tablets 9 mg and placebo (95% CI) p < 0.025 for budesonide extended-release tablets 9 mg vs. placebo in both Studies 1 and 2 based on the Chi-square test (alpha = 0.025) 10.4% (2.2%, 18.7%) 12.9% (4.6%, 21.3%)
| The primary analysis population included only patients that had histology consistent with active UC. | ||
| CI = Confidence Interval | ||
References
This field may contain references when prescription drug labeling must summarize or otherwise relay on a recommendation by an authoritative scientific body, or on a standardized methodology, scale, or technique, because the information is important to prescribing decisions.15 REFERENCES 1. Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ . 1989;298: 82-86.
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use Clinical studies of budesonide extended-release tablets did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, budesonide extended-release tablets should be used cautiously in elderly patients due to the potential for decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use Safety and effectiveness of budesonide extended-release tablets in pediatric patients have not been established. Glucocorticosteroids, such as budesonide extended-release tablets, may cause a reduction of growth velocity in pediatric patients.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Risk Summary Limited published studies report on the use of budesonide in pregnant women; however, the data are insufficient to inform a drug-associated risk for major birth defects and miscarriage. There are clinical considerations (see Clinical Considerations ). In animal reproduction studies with pregnant rats and rabbits, subcutaneous administration of budesonide during organogenesis at doses 0.5 times and 0.05 times, respectively, the maximum recommended human dose, resulted in increased fetal loss, decreased pup weights, and skeletal abnormalities. Maternal toxicity was observed in both rats and rabbits at these dose levels ( see Data ). Based on animal data, advise pregnant women of the potential risk to a fetus. The estimated background risk of major birth defects and miscarriage of the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4%, and 15% to 20%, respectively. Clinical Considerations Disease-Associated Maternal and/or Embryofetal Risk Published data suggest that increased disease activity is associated with the risk of developing adverse pregnancy outcomes in women with ulcerative colitis. Adverse pregnancy outcomes include preterm delivery (before 37 weeks of gestation), low birth weight (less than 2500 g) infants, and small for gestational age at birth. Fetal/Neonatal Adverse Reactions Hypoadrenalism may occur in infants born of mothers receiving corticosteroids during pregnancy. Infants should be carefully observed for signs of hypoadrenalism, such as poor feeding, irritability, weakness, and vomiting, and managed accordingly [see Warnings and Precautions (5.1) ] . Data Animal Data Budesonide was teratogenic and embryolethal in rabbits and rats. In an embryofetal development study in pregnant rats dosed subcutaneously with budesonide during the period of organogenesis from gestation days 6-15 there were effects on fetal development and survival at subcutaneous doses up to approximately 500 mcg/kg in rats (approximately 0.5 times the maximum recommended human dose on a body surface area basis). In an embryofetal development study in pregnant rabbits dosed during the period of organogenesis from gestation days 6-18, there was an increase in maternal abortion, and effects on fetal development and reduction in litter weights at subcutaneous doses up to approximately 25 mcg/kg in rabbits (approximately 0.05 times the maximum recommended human dose on a body surface area basis). Maternal toxicity, including reduction in body weight gain, was observed at subcutaneous doses of 5 mcg/kg in rabbits (approximately 0.01 times the maximum recommended human dose on a body surface area basis) and 500 mcg/kg in rats (approximately 0.5 times the maximum recommended human dose on a body surface area basis). In a peri- and postnatal development study, rats dosed subcutaneously with budesonide during the period of Day 15 post coitum to Day 21 postpartum, budesonide had no effects on delivery but did have an effect on growth and development of offspring. In addition, offspring survival was reduced, and surviving offspring had decreased mean body weights at birth and during lactation at exposures 0.02 times the MRHD (on a mg/m 2 basis at maternal subcutaneous doses of 20 mcg/kg/day and higher). These findings occurred in the presence of maternal toxicity.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS • Pregnancy : Based on animal data, may cause fetal harm. ( 8.1 ) • Hepatic Impairment : Monitor patients for signs and/or symptoms of hypercorticism. ( 5.5 , 8.6 ) 8.1 Pregnancy Risk Summary Limited published studies report on the use of budesonide in pregnant women; however, the data are insufficient to inform a drug-associated risk for major birth defects and miscarriage. There are clinical considerations (see Clinical Considerations ). In animal reproduction studies with pregnant rats and rabbits, subcutaneous administration of budesonide during organogenesis at doses 0.5 times and 0.05 times, respectively, the maximum recommended human dose, resulted in increased fetal loss, decreased pup weights, and skeletal abnormalities. Maternal toxicity was observed in both rats and rabbits at these dose levels ( see Data ). Based on animal data, advise pregnant women of the potential risk to a fetus. The estimated background risk of major birth defects and miscarriage of the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4%, and 15% to 20%, respectively. Clinical Considerations Disease-Associated Maternal and/or Embryofetal Risk Published data suggest that increased disease activity is associated with the risk of developing adverse pregnancy outcomes in women with ulcerative colitis. Adverse pregnancy outcomes include preterm delivery (before 37 weeks of gestation), low birth weight (less than 2500 g) infants, and small for gestational age at birth. Fetal/Neonatal Adverse Reactions Hypoadrenalism may occur in infants born of mothers receiving corticosteroids during pregnancy. Infants should be carefully observed for signs of hypoadrenalism, such as poor feeding, irritability, weakness, and vomiting, and managed accordingly [see Warnings and Precautions (5.1) ] . Data Animal Data Budesonide was teratogenic and embryolethal in rabbits and rats. In an embryofetal development study in pregnant rats dosed subcutaneously with budesonide during the period of organogenesis from gestation days 6-15 there were effects on fetal development and survival at subcutaneous doses up to approximately 500 mcg/kg in rats (approximately 0.5 times the maximum recommended human dose on a body surface area basis). In an embryofetal development study in pregnant rabbits dosed during the period of organogenesis from gestation days 6-18, there was an increase in maternal abortion, and effects on fetal development and reduction in litter weights at subcutaneous doses up to approximately 25 mcg/kg in rabbits (approximately 0.05 times the maximum recommended human dose on a body surface area basis). Maternal toxicity, including reduction in body weight gain, was observed at subcutaneous doses of 5 mcg/kg in rabbits (approximately 0.01 times the maximum recommended human dose on a body surface area basis) and 500 mcg/kg in rats (approximately 0.5 times the maximum recommended human dose on a body surface area basis). In a peri- and postnatal development study, rats dosed subcutaneously with budesonide during the period of Day 15 post coitum to Day 21 postpartum, budesonide had no effects on delivery but did have an effect on growth and development of offspring. In addition, offspring survival was reduced, and surviving offspring had decreased mean body weights at birth and during lactation at exposures 0.02 times the MRHD (on a mg/m 2 basis at maternal subcutaneous doses of 20 mcg/kg/day and higher). These findings occurred in the presence of maternal toxicity. 8.2 Lactation Risk Summary Lactation studies have not been conducted with budesonide extended-release tablets or other oral budesonide products and no information is available on the effects of budesonide on the breastfed infant or the effects of the drug on milk production. One published study reports that budesonide is present in human milk following maternal inhalation of budesonide (see Data ) . The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for budesonide extended-release tablets and any potential adverse effects on the breastfed infant from budesonide extended-release tablets, or from the underlying maternal condition. Data One published study reports that budesonide is present in human milk following maternal inhalation of budesonide which resulted in infant doses approximately 0.3% to 1% of the maternal weight-adjusted dosage and a milk/plasma ratio ranging between 0.4 and 0.5. Budesonide plasma concentrations were not detected, and no adverse events were noted in the breastfed infants following maternal use of inhaled budesonide. The recommended daily dose of budesonide extended-release tablets is higher (9 mg daily) compared with inhaled budesonide (up to 800 mcg daily) given to mothers in the above described study. The maximum budesonide plasma concentration following a 9 mg daily dose (in both single- and repeated-dose pharmacokinetic studies) of oral budesonide is approximately 5 to 10 nmol/L which is up to 10 times higher than the 1 to 2 nmol/L for a 800 mcg daily dose of inhaled budesonide at steady state in the above inhalation study. Assuming the coefficient of extrapolation between the inhaled and oral doses is constant across all dose levels, at therapeutic doses of budesonide extended-release tablets, budesonide exposure to the nursing child may be up to 10 times higher than that by budesonide inhalation. 8.4 Pediatric Use Safety and effectiveness of budesonide extended-release tablets in pediatric patients have not been established. Glucocorticosteroids, such as budesonide extended-release tablets, may cause a reduction of growth velocity in pediatric patients. 8.5 Geriatric Use Clinical studies of budesonide extended-release tablets did not include sufficient numbers of subjects aged 65 and older to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, budesonide extended-release tablets should be used cautiously in elderly patients due to the potential for decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. 8.6 Hepatic Impairment Patients with moderate to severe liver disease should be monitored for increased signs and/or symptoms of hypercorticism. Discontinuing the use of budesonide extended-release tablets should be considered in these patients [see Warnings and Precautions (5.5) ] .
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING Budesonide Extended-Release Tablets are available containing 9 mg of budesonide, USP. The 9 mg tablets are white, film-coated, round, unscored tablets with M over BE9 imprinted in black ink on one side of the tablet and blank on the other side. They are available as follows: NDC 0378-4500-93 bottles of 30 tablets Store at 20° to 25°C (68° to 77°F). [See USP Controlled Room Temperature.] Keep container tightly closed. Protect from light and moisture. Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API