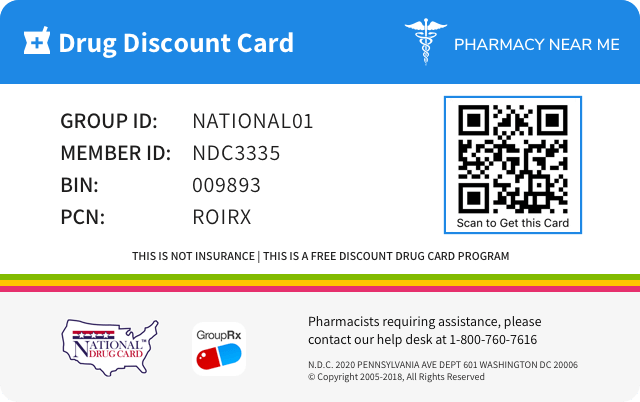
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 68180-863 | ||||
|---|---|---|---|---|---|
| Drug Name | Azithromycin dihydrate |
||||
| Type | Generic | ||||
| Pharm Class | Macrolide Antimicrobial [EPC], Macrolides [CS] |
||||
| Active Ingredients |
|
||||
| Route | ORAL | ||||
| Dosage Form | TABLET | ||||
| RxCUI drug identifier | 204844 | ||||
| Application Number | ANDA065400 | ||||
| Labeler Name | Lupin Pharmaceuticals, Inc. | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Overdosage of azithromycin dihydrate
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE Adverse reactions experienced in higher than recommended doses were similar to those seen at normal doses. In the event of overdosage, general symptomatic and supportive measures are indicated as required.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS The following clinically significant adverse reactions are described elsewhere in labeling: Hypersensitivity [see WARNINGS AND PRECAUTIONS ( 5.1 )] Hepatotoxicity [see WARNINGS AND PRECAUTIONS ( 5.2 )] Infantile Hypertrophic Pyloric Stenosis (IHPS) [see WARNINGS AND PRECAUTIONS ( 5.3 )] QT Prolongation [see WARNINGS AND PRECAUTIONS ( 5.4 )] Cardiovascular Death [see WARNINGS AND PRECAUTIONS ( 5.5 )] Clostridiodes difficile- Associated Diarrhea (CDAD) [see WARNINGS AND PRECAUTIONS ( 5.6 )] Exacerbation of Myasthenia Gravis [see WARNINGS AND PRECAUTIONS ( 5.7 )] The most common adverse reactions are diarrhea (5%), nausea (3%), abdominal pain (3%), or vomiting, (no percent given) ( 6 ) To report SUSPECTED ADVERSE REACTIONS, contact Lupin Pharmaceuticals, Inc. at 1-800-399-2561 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. In clinical trials, most of the reported adverse reactions were mild to moderate in severity and were reversible upon discontinuation of the drug. Approximately 0.7% of the patients from the multiple-dose clinical trials discontinued azithromycin therapy because of treatment-related adverse reactions. Serious adverse reactions included angioedema and cholestatic jaundice. Most of the adverse reactions leading to discontinuation were related to the gastrointestinal tract, e.g., nausea, vomiting, diarrhea, or abdominal pain. [see CLINICAL STUDIES ( 14.2 )] Multiple-dose regimen Overall, the most common adverse reactions in adult patients receiving a multiple-dose regimen of azithromycin were related to the gastrointestinal system with diarrhea/loose stools (5%), nausea (3%), and abdominal pain (3%) being the most frequently reported. No other adverse reactions occurred in patients on the multiple-dose regimen of azithromycin with a frequency greater than 1%. Adverse reactions that occurred with a frequency of 1% or less included the following: Cardiovascular: Palpitations and chest pain. Gastrointestinal: Dyspepsia, flatulence, vomiting, melena, and cholestatic jaundice. Genitourinary: Monilia, vaginitis, and nephritis. Nervous System: Dizziness, headache, vertigo, and somnolence. General: Fatigue. Allergic: Rash, photosensitivity, and angioedema. Chronic therapy with 1200 mg weekly regimen The nature of adverse reactions seen with the 1200 mg weekly dosing regimen for the prevention of Mycobacterium avium infection in severely immunocompromised HIV-infected patients were similar to those seen with short-term dosing regimens. [see CLINICAL STUDIES ( 14 )] Chronic therapy with 600 mg daily regimen combined with ethambutol The nature of adverse reactions seen with the 600 mg daily dosing regimen for the treatment of Mycobacterium avium complex infection in severely immunocompromised HIV-infected patients were similar to those seen with short term dosing regimens. Five percent of patients experienced reversible hearing impairment in the pivotal clinical trial for the treatment of disseminated MAC in patients with AIDS. Hearing impairment has been reported with macrolide antibiotics, especially at higher doses. Other treatment-related adverse reactions occurring in >5% of subjects and seen at any time during a median of 87.5 days of therapy include: abdominal pain (14%), nausea (14%), vomiting (13%), diarrhea (12%), flatulence (5%), headache (5%), and abnormal vision (5%). Discontinuations from treatment due to laboratory abnormalities or adverse reactions considered related to study drug occurred in 8 of 88 (9.1%) of subjects. 6.2 Postmarketing Experience The following adverse reactions have been identified during post approval use of azithromycin. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Adverse reactions reported with azithromycin during the postmarketing period in adult and/or pediatric patients for which a causal relationship may not be established include: Allergic Arthralgia, edema, urticaria, and angioedema. Cardiovascular Arrhythmias, including ventricular tachycardia, and hypotension. There have been reports of QT prolongation and torsades de pointes, and cardiovascular death. Gastrointestinal Anorexia, constipation, dyspepsia, flatulence, vomiting/diarrhea pseudomembranous colitis, pancreatitis, oral candidiasis, pyloric stenosis, and tongue discoloration. General Asthenia, paresthesia, fatigue, malaise, and anaphylaxis Genitourinary Interstitial nephritis, acute renal failure, and vaginitis. Hematopoietic Thrombocytopenia. Liver/Biliary Abnormal liver function, hepatitis, cholestatic jaundice, hepatic necrosis, and hepatic failure. [see WARNINGS AND PRECAUTIONS ( 5.2 )] . Nervous System Convulsions, dizziness/vertigo, headache, somnolence, hyperactivity, nervousness, agitation, and syncope. Psychiatric Aggressive reaction and anxiety. Skin/Appendages Pruritus, and serious skin reactions including erythema multiforme, AGEP, Stevens-Johnson Syndrome, toxic epidermal necrolysis, and DRESS. Special Senses Hearing disturbances including hearing loss, deafness, and/or tinnitus, and reports of taste/smell perversion and/or loss. 6.3 Laboratory Abnormalities Significant abnormalities (irrespective of drug relationship) occurring during the clinical trials were reported as follows: With an incidence of 1 to 2%, elevated serum creatine phosphokinase, potassium, ALT (SGPT), GGT, and AST (SGOT). With an incidence of less than 1%, leukopenia, neutropenia, decreased platelet count, elevated serum alkaline phosphatase, bilirubin, BUN, creatinine, blood glucose, LDH, and phosphate. When follow-up was provided, changes in laboratory tests appeared to be reversible. In multiple-dose clinical trials involving more than 3000 patients, 3 patients discontinued therapy because of treatment-related liver enzyme abnormalities and 1 because of a renal function abnormality. In a phase 1 drug interaction study performed in normal volunteers, 1 of 6 subjects given the combination of azithromycin and rifabutin, 1 of 7 given rifabutin alone, and 0 of 6 given azithromycin alone developed a clinically significant neutropenia (<500 cells/mm 3 ). Laboratory abnormalities seen in clinical trials for the prevention of disseminated Mycobacterium avium disease in severely immunocompromised HIV-infected patients. [see CLINICAL STUDIES ( 14 )] Chronic therapy (median duration: 87.5 days, range: 1 to 229 days) that resulted in laboratory abnormalities in >5% of subjects with normal baseline values in the pivotal trial for treatment of disseminated MAC in severely immunocompromised HIV - infected patients treated with azithromycin 600 mg daily in combination with ethambutol include: a reduction in absolute neutrophils to <50% of the lower limit of normal (10/52, 19%) and an increase to five times the upper limit of normal in alkaline phosphatase (3/35, 9%). These findings in subjects with normal baseline values are similar when compared to all subjects for analyses of neutrophil reductions (22/75, 29%) and elevated alkaline phosphatase (16/80, 20%). Causality of these laboratory abnormalities due to the use of study drug has not been established.
azithromycin dihydrate Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS Nelfinavir: Close monitoring for known side effects of azithromycin, such as liver enzyme abnormalities and hearing impairment, is warranted. ( 7.1 ) Warfarin: Use with azithromycin may increase coagulation times; monitor prothrombin time. ( 7.2 ) 7.1 Nelfinavir Co-administration of nelfinavir at steady-state with a single oral dose of azithromycin resulted in increased azithromycin serum concentrations. Although a dose adjustment of azithromycin is not recommended when administered in combination with nelfinavir, close monitoring for known adverse reactions of azithromycin, such as liver enzyme abnormalities and hearing impairment, is warranted. [see ADVERSE REACTIONS ( 6 )] 7.2 Warfarin Spontaneous postmarketing reports suggest that concomitant administration of azithromycin may potentiate the effects of oral anticoagulants such as warfarin, although the prothrombin time was not affected in the dedicated drug interaction study with azithromycin and warfarin. Prothrombin times should be carefully monitored while patients are receiving azithromycin and oral anticoagulants concomitantly. 7.3 Potential Drug-Drug Interaction with Macrolides Interactions digoxin, colchicine or phenytoin have not been reported in clinical trials with azithromycin. No specific drug interaction studies have been performed to evaluate potential drug-drug interaction. However, drug interactions have been observed with other macrolide products. Until further data are developed regarding drug interactions when digoxin, colchicine or phenytoin are used with azithromycin careful monitoring of patients is advised.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Azithromycin is a macrolide antibacterial drug. [see Microbiology ( 12.4 )] 12.2 Pharmacodynamics Based on animal models of infection, the antibacterial activity of azithromycin appears to correlate with the ratio of area under the concentration-time curve to minimum inhibitory concentration (AUC/MIC) for certain pathogens ( S. pneumoniae and S. aureus ). The principal pharmacokinetic/pharmacodynamic parameter best associated with clinical and microbiological cure has not been elucidated in clinical trials with azithromycin. Cardiac Electrophysiology QTc interval prolongation was studied in a randomized, placebo-controlled parallel trial in 116 healthy subjects who received either chloroquine (1000 mg) alone or in combination with oral azithromycin (500 mg, 1000 mg, and 1500 mg once daily). Co-administration of azithromycin increased the QTc interval in a dose-and concentration-dependent manner. In comparison to chloroquine alone, the maximum mean (95% upper confidence bound) increases in QTcF were 5 (10) ms, 7 (12) ms and 9 (14) ms with the co-administration of 500 mg, 1000 mg and 1500 mg azithromycin, respectively. 12.3 Pharmacokinetics The pharmacokinetic parameters of azithromycin in plasma after dosing as per labeled recommendations in healthy young adults and asymptomatic HIV-positive adults (age 18 to 40 years old) are portrayed in the following chart: MEAN (CV%) PK PARAMETER DOSE/DOSAGE FORM (serum, except as indicated) Subjects Day No. C max (mcg/mL) T max (hr) C 24 (mcg/mL) AUC (mcg • hr/mL) T ½ (hr) Urinary Excretion (% of dose) 500 mg/250 mg capsule 12 1 0.41 2.5 0.05 2.6 AUC 0 to 24 ; b 0-last. – 4.5 and 250 mg on Days 2 to 5 12 5 0.24 3.2 0.05 2.1 – 6.5 1200 mg/600 mg tablets 12 1 0.66 2.5 0.074 6.8 1 40 – %CV (62%) (79%) (49%) (64%) (33%) 600 mg tablet/day 7 1 0.33 2.0 0.039 2.4 %CV 25% (50%) (36%) (19%) 7 22 0.55 2.1 0.14 5.8 84.5 - %CV (18%) (52%) (26%) (25%) - 600 mg tablet/day (leukocytes) 7 22 252 10.9 146 4763 82.8 - %CV (49%) (28%) (33%) (42%) - - With a regimen of 500 mg on Day 1 and 250 mg/day on Days 2 to 5, C min and C max remained essentially unchanged from Day 2 through Day 5 of therapy. However, without a loading dose, azithromycin C min levels required 5 to 7 days to reach steady state. In asymptomatic HIV-positive adult subjects receiving 600 mg azithromycin tablets once daily for 22 days, steady state azithromycin serum levels were achieved by Day 15 of dosing. The high values in adults for apparent steady-state volume of distribution (31.1 L/kg) and plasma clearance (630 mL/min) suggest that the prolonged half-life is due to extensive uptake and subsequent release of drug from tissues. Absorption The 1 gram single - dose packet is bioequivalent to four 250 mg azithromycin capsule. When the oral suspension of azithromycin was administered with food, the C max increased by 46% and the AUC by 14%. The absolute bioavailability of two 600 mg tablets was 34% (CV=56%). Administration of two 600 mg tablets with food increased C max by 31% (CV=43%) while the extent of absorption (AUC) was unchanged (mean ratio of AUCs=1.00; CV=55%). Distribution The serum protein binding of azithromycin is variable in the concentration range approximating human exposure, decreasing from 51% at 0.02 mcg/mL to 7% at 2 mcg/mL. The antibacterial activity of azithromycin is pH related and appears to be reduced with decreasing pH. However, the extensive distribution of drug to tissues may be relevant to clinical activity. Azithromycin has been shown to penetrate into tissues in humans, including skin, lung, tonsil, and cervix. Extensive tissue distribution was confirmed by examination of additional tissues and fluids (bone, ejaculum, prostate, ovary, uterus, salpinx, stomach, liver, and gallbladder). As there are no data from adequate and well-controlled studies of azithromycin treatment of infections in these additional body sites, the clinical importance of these tissue concentration data is unknown. Azithromycin concentrates in phagocytes and fibroblasts as demonstrated by in vitro incubation techniques. Using such methodology, the ratio of intracellular to extracellular concentration was >30 after one hr of incubation. In vivo studies suggest that concentration in phagocytes may contribute to drug distribution to inflamed tissues. Following oral administration of a single 1200 mg dose (two 600 mg tablets), the mean maximum concentration in peripheral leukocytes was 140 mcg/mL. Concentration remained above 32 mcg/mL, for approximately 60 hr. The mean half-lives for 6 males and 6 females were 34 hr and 57 hr, respectively. Leukocyte-to-plasma C max ratios for males and females were 258 (±77%) and 175 (±60%), respectively, and the AUC ratios were 804 (±31%) and 541 (±28%) respectively. The clinical relevance of these findings is unknown. Following oral administration of multiple daily doses of 600 mg (1 tablet/day) to asymptomatic HIV-positive adults, mean maximum concentration in peripheral leukocytes was 252 mcg/mL (±49%). Trough concentrations in peripheral leukocytes at steady-state averaged 146 mcg/mL (±33%). The mean leukocyte-to-serum C max ratio was 456 (±38%) and the mean leukocyte to serum AUC ratio was 816 (±31%). The clinical relevance of these findings is unknown. Metabolism In vitro and in vivo studies to assess the metabolism of azithromycin have not been performed. Elimination Plasma concentrations of azithromycin following single 500 mg oral and IV doses declined in a polyphasic pattern resulting in an average terminal half-life of 68 hr. Biliary excretion of azithromycin, predominantly as unchanged drug, is a major route of elimination. Over the course of a week, approximately 6% of the administered dose appears as unchanged drug in urine. Specific Populations Patients with Renal Impairment: Azithromycin pharmacokinetics was investigated in 42 adults (21 to 85 years of age) with varying degrees of renal impairment. Following the oral administration of a single 1.0 g dose of azithromycin (4 × 250 mg capsules), the mean C max and AUC 0 to 120 increased by 5.1% and 4.2%, respectively, in subjects with GFR 10 to 80 mL/min compared to subjects with normal renal function (GFR >80 mL/min). The mean C max and AUC 0 to 120 increased 61% and 35%, respectively, in subjects with end-stage renal disease (GFR <10 mL/min) compared to subjects with normal renal function (GFR >80 mL/min ). Patients with Hepatic Impairment: The pharmacokinetics of azithromycin in subjects with hepatic impairment has not been established. Male and Female Patients: There are no significant differences in the disposition of azithromycin between male and female subjects. No dosage adjustment is recommended on the basis of gender. Geriatric Patients : Pharmacokinetic parameters in older volunteers (65 to 85 years old) were similar to those in younger volunteers (18 to 40 years old) for the 5-day therapeutic regimen. Dosage adjustment does not appear to be necessary for older patients with normal renal and hepatic function receiving treatment with this dosage regimen. [see Geriatric Use ( 8.5 )] Pediatric Patients: For information regarding the pharmacokinetics of azithromycin for oral suspension in pediatric patients, see the prescribing information for azithromycin for oral suspension 100 mg/5 mL and 200 mg/5 mL bottles. Drug Interaction Studies: Drug interaction studies were performed with azithromycin and other drugs likely to be co-administered. The effects of co-administration of azithromycin on the pharmacokinetics of other drugs are shown in Table 1 and the effects of other drugs on the pharmacokinetics of azithromycin are shown in Table 2. Co-administration of azithromycin at therapeutic doses had a modest effect on the pharmacokinetics of the drugs listed in Table 1. No dosage adjustment of drugs listed in Table 1 is recommended when co-administered with azithromycin. Co-administration of azithromycin with efavirenz or fluconazole had a modest effect on the pharmacokinetics of azithromycin. Nelfinavir significantly increased the C max and AUC of azithromycin. No dosage adjustment of azithromycin is recommended when administered with drugs listed in Table 2. [see DRUG INTERACTIONS ( 7.3 )] Table 1: Drug Interactions: Pharmacokinetic Parameters for Co-administered Drugs in the Presence of Azithromycin Co - administered Drug Dose of Co - administered Drug Dose of Azithromycin n Ratio ( with / without azithromycin ) of Co - administered Drug Pharmacokinetic Parameters ( 90 % CI ); No Effect = 1 . 00 Mean C m a x Mean AUC Atorvastatin 10 mg/day for 8 days 500 mg/day orally on days 6 to 8 12 0.83 (0.63 to 1.08) 1.01 (0.81 to 1.25) Carbamazepine 200 mg/day for 2 days, then 200 mg twice a day for 18 days 500 mg/day orally for days 16 to 18 7 0.97 (0.88 to 1.06) 0.96 (0.88 to 1.06) Cetirizine 20 mg/day for 11 days 500 mg orally on day 7, then 250 mg/day on days 8 to 11 14 1.03 (0.93 to 1.14) 1.02 (0.92 to 1.13) Didanosine 200 mg orally twice a day for 21 days 1,200 mg/day orally on days 8 to 21 6 1.44 (0.85 to 2.43) 1.14 (0.83 to 1.57) Efavirenz 400 mg/day for 7 days 600 mg orally on day 7 14 1.04 -90% Confidence interval not reported 0.95 Fluconazole 200 mg orally single dose 1,200 mg orally single dose 18 1.04 (0.98 to 1.11) 1.01 (0.97 to 1.05) Indinavir 800 mg three times a day for 5 days 1,200 mg orally on day 5 18 0.96 (0.86 to 1.08) 0.90 (0.81 to 1.00) Midazolam 15 mg orally on day 3 500 mg/day orally for 3 days 12 1.27 (0.89 to 1.81) 1.26 (1.01 to 1.56) Nelfinavir 750 mg three times a day for 11 days 1,200 mg orally on day 9 14 0.90 (0.81 to 1.01) 0.85 (0.78 to 0.93) Sildenafil 100 mg on days 1 and 4 500 mg/day orally for 3 days 12 1.16 (0.86 to 1.57) 0.92 (0.75 to 1.12) Theophylline 4 mg/kg IV on days 1, 11, 25 500 mg orally on day 7, 250 mg/day on days 8 to 11 10 1.19 (1.02 to 1.40) 1.02 (0.86 to 1.22) Theophylline 300 mg orally BID ×15 days 500 mg orally on day 6, then 250 mg/day on days 7 to 10 8 1.09 (0.92 to 1.29) 1.08 (0.89 to 1.31) Triazolam 0.125 mg on day 2 500 mg orally on day 1, then 250 mg/day on day 2 12 1.06 1.02 Trimethoprim/ Sulfamethoxazole 160 mg/800 mg/day orally for 7 days 1,200 mg orally on day 7 12 0.85 (0.75 to 0.97)/ 0.90 (0.78 to 1.03) 0.87 (0.80 to 0.95/ 0.96 (0.88 to 1.03) Zidovudine 500 mg/day orally for 21 days 600 mg/day orally for 14 days 5 1.12 (0.42 to 3.02) 0.94 (0.52 to 1.7) Zidovudine 500 mg/day orally for 21 days 1,200 mg/day orally for 14 days 4 1.31 (0.43 to 3.97) 1.30 (0.69 to 2.43) Table 2: Drug Interactions: Pharmacokinetic Parameters for Azithromycin in the Presence of Co-administered Drugs [see DRUG INTERACTIONS ( 7.3 )]. Co - administered Drug Dose of Co - administered Drug Dose of Azithromycin n Ratio ( with / without co - administered drug ) of Azithromycin Pharmacokinetic Parameters ( 90 % CI ); No Effect = 1 . 00 Mean C m a x Mean AUC Efavirenz 400 mg/day for 7 days 600 mg orally on day 7 14 1.22 (1.04 to 1.42) 0.92 -90% Confidence interval not reported Fluconazole 200 mg orally single dose 1,200 mg orally single dose 18 0.82 (0.66 to 1.02) 1.07 (0.94 to 1.22) Nelfinavir 750 mg three times a day for 11 days 1,200 mg orally on day 9 14 2.36 (1.77 to 3.15) 2.12 (1.80 to 2.50) 12.4 Microbiology Mechanism of Action Azithromycin acts by binding to the 23S rRNA of the 50S ribosomal subunit of susceptible microorganisms inhibiting bacterial protein synthesis and impeding the assembly of the 50S ribosomal subunit. Resistance The most frequently encountered mechanism of resistance to azithromycin is modification of the 23S rRNA target, most often by methylation. Ribosomal modifications can determine cross resistance to other macrolides, lincosamides, and streptogramin B (MLS B phenotype). The mechanism of acquired mutational resistance in isolates of Mycobacterium avium complex (i.e., 23S rRNA genemutation) is the same for both clarithromycin and azithromycin. Antimicrobial Activity Azithromycin has been shown to be active against the following microorganisms, both in vitro and in clinical infections. [see INDICATIONS AND USAGE ( 1 )] Mycobacteria Mycobacterium avium complex (MAC) consisting of: Mycobacterium avium Mycobacterium intracellulare Other Microorganisms Chlamydia trachomatis Susceptibility Testing For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
| 500 mg/250 mg capsule | 12 | 1 | 0.41 | 2.5 | 0.05 | 2.6 | – | 4.5 |
| and 250 mg on Days 2 to 5 | 12 | 5 | 0.24 | 3.2 | 0.05 | 2.1 | – | 6.5 |
| 1200 mg/600 mg tablets | 12 | 1 | 0.66 | 2.5 | 0.074 | 6.8 | 40 | – |
| %CV | (62%) | (79%) | (49%) | (64%) | (33%) | |||
| 600 mg tablet/day | 7 | 1 | 0.33 | 2.0 | 0.039 | 2.4 | ||
| %CV | 25% | (50%) | (36%) | (19%) | ||||
| 7 | 22 | 0.55 | 2.1 | 0.14 | 5.8 | 84.5 | - | |
| %CV | (18%) | (52%) | (26%) | (25%) | - | |||
| 600 mg tablet/day (leukocytes) | 7 | 22 | 252 | 10.9 | 146 | 4763 | 82.8 | - |
| %CV | (49%) | (28%) | (33%) | (42%) | - | - |
| Atorvastatin | 10 mg/day for 8 days | 500 mg/day orally on days 6 to 8 | 12 | 0.83 (0.63 to 1.08) | 1.01 (0.81 to 1.25) |
| Carbamazepine | 200 mg/day for 2 days, then 200 mg twice a day for 18 days | 500 mg/day orally for days 16 to 18 | 7 | 0.97 (0.88 to 1.06) | 0.96 (0.88 to 1.06) |
| Cetirizine | 20 mg/day for 11 days | 500 mg orally on day 7, then 250 mg/day on days 8 to 11 | 14 | 1.03 (0.93 to 1.14) | 1.02 (0.92 to 1.13) |
| Didanosine | 200 mg orally twice a day for 21 days | 1,200 mg/day orally on days 8 to 21 | 6 | 1.44 (0.85 to 2.43) | 1.14 (0.83 to 1.57) |
| Efavirenz | 400 mg/day for 7 days | 600 mg orally on day 7 | 14 | 1.04 | 0.95 |
| Fluconazole | 200 mg orally single dose | 1,200 mg orally single dose | 18 | 1.04 (0.98 to 1.11) | 1.01 (0.97 to 1.05) |
| Indinavir | 800 mg three times a day for 5 days | 1,200 mg orally on day 5 | 18 | 0.96 (0.86 to 1.08) | 0.90 (0.81 to 1.00) |
| Midazolam | 15 mg orally on day 3 | 500 mg/day orally for 3 days | 12 | 1.27 (0.89 to 1.81) | 1.26 (1.01 to 1.56) |
| Nelfinavir | 750 mg three times a day for 11 days | 1,200 mg orally on day 9 | 14 | 0.90 (0.81 to 1.01) | 0.85 (0.78 to 0.93) |
| Sildenafil | 100 mg on days 1 and 4 | 500 mg/day orally for 3 days | 12 | 1.16 (0.86 to 1.57) | 0.92 (0.75 to 1.12) |
| Theophylline | 4 mg/kg IV on days 1, 11, 25 | 500 mg orally on day 7, 250 mg/day on days 8 to 11 | 10 | 1.19 (1.02 to 1.40) | 1.02 (0.86 to 1.22) |
| Theophylline | 300 mg orally BID ×15 days | 500 mg orally on day 6, then 250 mg/day on days 7 to 10 | 8 | 1.09 (0.92 to 1.29) | 1.08 (0.89 to 1.31) |
| Triazolam | 0.125 mg on day 2 | 500 mg orally on day 1, then 250 mg/day on day 2 | 12 | 1.06 | 1.02 |
| Trimethoprim/ Sulfamethoxazole | 160 mg/800 mg/day orally for 7 days | 1,200 mg orally on day 7 | 12 | 0.85 (0.75 to 0.97)/ 0.90 (0.78 to 1.03) | 0.87 (0.80 to 0.95/ 0.96 (0.88 to 1.03) |
| Zidovudine | 500 mg/day orally for 21 days | 600 mg/day orally for 14 days | 5 | 1.12 (0.42 to 3.02) | 0.94 (0.52 to 1.7) |
| Zidovudine | 500 mg/day orally for 21 days | 1,200 mg/day orally for 14 days | 4 | 1.31 (0.43 to 3.97) | 1.30 (0.69 to 2.43) |
| Efavirenz | 400 mg/day for 7 days | 600 mg orally on day 7 | 14 | 1.22 (1.04 to 1.42) | 0.92 |
| Fluconazole | 200 mg orally single dose | 1,200 mg orally single dose | 18 | 0.82 (0.66 to 1.02) | 1.07 (0.94 to 1.22) |
| Nelfinavir | 750 mg three times a day for 11 days | 1,200 mg orally on day 9 | 14 | 2.36 (1.77 to 3.15) | 2.12 (1.80 to 2.50) |
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action Azithromycin is a macrolide antibacterial drug. [see Microbiology ( 12.4 )]
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Based on animal models of infection, the antibacterial activity of azithromycin appears to correlate with the ratio of area under the concentration-time curve to minimum inhibitory concentration (AUC/MIC) for certain pathogens ( S. pneumoniae and S. aureus ). The principal pharmacokinetic/pharmacodynamic parameter best associated with clinical and microbiological cure has not been elucidated in clinical trials with azithromycin. Cardiac Electrophysiology QTc interval prolongation was studied in a randomized, placebo-controlled parallel trial in 116 healthy subjects who received either chloroquine (1000 mg) alone or in combination with oral azithromycin (500 mg, 1000 mg, and 1500 mg once daily). Co-administration of azithromycin increased the QTc interval in a dose-and concentration-dependent manner. In comparison to chloroquine alone, the maximum mean (95% upper confidence bound) increases in QTcF were 5 (10) ms, 7 (12) ms and 9 (14) ms with the co-administration of 500 mg, 1000 mg and 1500 mg azithromycin, respectively.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics The pharmacokinetic parameters of azithromycin in plasma after dosing as per labeled recommendations in healthy young adults and asymptomatic HIV-positive adults (age 18 to 40 years old) are portrayed in the following chart: MEAN (CV%) PK PARAMETER DOSE/DOSAGE FORM (serum, except as indicated) Subjects Day No. C max (mcg/mL) T max (hr) C 24 (mcg/mL) AUC (mcg • hr/mL) T ½ (hr) Urinary Excretion (% of dose) 500 mg/250 mg capsule 12 1 0.41 2.5 0.05 2.6 AUC 0 to 24 ; b 0-last. – 4.5 and 250 mg on Days 2 to 5 12 5 0.24 3.2 0.05 2.1 – 6.5 1200 mg/600 mg tablets 12 1 0.66 2.5 0.074 6.8 1 40 – %CV (62%) (79%) (49%) (64%) (33%) 600 mg tablet/day 7 1 0.33 2.0 0.039 2.4 %CV 25% (50%) (36%) (19%) 7 22 0.55 2.1 0.14 5.8 84.5 - %CV (18%) (52%) (26%) (25%) - 600 mg tablet/day (leukocytes) 7 22 252 10.9 146 4763 82.8 - %CV (49%) (28%) (33%) (42%) - - With a regimen of 500 mg on Day 1 and 250 mg/day on Days 2 to 5, C min and C max remained essentially unchanged from Day 2 through Day 5 of therapy. However, without a loading dose, azithromycin C min levels required 5 to 7 days to reach steady state. In asymptomatic HIV-positive adult subjects receiving 600 mg azithromycin tablets once daily for 22 days, steady state azithromycin serum levels were achieved by Day 15 of dosing. The high values in adults for apparent steady-state volume of distribution (31.1 L/kg) and plasma clearance (630 mL/min) suggest that the prolonged half-life is due to extensive uptake and subsequent release of drug from tissues. Absorption The 1 gram single - dose packet is bioequivalent to four 250 mg azithromycin capsule. When the oral suspension of azithromycin was administered with food, the C max increased by 46% and the AUC by 14%. The absolute bioavailability of two 600 mg tablets was 34% (CV=56%). Administration of two 600 mg tablets with food increased C max by 31% (CV=43%) while the extent of absorption (AUC) was unchanged (mean ratio of AUCs=1.00; CV=55%). Distribution The serum protein binding of azithromycin is variable in the concentration range approximating human exposure, decreasing from 51% at 0.02 mcg/mL to 7% at 2 mcg/mL. The antibacterial activity of azithromycin is pH related and appears to be reduced with decreasing pH. However, the extensive distribution of drug to tissues may be relevant to clinical activity. Azithromycin has been shown to penetrate into tissues in humans, including skin, lung, tonsil, and cervix. Extensive tissue distribution was confirmed by examination of additional tissues and fluids (bone, ejaculum, prostate, ovary, uterus, salpinx, stomach, liver, and gallbladder). As there are no data from adequate and well-controlled studies of azithromycin treatment of infections in these additional body sites, the clinical importance of these tissue concentration data is unknown. Azithromycin concentrates in phagocytes and fibroblasts as demonstrated by in vitro incubation techniques. Using such methodology, the ratio of intracellular to extracellular concentration was >30 after one hr of incubation. In vivo studies suggest that concentration in phagocytes may contribute to drug distribution to inflamed tissues. Following oral administration of a single 1200 mg dose (two 600 mg tablets), the mean maximum concentration in peripheral leukocytes was 140 mcg/mL. Concentration remained above 32 mcg/mL, for approximately 60 hr. The mean half-lives for 6 males and 6 females were 34 hr and 57 hr, respectively. Leukocyte-to-plasma C max ratios for males and females were 258 (±77%) and 175 (±60%), respectively, and the AUC ratios were 804 (±31%) and 541 (±28%) respectively. The clinical relevance of these findings is unknown. Following oral administration of multiple daily doses of 600 mg (1 tablet/day) to asymptomatic HIV-positive adults, mean maximum concentration in peripheral leukocytes was 252 mcg/mL (±49%). Trough concentrations in peripheral leukocytes at steady-state averaged 146 mcg/mL (±33%). The mean leukocyte-to-serum C max ratio was 456 (±38%) and the mean leukocyte to serum AUC ratio was 816 (±31%). The clinical relevance of these findings is unknown. Metabolism In vitro and in vivo studies to assess the metabolism of azithromycin have not been performed. Elimination Plasma concentrations of azithromycin following single 500 mg oral and IV doses declined in a polyphasic pattern resulting in an average terminal half-life of 68 hr. Biliary excretion of azithromycin, predominantly as unchanged drug, is a major route of elimination. Over the course of a week, approximately 6% of the administered dose appears as unchanged drug in urine. Specific Populations Patients with Renal Impairment: Azithromycin pharmacokinetics was investigated in 42 adults (21 to 85 years of age) with varying degrees of renal impairment. Following the oral administration of a single 1.0 g dose of azithromycin (4 × 250 mg capsules), the mean C max and AUC 0 to 120 increased by 5.1% and 4.2%, respectively, in subjects with GFR 10 to 80 mL/min compared to subjects with normal renal function (GFR >80 mL/min). The mean C max and AUC 0 to 120 increased 61% and 35%, respectively, in subjects with end-stage renal disease (GFR <10 mL/min) compared to subjects with normal renal function (GFR >80 mL/min ). Patients with Hepatic Impairment: The pharmacokinetics of azithromycin in subjects with hepatic impairment has not been established. Male and Female Patients: There are no significant differences in the disposition of azithromycin between male and female subjects. No dosage adjustment is recommended on the basis of gender. Geriatric Patients : Pharmacokinetic parameters in older volunteers (65 to 85 years old) were similar to those in younger volunteers (18 to 40 years old) for the 5-day therapeutic regimen. Dosage adjustment does not appear to be necessary for older patients with normal renal and hepatic function receiving treatment with this dosage regimen. [see Geriatric Use ( 8.5 )] Pediatric Patients: For information regarding the pharmacokinetics of azithromycin for oral suspension in pediatric patients, see the prescribing information for azithromycin for oral suspension 100 mg/5 mL and 200 mg/5 mL bottles. Drug Interaction Studies: Drug interaction studies were performed with azithromycin and other drugs likely to be co-administered. The effects of co-administration of azithromycin on the pharmacokinetics of other drugs are shown in Table 1 and the effects of other drugs on the pharmacokinetics of azithromycin are shown in Table 2. Co-administration of azithromycin at therapeutic doses had a modest effect on the pharmacokinetics of the drugs listed in Table 1. No dosage adjustment of drugs listed in Table 1 is recommended when co-administered with azithromycin. Co-administration of azithromycin with efavirenz or fluconazole had a modest effect on the pharmacokinetics of azithromycin. Nelfinavir significantly increased the C max and AUC of azithromycin. No dosage adjustment of azithromycin is recommended when administered with drugs listed in Table 2. [see DRUG INTERACTIONS ( 7.3 )] Table 1: Drug Interactions: Pharmacokinetic Parameters for Co-administered Drugs in the Presence of Azithromycin Co - administered Drug Dose of Co - administered Drug Dose of Azithromycin n Ratio ( with / without azithromycin ) of Co - administered Drug Pharmacokinetic Parameters ( 90 % CI ); No Effect = 1 . 00 Mean C m a x Mean AUC Atorvastatin 10 mg/day for 8 days 500 mg/day orally on days 6 to 8 12 0.83 (0.63 to 1.08) 1.01 (0.81 to 1.25) Carbamazepine 200 mg/day for 2 days, then 200 mg twice a day for 18 days 500 mg/day orally for days 16 to 18 7 0.97 (0.88 to 1.06) 0.96 (0.88 to 1.06) Cetirizine 20 mg/day for 11 days 500 mg orally on day 7, then 250 mg/day on days 8 to 11 14 1.03 (0.93 to 1.14) 1.02 (0.92 to 1.13) Didanosine 200 mg orally twice a day for 21 days 1,200 mg/day orally on days 8 to 21 6 1.44 (0.85 to 2.43) 1.14 (0.83 to 1.57) Efavirenz 400 mg/day for 7 days 600 mg orally on day 7 14 1.04 -90% Confidence interval not reported 0.95 Fluconazole 200 mg orally single dose 1,200 mg orally single dose 18 1.04 (0.98 to 1.11) 1.01 (0.97 to 1.05) Indinavir 800 mg three times a day for 5 days 1,200 mg orally on day 5 18 0.96 (0.86 to 1.08) 0.90 (0.81 to 1.00) Midazolam 15 mg orally on day 3 500 mg/day orally for 3 days 12 1.27 (0.89 to 1.81) 1.26 (1.01 to 1.56) Nelfinavir 750 mg three times a day for 11 days 1,200 mg orally on day 9 14 0.90 (0.81 to 1.01) 0.85 (0.78 to 0.93) Sildenafil 100 mg on days 1 and 4 500 mg/day orally for 3 days 12 1.16 (0.86 to 1.57) 0.92 (0.75 to 1.12) Theophylline 4 mg/kg IV on days 1, 11, 25 500 mg orally on day 7, 250 mg/day on days 8 to 11 10 1.19 (1.02 to 1.40) 1.02 (0.86 to 1.22) Theophylline 300 mg orally BID ×15 days 500 mg orally on day 6, then 250 mg/day on days 7 to 10 8 1.09 (0.92 to 1.29) 1.08 (0.89 to 1.31) Triazolam 0.125 mg on day 2 500 mg orally on day 1, then 250 mg/day on day 2 12 1.06 1.02 Trimethoprim/ Sulfamethoxazole 160 mg/800 mg/day orally for 7 days 1,200 mg orally on day 7 12 0.85 (0.75 to 0.97)/ 0.90 (0.78 to 1.03) 0.87 (0.80 to 0.95/ 0.96 (0.88 to 1.03) Zidovudine 500 mg/day orally for 21 days 600 mg/day orally for 14 days 5 1.12 (0.42 to 3.02) 0.94 (0.52 to 1.7) Zidovudine 500 mg/day orally for 21 days 1,200 mg/day orally for 14 days 4 1.31 (0.43 to 3.97) 1.30 (0.69 to 2.43) Table 2: Drug Interactions: Pharmacokinetic Parameters for Azithromycin in the Presence of Co-administered Drugs [see DRUG INTERACTIONS ( 7.3 )]. Co - administered Drug Dose of Co - administered Drug Dose of Azithromycin n Ratio ( with / without co - administered drug ) of Azithromycin Pharmacokinetic Parameters ( 90 % CI ); No Effect = 1 . 00 Mean C m a x Mean AUC Efavirenz 400 mg/day for 7 days 600 mg orally on day 7 14 1.22 (1.04 to 1.42) 0.92 -90% Confidence interval not reported Fluconazole 200 mg orally single dose 1,200 mg orally single dose 18 0.82 (0.66 to 1.02) 1.07 (0.94 to 1.22) Nelfinavir 750 mg three times a day for 11 days 1,200 mg orally on day 9 14 2.36 (1.77 to 3.15) 2.12 (1.80 to 2.50)
| 500 mg/250 mg capsule | 12 | 1 | 0.41 | 2.5 | 0.05 | 2.6 | – | 4.5 |
| and 250 mg on Days 2 to 5 | 12 | 5 | 0.24 | 3.2 | 0.05 | 2.1 | – | 6.5 |
| 1200 mg/600 mg tablets | 12 | 1 | 0.66 | 2.5 | 0.074 | 6.8 | 40 | – |
| %CV | (62%) | (79%) | (49%) | (64%) | (33%) | |||
| 600 mg tablet/day | 7 | 1 | 0.33 | 2.0 | 0.039 | 2.4 | ||
| %CV | 25% | (50%) | (36%) | (19%) | ||||
| 7 | 22 | 0.55 | 2.1 | 0.14 | 5.8 | 84.5 | - | |
| %CV | (18%) | (52%) | (26%) | (25%) | - | |||
| 600 mg tablet/day (leukocytes) | 7 | 22 | 252 | 10.9 | 146 | 4763 | 82.8 | - |
| %CV | (49%) | (28%) | (33%) | (42%) | - | - |
| Atorvastatin | 10 mg/day for 8 days | 500 mg/day orally on days 6 to 8 | 12 | 0.83 (0.63 to 1.08) | 1.01 (0.81 to 1.25) |
| Carbamazepine | 200 mg/day for 2 days, then 200 mg twice a day for 18 days | 500 mg/day orally for days 16 to 18 | 7 | 0.97 (0.88 to 1.06) | 0.96 (0.88 to 1.06) |
| Cetirizine | 20 mg/day for 11 days | 500 mg orally on day 7, then 250 mg/day on days 8 to 11 | 14 | 1.03 (0.93 to 1.14) | 1.02 (0.92 to 1.13) |
| Didanosine | 200 mg orally twice a day for 21 days | 1,200 mg/day orally on days 8 to 21 | 6 | 1.44 (0.85 to 2.43) | 1.14 (0.83 to 1.57) |
| Efavirenz | 400 mg/day for 7 days | 600 mg orally on day 7 | 14 | 1.04 | 0.95 |
| Fluconazole | 200 mg orally single dose | 1,200 mg orally single dose | 18 | 1.04 (0.98 to 1.11) | 1.01 (0.97 to 1.05) |
| Indinavir | 800 mg three times a day for 5 days | 1,200 mg orally on day 5 | 18 | 0.96 (0.86 to 1.08) | 0.90 (0.81 to 1.00) |
| Midazolam | 15 mg orally on day 3 | 500 mg/day orally for 3 days | 12 | 1.27 (0.89 to 1.81) | 1.26 (1.01 to 1.56) |
| Nelfinavir | 750 mg three times a day for 11 days | 1,200 mg orally on day 9 | 14 | 0.90 (0.81 to 1.01) | 0.85 (0.78 to 0.93) |
| Sildenafil | 100 mg on days 1 and 4 | 500 mg/day orally for 3 days | 12 | 1.16 (0.86 to 1.57) | 0.92 (0.75 to 1.12) |
| Theophylline | 4 mg/kg IV on days 1, 11, 25 | 500 mg orally on day 7, 250 mg/day on days 8 to 11 | 10 | 1.19 (1.02 to 1.40) | 1.02 (0.86 to 1.22) |
| Theophylline | 300 mg orally BID ×15 days | 500 mg orally on day 6, then 250 mg/day on days 7 to 10 | 8 | 1.09 (0.92 to 1.29) | 1.08 (0.89 to 1.31) |
| Triazolam | 0.125 mg on day 2 | 500 mg orally on day 1, then 250 mg/day on day 2 | 12 | 1.06 | 1.02 |
| Trimethoprim/ Sulfamethoxazole | 160 mg/800 mg/day orally for 7 days | 1,200 mg orally on day 7 | 12 | 0.85 (0.75 to 0.97)/ 0.90 (0.78 to 1.03) | 0.87 (0.80 to 0.95/ 0.96 (0.88 to 1.03) |
| Zidovudine | 500 mg/day orally for 21 days | 600 mg/day orally for 14 days | 5 | 1.12 (0.42 to 3.02) | 0.94 (0.52 to 1.7) |
| Zidovudine | 500 mg/day orally for 21 days | 1,200 mg/day orally for 14 days | 4 | 1.31 (0.43 to 3.97) | 1.30 (0.69 to 2.43) |
| Efavirenz | 400 mg/day for 7 days | 600 mg orally on day 7 | 14 | 1.22 (1.04 to 1.42) | 0.92 |
| Fluconazole | 200 mg orally single dose | 1,200 mg orally single dose | 18 | 0.82 (0.66 to 1.02) | 1.07 (0.94 to 1.22) |
| Nelfinavir | 750 mg three times a day for 11 days | 1,200 mg orally on day 9 | 14 | 2.36 (1.77 to 3.15) | 2.12 (1.80 to 2.50) |
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS Patients with known hypersensitivity to azithromycin, erythromycin, any macrolide, or ketolide antibiotic. ( 4.1 ) Patients with a history of cholestatic jaundice/hepatic dysfunction associated with prior use of azithromycin. ( 4.2 ) 4.1 Hypersensitivity Azithromycin is contraindicated in patients with known hypersensitivity to azithromycin, erythromycin, any macrolide, or ketolide drug. 4.2 Hepatic Dysfunction Azithromycin is contraindicated in patients with a history of cholestatic jaundice/hepatic dysfunction associated with prior use of azithromycin.
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION Azithromycin tablets USP contain the active ingredient azithromycin, a macrolide antibacterial drug, for oral administration. Azithromycin has the chemical name ( 2R,3S,4R,5R,8R,10R,11R,12S,13S,14R )-13-[(2,6-dideoxy-3- C -methyl-3- O -methyl-α -L-ribo -hexopyranosyl)oxy]-2-ethyl-3,4,10-trihydroxy-3,5,6,8,10,12,14-heptamethyl-11-[[3,4,6-trideoxy-3-(dimethylamino)-β- D-xylo -hexopyranosyl]oxy]-1-oxa-6-azacyclopentadecan-15-one. Azithromycin is derived from erythromycin; however, it differs chemically from erythromycin in that a methyl-substituted nitrogen atom is incorporated into the lactone ring. Its molecular formula is C 38 H 72 N 2 O 12 , and its molecular weight is 749.0. Azithromycin has the following structural formula: Azithromycin, as the dihydrate, is a white to almost white crystalline powder with a molecular formula of C 38 H 72 N 2 O 12 •2H 2 O and a molecular weight of 785.02 Azithromycin tablets USP contain azithromycin dihydrate equivalent to 600 mg azithromycin. They also contain the following inactive ingredients: croscarmellose sodium, dibasic calcium phosphate, hydroxypropyl methyl cellulose, lactose monohydrate, magnesium stearate, sodium lauryl sulfate, titanium dioxide and triacetin. Organic Impurities Test Pending. Sturcture
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION Mycobacterial Infections ( 2.2 ) [see INDICATIONS AND USAGE ( 1 )] Azithromycin tablets can be taken with or without food. However, increased tolerability has been observed when tablets are taken with food. 2.2 Mycobacterial Infections Prevention of Disseminated MAC Infections The recommended dose of azithromycin for the prevention of disseminated Mycobacterium avium complex (MAC) disease is: 1200 mg taken once weekly. This dose of azithromycin may be combined with the approved dosage regimen of rifabutin. Treatment of Disseminated MAC Infections Azithromycin should be taken at a daily dose of 600 mg, in combination with ethambutol at the recommended daily dose of 15 mg/kg. Other antimycobacterial drugs that have shown in vitro activity against MAC may be added to the regimen of azithromycin plus ethambutol at the discretion of the physician or health care provider.
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Azithromycin tablets USP, 600 mg ( 3 ) Azithromycin Tablets USP, 600 mg are supplied as white, oval shaped film-coated tablets, engraved with "LU" on one side and "L06" on the other side containing azithromycin dihydrate equivalent to 600 mg of azithromycin USP. These are packaged in bottles of 30 tablets.
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE Azithromycin tablets are a macrolide antibacterial indicated for mild to moderate infections caused by designated, susceptible bacteria: Mycobacterial Infections ( 1.2 ) To reduce the development of drug-resistant bacteria and maintain the effectiveness of azithromycin tablets and other antibacterial drugs, azithromycin tablets should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. ( 1.3 ) Azithromycin tablets are a macrolide antibacterial drug indicated for the treatment of patients with mild to moderate infections caused by susceptible strains of the designated microorganisms in the specific conditions listed below. 1.2 Mycobacterial Infections Prophylaxis of Disseminated Mycobacterium avium complex (MAC) Disease Azithromycin tablets, taken alone or in combination with rifabutin at its approved dose, are indicated for the prevention of disseminated MAC disease in persons with advanced HIV infection [see DOSAGE AND ADMINISTRATION ( 2 )] . Treatment of Disseminated MAC Disease Azithromycin tablets, taken in combination with ethambutol, are indicated for the treatment of disseminated MAC infections in persons with advanced HIV infection [see USE IN SPECIFIC POPULATIONS ( 8.4 ) and CLINICAL STUDIES ( 14.1 )]. 1.3 Usage To reduce the development of drug-resistant bacteria and maintain the effectiveness of azithromycin tablets and other antibacterial drugs, azithromycin tablets should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
Spl product data elements
Usually a list of ingredients in a drug product.azithromycin dihydrate azithromycin dihydrate AZITHROMYCIN DIHYDRATE AZITHROMYCIN ANHYDROUS CALCIUM PHOSPHATE, DIBASIC, ANHYDROUS CROSCARMELLOSE SODIUM HYPROMELLOSE 2910 (15 MPA.S) LACTOSE MONOHYDRATE MAGNESIUM STEARATE SODIUM LAURYL SULFATE TITANIUM DIOXIDE TRIACETIN LU;L06
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Long-term studies in animals have not been performed to evaluate carcinogenic potential. Azithromycin has shown no mutagenic potential in standard laboratory tests: mouse lymphoma assay, human lymphocyte clastogenic assay, and mouse bone marrow clastogenic assay. In fertility studies conducted in male and female rats, oral administration of azithromycin for 64 to 66 days (males) or 15 days (females) prior to and during cohabitation resulted in decreased pregnancy rate at 20 and 30 mg/kg/day when both males and females were treated with azithromycin. This minimal effect on pregnancy rate (approximately 12% reduction compared to concurrent controls) did not become more pronounced when the dose was increased from 20 to 30 mg/kg/day (approximately 0.3 to 0.5 times the adult human daily dose of 600 mg based on body surface area) and it was not observed when only one animal in the mated pair was treated. There were no effects on any other reproductive parameters, and there were no effects on fertility at 10 mg/kg/day. The relevance of these findings to patients being treated with azithromycin at the doses and durations recommended in the prescribing information is uncertain. 13.2 Animal Toxicology Phospholipidosis (intracellular phospholipid accumulation) has been observed in some tissues of mice, rats, and dogs given multiple doses of azithromycin. It has been demonstrated in numerous organ systems (e.g., eye, dorsal root ganglia, liver, gallbladder, kidney, spleen, and/or pancreas) in dogs and rats treated with azithromycin at doses which, expressed on the basis of body surface area, are similar to or less than the highest recommended adult human dose. This effect has been shown to be reversible after cessation of azithromycin treatment. Based on the pharmacokinetic data, phospholipidosis has been seen in the rat (50 mg/kg/day dose) at the observed maximal plasma concentration of 1.3 mcg/mL (1.6 times the observed C max of 0.821 mcg/mL at the adult dose of 2 g.) Similarly, it has been shown in the dog (10 mg/kg/day dose) at the observed maximal serum concentration of 1 mcg/mL (1.2 times the observed C max of 0.821 mcg/mL at the adult dose of 2 g). Phospholipidosis was also observed in neonatal rats dosed for 18 days at 30 mg/kg/day, which is less than the pediatric dose of 60 mg/kg based on the surface area. It was not observed in neonatal rats treated for 10 days at 40 mg/kg/day with mean maximal serum concentrations of 1.86 mcg/mL, approximately 1.5 times the C max of 1.27 mcg/mL at the pediatric dose. Phospholipidosis has been observed in neonatal dogs (10 mg/kg/day) at maximum mean whole blood concentrations of 3.54 mcg/mL, approximately 3 times the pediatric dose C max . The significance of the finding for animals and for humans is unknown.
Microbiology
Microbiology12.4 Microbiology Mechanism of Action Azithromycin acts by binding to the 23S rRNA of the 50S ribosomal subunit of susceptible microorganisms inhibiting bacterial protein synthesis and impeding the assembly of the 50S ribosomal subunit. Resistance The most frequently encountered mechanism of resistance to azithromycin is modification of the 23S rRNA target, most often by methylation. Ribosomal modifications can determine cross resistance to other macrolides, lincosamides, and streptogramin B (MLS B phenotype). The mechanism of acquired mutational resistance in isolates of Mycobacterium avium complex (i.e., 23S rRNA genemutation) is the same for both clarithromycin and azithromycin. Antimicrobial Activity Azithromycin has been shown to be active against the following microorganisms, both in vitro and in clinical infections. [see INDICATIONS AND USAGE ( 1 )] Mycobacteria Mycobacterium avium complex (MAC) consisting of: Mycobacterium avium Mycobacterium intracellulare Other Microorganisms Chlamydia trachomatis Susceptibility Testing For specific information regarding susceptibility test interpretive criteria and associated test methods and quality control standards recognized by FDA for this drug, please see: https://www.fda.gov/STIC.
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PACKAGE LABEL.PRINCIPAL DISPLAY PANEL Azithromycin Tablets USP, 600 mg 30 Tablets- Container Label NDC 68180-863-06 Bottle Label - 600 mg
Recent major changes
A list of the section(s) that contain substantive changes that have been approved by FDA in the product labeling. The headings and subheadings, if appropriate, affected by the change are listed together with each section’s identifying number and the month and year on which the change was incorporated in the labeling.RECENT MAJOR CHANGES Warnings and Precautions, Cardiovascular Death ( 5.5 ) 11/2021
azithromycin dihydrate: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Azithromycin tablets may be taken with or without food. However, increased tolerability has been observed when tablets are taken with food. Patients should also be cautioned not to take aluminum- and magnesium-containing antacids and azithromycin simultaneously. The patient should be directed to discontinue azithromycin immediately and contact a physician if any signs of an allergic reaction occur. Direct parents or caregivers to contact their physician if vomiting and irritability with feeding occurs in the infant. Patients should be counseled that antibacterial drugs, including azithromycin, should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When azithromycin is prescribed to treat bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by azithromycin or other antibacterial drugs in the future. Diarrhea is a common problem caused by antibacterial which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibacterials, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial. If this occurs, patients should contact their physician as soon as possible. Manufactured for: Lupin Pharmaceuticals, Inc. Baltimore, Maryland 21202 United States Manufactured by: Lupin Limited Goa - 403722 India Revised: August 2022 ID#: 271316
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES 14.1 Clinical Studies in Patients with Advanced HIV Infection for the Prevention and Treatment of Disease Due to Disseminated Mycobacterium avium Complex (MAC) [see INDICATIONS AND USAGE ( 1 )] Prevention of Disseminated MAC Disease Two randomized, double - blind clinical trials were performed in patients with CD4 counts <100 cells/µL. The first trial (Study 155) compared azithromycin (1200 mg once weekly) to placebo and enrolled 182 patients with a mean CD4 count of 35 cells/mcgL. The second trial (Study 174) randomized 723 patients to either azithromycin (1200 mg once weekly), rifabutin (300 mg daily), or the combination of both. The mean CD4 count was 51 cells/mcgL. The primary endpoint in these trials was disseminated MAC disease. Other endpoints included the incidence of clinically significant MAC disease and discontinuations from therapy for drug-related side effects. MAC bacteremia In Study 155, 85 patients randomized to receive azithromycin and 89 patients randomized to receive placebo met the entrance criteria. Cumulative incidences at 6, 12, and 18 months of the possible outcomes are in the following table: Cumulative Incidence Rate , %: Placebo ( n = 89 ) Month MAC Free and Alive MAC Adverse Experience Lost to Follow - up 6 69.7 13.5 6.7 10.1 12 47.2 19.1 15.7 18.0 18 37.1 22.5 18.0 22.5 Cumulative Incidence Rate , %: Azithromycin ( n = 85 ) Month MAC Free and Alive MAC Adverse Experience Lost to Follow - up 6 84.7 3.5 9.4 2.4 12 63.5 8.2 16.5 11.8 18 44.7 11.8 25.9 17.6 The difference in the one-year cumulative incidence rates of disseminated MAC disease (placebo-azithromycin) is 10.9%. This difference is statistically significant (p=0.037) with a 95% confidence interval for this difference of 0.8%, 20.9%. The comparable number of patients experiencing adverse events and the fewer number of patients lost to follow-up on azithromycin should be taken into account when interpreting the significance of this difference. In Study 174, 223 patients randomized to receive rifabutin, 223 patients randomized to receive azithromycin, and 218 patients randomized to receive both rifabutin and azithromycin met the entrance criteria. Cumulative incidences at 6, 12, and 18 months of the possible outcomes are recorded in the following table: Cumulative Incidence Rate , %: Rifabutin ( n = 223 ) Month MAC Free and Alive MAC Adverse Experience Lost to Follow - up 6 83.4 7.2 8.1 1.3 12 60.1 15.2 16.1 8.5 18 40.8 21.5 24.2 13.5 Cumulative Incidence Rate , %: Azithromycin ( n = 223 ) Month MAC Free and Alive MAC Adverse Experience Lost to Follow - up 6 85.2 3.6 5.8 5.4 12 65.5 7.6 16.1 10.8 18 45.3 12.1 23.8 18.8 Cumulative Incidence Rate , %: Azithromycin / Rifabutin Combination ( n = 218 ) Month MAC Free and Alive MAC Adverse Experience Lost to Follow - up 6 89.4 1.8 5.5 3.2 12 71.6 2.8 15.1 10.6 18 49.1 6.4 29.4 15.1 Comparing the cumulative one - year incidence rates, azithromycin monotherapy is at least as effective as rifabutin monotherapy. The difference (rifabutin – azithromycin) in the one - year rates (7.6%) is statistically significant (p=0.022) with an adjusted 95% confidence interval (0.9%, 14.3%). Additionally, azithromycin/rifabutin combination therapy is more effective than rifabutin alone. The difference (rifabutin – azithromycin/rifabutin) in the cumulative one - year incidence rates (12.5%) is statistically significant (p<0.001) with an adjusted 95% confidence interval of 6.6%, 18.4%. The comparable number of patients experiencing adverse events and the fewer number of patients lost to follow-up on rifabutin should be taken into account when interpreting the significance of this difference. In Study 174, sensitivity testing 2 was performed on all available MAC isolates from subjects randomized to either azithromycin, rifabutin, or the combination. The distribution of MIC values for azithromycin from susceptibility testing of the breakthrough isolates was similar between trial arms. As the efficacy of azithromycin in the treatment of disseminated MAC has not been established, the clinical relevance of these in vitro MICs as an indicator of susceptibility or resistance is not known. Clinically Significant Disseminated MAC Disease In association with the decreased incidence of bacteremia, patients in the groups randomized to either azithromycin alone or azithromycin in combination with rifabutin showed reductions in the signs and symptoms of disseminated MAC disease, including fever or night sweats, weight loss, and anemia. Discontinuations from Therapy for Drug-Related Side Effects In Study 155, discontinuations for drug-related toxicity occurred in 8.2% of subjects treated with azithromycin and 2.3% of those given placebo (p=0.121). In Study 174, more subjects discontinued from the combination of azithromycin and rifabutin (22.7%) than from azithromycin alone (13.5%; p=0.026) or rifabutin alone (15.9%; p=0.209). Safety As these patients with advanced HIV disease were taking multiple concomitant medications and experienced a variety of intercurrent illnesses, it was often difficult to attribute adverse reactions to study medication. Overall, the nature of adverse reactions seen on the weekly dosage regimen of azithromycin over a period of approximately one year in patients with advanced HIV disease were similar to that previously reported for shorter course therapies. INCIDENCE OF ONE OR MORE TREATMENT-RELATED a ADVERSE REACTIONS b IN HIV INFECTED PATIENTS RECEIVING PROPHYLAXIS FOR DISSEMINATED MAC OVER APPROXIMATELY 1 YEAR a Includes those reactions considered possibly or probably related to study drug b >2% adverse reaction rates for any group (except uveitis) Study 155 Study 174 Placebo ( N = 91 ) Azithromycin 1200 mg weekly ( N = 89 ) Azithromycin 1200 mg weekly ( N = 233 ) Rifabutin 300 mg daily ( N = 236 ) Azithromycin + Rifabutin ( N = 224 ) Mean Duration of Therapy (days) 303.8 402.9 315 296.1 344.4 Discontinuation of Therapy 2.3 8.2 13.5 15.9 22.7 Autonomic Nervous System Mouth Dry 0 0 0 3 2.7 Central Nervous System Dizziness 0 1.1 3.9 1.7 0.4 Headache 0 0 3 5.5 4.5 Gastrointestinal Diarrhea 15.4 52.8 50.2 19.1 50.9 Loose Stools 6.6 19.1 12.9 3 9.4 Abdominal Pain 6.6 27 32.2 12.3 31.7 Dyspepsia 1.1 9 4.7 1.7 1.8 Flatulence 4.4 9 10.7 5.1 5.8 Nausea 11 32.6 27 16.5 28.1 Vomiting 1.1 6.7 9 3.8 5.8 General Fever 1.1 0 2.1 4.2 4.9 Fatigue 0 2.2 3.9 2.1 3.1 Malaise 0 1.1 0.4 0 2.2 Musculoskeletal Arthralgia 0 0 3 4.2 7.1 Psychiatric Anorexia 1.1 0 2.1 2.1 3.1 Skin & Appendages Pruritus 3.3 0 3.9 3.4 7.6 Rash 3.2 3.4 8.1 9.4 11.1 Skin discoloration 0 0 0 2.1 2.2 Special Senses Tinnitus 4.4 3.4 0.9 1.3 0.9 Hearing Decreased 2.2 1.1 0.9 0.4 0 Uveitis 0 0 0.4 1.3 1.8 Taste Perversion 0 0 1.3 2.5 1.3 Adverse reactions related to the gastrointestinal tract were seen more frequently in patients receiving azithromycin than in those receiving placebo or rifabutin. In Study 174, 86% of diarrheal episodes were mild to moderate in nature with discontinuation of therapy for this reason occurring in only 9/233 (3.8%) of patients. Changes in Laboratory Values In these immunocompromised patients with advanced HIV infection, it was necessary to assess laboratory abnormalities developing on trial with additional criteria if baseline values were outside the relevant normal range. PROPHYLAXIS AGAINST DISSEMINATED MAC ABNORMAL LABORATORY VALUES a a excludes subjects outside of the relevant normal range at baseline Placebo Azithromycin 1200 mg weekly Rifabutin 300 mg daily Azithromycin & Rifabutin Hemoglobin <8 g/dL 1/51 2% 4/170 2% 4/114 4% 8/107 8% Platelet Count <50 × 10 3 /mm 3 1/71 1% 4/260 2% 2/182 1% 6/181 3% WBC Count <1 × 10 3 /mm 3 0/8 0% 2/70 3% 2/47 4% 0/43 0% Neutrophils <500/mm 3 0/26 0% 4/106 4% 3/82 4% 2/78 3% SGOT >5 × ULN Upper Limit of Normal 1/41 2% 8/158 5% 3/121 3% 6/114 5% SGPT >5 × ULN 0/49 0% 8/166 5% 3/130 2% 5/117 4% Alk Phos >5 × ULN 1/80 1% 4/247 2% 2/172 1% 3/164 2% Treatment of Disseminated MAC Disease One randomized, double - blind clinical trial (Study 189) was performed in patients with disseminated MAC. In this trial, 246 HIV - infected patients with disseminated MAC received either azithromycin 250 mg daily (N=65), azithromycin 600 mg daily (N=91), or clarithromycin 500 mg twice a day (N=90), each administered with ethambutol 15 mg/kg daily, for 24 weeks. Blood cultures and clinical assessments were performed every 3 weeks through week 12 and monthly thereafter through week 24. After week 24, patients were switched to any open - label therapy at the discretion of the investigator and followed every 3 months through the last follow - up visit of the trial. Patients were followed from the baseline visit for a period of up to 3.7 years (median: 9 months). MAC isolates recovered during treatment or post-treatment were obtained whenever possible. The primary endpoint was sterilization by week 24. Sterilization was based on data from the central laboratory, and was defined as two consecutive observed negative blood cultures for MAC, independent of missing culture data between the two negative observations. Analyses were performed on all randomized patients who had a positive baseline culture for MAC. The azithromycin 250 mg arm was discontinued after an interim analysis at 12 weeks showed a significantly lower clearance of bacteremia compared to clarithromycin 500 mg twice a day. Efficacy results for the azithromycin 600 mg daily and clarithromycin 500 mg twice a day treatment regimens are described in the following table: RESPONSE TO THERAPY OF PATIENTS TAKING ETHAMBUTOL AND EITHER AZITHROMYCIN 600 MG DAILY OR CLARITHROMYCIN 500 MG TWICE A DAY Azithromycin 600 mg daily Clarithromycin 500 mg twice a day [95% confidence interval] on difference in rates (azithromycin-clarithromycin) 95 . 1 % CI on difference Patients with positive culture at baseline 68 57 Week 24 Two consecutive negative blood cultures Primary endpoint 31/68 (46%) 32/57 (56%) [-28, 7] Mortality 16/68 (24%) 15/57 (26%) [-18, 13] The primary endpoint, rate of sterilization of blood cultures (two consecutive negative cultures) at 24 weeks, was lower in the azithromycin 600 mg daily group than in the clarithromycin 500 mg twice a day group. Sterilization by Baseline Colony Count Within both treatment groups, the sterilization rates at week 24 decreased as the range of MAC cfu/mL increased. Azithromycin 600 mg ( N = 68 ) Clarithromycin 500 mg twice a day ( N = 57 ) groups stratified by MAC colony counts at baseline no . (%) subjects in stratified group sterile at week 24 no . (%) subjects in stratified group sterile at week 24 ≤10 cfu/mL 10/15 (66.7%) 12/17 (70.6%) 11 to 100 cfu/mL 13/28 (46.4%) 13/19 (68.4%) 101 to 1,000 cfu/mL 7/19 (36.8%) 5/13 (38.5%) 1,001 to 10,000 cfu/mL 1/5 (20.0%) 1/5 (20%) >10,000 cfu/mL 0/1 (0.0%) 1/3 (33.3%) Susceptibility Pattern of MAC Isolates Susceptibility testing was performed on MAC isolates recovered at baseline, at the time of breakthrough on therapy or during post-therapy follow-up. The T100 radiometric broth method was employed to determine azithromycin and clarithromycin MIC values. Azithromycin MIC values ranged from <4 to >256 mcg/mL and clarithromycin MICs ranged from <1 to >32 mcg/mL. The individual MAC susceptibility results demonstrated that azithromycin MIC values could be 4 to 32-fold higher than clarithromycin MIC values. During treatment and post-treatment follow-up for up to 3.7 years (median: 9 months) in Study 189, a total of 6/68 (9%) and 6/57 (11%) of the patients randomized to azithromycin 600 mg daily and clarithromycin 500 mg twice a day respectively, developed MAC blood culture isolates that had a sharp increase in MIC values. All twelve MAC isolates had azithromycin MICs ≥256 mcg/mL and clarithromycin MICs >32 mcg/mL. These high MIC values suggest development of drug resistance. However, at this time, specific breakpoints for separating susceptible and resistant MAC isolates have not been established for either macrolide.
| 6 | 69.7 | 13.5 | 6.7 | 10.1 |
| 12 | 47.2 | 19.1 | 15.7 | 18.0 |
| 18 | 37.1 | 22.5 | 18.0 | 22.5 |
| 6 | 84.7 | 3.5 | 9.4 | 2.4 |
| 12 | 63.5 | 8.2 | 16.5 | 11.8 |
| 18 | 44.7 | 11.8 | 25.9 | 17.6 |
| 6 | 83.4 | 7.2 | 8.1 | 1.3 |
| 12 | 60.1 | 15.2 | 16.1 | 8.5 |
| 18 | 40.8 | 21.5 | 24.2 | 13.5 |
| 6 | 85.2 | 3.6 | 5.8 | 5.4 |
| 12 | 65.5 | 7.6 | 16.1 | 10.8 |
| 18 | 45.3 | 12.1 | 23.8 | 18.8 |
| 6 | 89.4 | 1.8 | 5.5 | 3.2 |
| 12 | 71.6 | 2.8 | 15.1 | 10.6 |
| 18 | 49.1 | 6.4 | 29.4 | 15.1 |
| Mean Duration of Therapy (days) | 303.8 | 402.9 | 315 | 296.1 | 344.4 |
| Discontinuation of Therapy | 2.3 | 8.2 | 13.5 | 15.9 | 22.7 |
| Mouth Dry | 0 | 0 | 0 | 3 | 2.7 |
| Dizziness | 0 | 1.1 | 3.9 | 1.7 | 0.4 |
| Headache | 0 | 0 | 3 | 5.5 | 4.5 |
| Diarrhea | 15.4 | 52.8 | 50.2 | 19.1 | 50.9 |
| Loose Stools | 6.6 | 19.1 | 12.9 | 3 | 9.4 |
| Abdominal Pain | 6.6 | 27 | 32.2 | 12.3 | 31.7 |
| Dyspepsia | 1.1 | 9 | 4.7 | 1.7 | 1.8 |
| Flatulence | 4.4 | 9 | 10.7 | 5.1 | 5.8 |
| Nausea | 11 | 32.6 | 27 | 16.5 | 28.1 |
| Vomiting | 1.1 | 6.7 | 9 | 3.8 | 5.8 |
| Fever | 1.1 | 0 | 2.1 | 4.2 | 4.9 |
| Fatigue | 0 | 2.2 | 3.9 | 2.1 | 3.1 |
| Malaise | 0 | 1.1 | 0.4 | 0 | 2.2 |
| Arthralgia | 0 | 0 | 3 | 4.2 | 7.1 |
| Anorexia | 1.1 | 0 | 2.1 | 2.1 | 3.1 |
| Pruritus | 3.3 | 0 | 3.9 | 3.4 | 7.6 |
| Rash | 3.2 | 3.4 | 8.1 | 9.4 | 11.1 |
| Skin discoloration | 0 | 0 | 0 | 2.1 | 2.2 |
| Tinnitus | 4.4 | 3.4 | 0.9 | 1.3 | 0.9 |
| Hearing Decreased | 2.2 | 1.1 | 0.9 | 0.4 | 0 |
| Uveitis | 0 | 0 | 0.4 | 1.3 | 1.8 |
| Taste Perversion | 0 | 0 | 1.3 | 2.5 | 1.3 |
| Hemoglobin | <8 g/dL | 1/51 | 2% | 4/170 | 2% | 4/114 | 4% | 8/107 | 8% |
| Platelet Count | <50 × 103/mm3 | 1/71 | 1% | 4/260 | 2% | 2/182 | 1% | 6/181 | 3% |
| WBC Count | <1 × 103/mm3 | 0/8 | 0% | 2/70 | 3% | 2/47 | 4% | 0/43 | 0% |
| Neutrophils | <500/mm3 | 0/26 | 0% | 4/106 | 4% | 3/82 | 4% | 2/78 | 3% |
| SGOT | >5 × ULN | 1/41 | 2% | 8/158 | 5% | 3/121 | 3% | 6/114 | 5% |
| SGPT | >5 × ULN | 0/49 | 0% | 8/166 | 5% | 3/130 | 2% | 5/117 | 4% |
| Alk Phos | >5 × ULN | 1/80 | 1% | 4/247 | 2% | 2/172 | 1% | 3/164 | 2% |
| Patients with positive culture at baseline | 68 | 57 | |
| Week 24 | |||
| Two consecutive negative blood cultures | 31/68 (46%) | 32/57 (56%) | [-28, 7] |
| Mortality | 16/68 (24%) | 15/57 (26%) | [-18, 13] |
| ≤10 cfu/mL | 10/15 (66.7%) | 12/17 (70.6%) |
| 11 to 100 cfu/mL | 13/28 (46.4%) | 13/19 (68.4%) |
| 101 to 1,000 cfu/mL | 7/19 (36.8%) | 5/13 (38.5%) |
| 1,001 to 10,000 cfu/mL | 1/5 (20.0%) | 1/5 (20%) |
| >10,000 cfu/mL | 0/1 (0.0%) | 1/3 (33.3%) |
References
This field may contain references when prescription drug labeling must summarize or otherwise relay on a recommendation by an authoritative scientific body, or on a standardized methodology, scale, or technique, because the information is important to prescribing decisions.15 REFERENCES Susceptibility Testing of Mycobacteria, Nocardia, and Other Aerobic Actinomycetes; Approved Standard, CLSI document M24 A2, CLSI, 2011. Griffith DE, Aksamit T, Brown-Elliot BA, et al. An official ATS/IDSA statement: Diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367-416.
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use In multiple-dose clinical trials of oral azithromycin, 9% of patients were at least 65 years of age (458/4949) and 3% of patients (144/4949) were at least 75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Elderly patients may be more susceptible to development of torsades de pointes arrhythmias than younger patients. [see WARNINGS AND PRECAUTIONS ( 5.4 )] Azithromycin 600 mg tablets contain 1.5 mg of sodium per tablet. Geriatric Patients with Opportunistic Infections, Including (MAC) Disease Safety data are available for 30 patients (65 to 94 years old) treated with azithromycin at doses >300 mg/day for a mean of 207 days. These patients were treated for a variety of opportunistic infections, including MAC. The adverse reaction were generally similar to that seen in younger patients, except for a higher incidence of adverse reactions relating to the gastrointestinal system and to reversible impairment of hearing. [see DOSAGE AND ADMINISTRATION ( 2 )]
Nursing mothers
Information about excretion of the drug in human milk and effects on the nursing infant, including pertinent adverse effects observed in animal offspring.8.2 Lactation Risk Summary Azithromycin is present in human milk (see Data) . Non-serious adverse reactions have been reported in breastfed infants after maternal administration of azithromycin (see Clinical Considerations) . There are no available data on the effects of azithromycin on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for azithromycin and any potential adverse effects on the breastfed infant from azithromycin or from the underlying maternal condition. Clinical Considerations Advise women to monitor the breastfed infant for diarrhea, vomiting, or rash. Data Azithromycin breastmilk concentrations were measured in 20 women after receiving a single 2 g oral dose of azithromycin during labor. Breastmilk samples collected on days 3 and 6 postpartum as well as 2 and 4 weeks postpartum revealed the presence of azithromycin in breastmilk up to 4 weeks after dosing. In another study, a single dose of azithromycin 500 mg was administered intravenously to 8 women prior to incision for cesarean section. Breastmilk (colostrum) samples obtained between 12 and 48 hours after dosing revealed that azithromycin persisted in breastmilk up to 48 hours.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use In controlled clinical studies, azithromycin has been administered to pediatric patients ranging in age from 6 months to 12 years. For information regarding the use of azithromycin for oral suspension in the treatment of pediatric patients, [see INDICATIONS AND USAGE ( 1 ) and DOSAGE AND ADMINISTRATION ( 2 )] of the prescribing information for azithromycin for oral suspension 100 mg/5 mL and 200 mg/5 mL bottles. HIV-Infected Pediatric Patients The safety and efficacy of azithromycin for the prevention or treatment of MAC in HIV-infected children have not been established. Safety data are available for 72 children 5 months to 18 years of age (mean 7 years) who received azithromycin for treatment of opportunistic infections. The mean duration of therapy was 242 days (range 3 to 2004 days) at doses of <1 to 52 mg/kg/day (mean 12 mg/kg/day). Adverse reactions were similar to those observed in the adult population, most of which involved the gastrointestinal tract. Treatment - related reversible hearing impairment in children was observed in 4 subjects (5.6%). Two (2.8%) children prematurely discontinued treatment due to adverse reactions: one due to back pain and one due to abdominal pain, hot and cold flushes, dizziness, headache, and numbness. A third child discontinued due to a laboratory abnormality (eosinophilia). The protocols upon which these data are based specified a daily dose of 10 to 20 mg/kg/day (oral and/or IV) of azithromycin.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Risk Summary Available data from published literature and postmarketing experience over several decades with azithromycin use in pregnant women have not identified any drug-associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data) . Developmental toxicity studies with azithromycin in rats, mice, and rabbits showed no drug-induced fetal malformations at doses up to 3, 2, and 1 times, respectively, an adult human daily dose of 600 mg based on body surface area. Decreased viability and delayed development were observed in the offspring of pregnant rats administered azithromycin from day 6 of pregnancy through weaning at a dose equivalent to 3 times an adult human daily dose of 600 mg based on body surface area (see Data). The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. Data Human Data: Available data from published observational studies, case series, and case reports over several decades do not suggest an increased risk for major birth defects, miscarriage, or adverse maternal or fetal outcomes with azithromycin use in pregnant women. Limitations of these data include the lack of randomization and inability to control for confounders such as underlying maternal disease and maternal use of concomitant medications. Animal Data: Azithromycin administered during the period of organogenesis did not cause fetal malformations in rats and mice at oral doses up to 200 mg/kg/day (moderately maternally toxic). Based on body surface area, this dose is approximately 3 (rats) and 2 (mice) times an adult human daily dose of 600 mg. In rabbits administered azithromycin at oral doses of 10, 20, and 40 mg/kg/day during organogenesis, reduced maternal body weight and food consumption were observed in all groups; no evidence of fetotoxicity or teratogenicity was observed at these doses, the highest of which is approximately equal to an adult human daily dose of 600 mg based on body surface area. In a pre-and postnatal development study, azithromycin was administered orally to pregnant rats from day 6 of pregnancy until weaning at doses of 50 or 200 mg/kg/day. Maternal toxicity (reduced food consumption and body weight gain; increased stress at parturition) was observed at the higher dose. Effects in the offspring were noted at 200 mg/kg/day during the postnatal development period (decreased viability, delayed developmental landmarks). These effects were not observed in a pre-and postnatal rat study when up to 200 mg/kg/day of azithromycin was given orally beginning on day 15 of pregnancy until weaning.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS Pediatric Use: Safety and effectiveness in the treatment of patients under 6 months of age have not been established. ( 8.4 ) Geriatric Use: Elderly patients may be more susceptible to development of torsades de pointes arrhythmias. ( 8.5 ) 8.1 Pregnancy Risk Summary Available data from published literature and postmarketing experience over several decades with azithromycin use in pregnant women have not identified any drug-associated risks for major birth defects, miscarriage, or adverse maternal or fetal outcomes (see Data) . Developmental toxicity studies with azithromycin in rats, mice, and rabbits showed no drug-induced fetal malformations at doses up to 3, 2, and 1 times, respectively, an adult human daily dose of 600 mg based on body surface area. Decreased viability and delayed development were observed in the offspring of pregnant rats administered azithromycin from day 6 of pregnancy through weaning at a dose equivalent to 3 times an adult human daily dose of 600 mg based on body surface area (see Data). The estimated background risk of major birth defects and miscarriage for the indicated populations is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively. Data Human Data: Available data from published observational studies, case series, and case reports over several decades do not suggest an increased risk for major birth defects, miscarriage, or adverse maternal or fetal outcomes with azithromycin use in pregnant women. Limitations of these data include the lack of randomization and inability to control for confounders such as underlying maternal disease and maternal use of concomitant medications. Animal Data: Azithromycin administered during the period of organogenesis did not cause fetal malformations in rats and mice at oral doses up to 200 mg/kg/day (moderately maternally toxic). Based on body surface area, this dose is approximately 3 (rats) and 2 (mice) times an adult human daily dose of 600 mg. In rabbits administered azithromycin at oral doses of 10, 20, and 40 mg/kg/day during organogenesis, reduced maternal body weight and food consumption were observed in all groups; no evidence of fetotoxicity or teratogenicity was observed at these doses, the highest of which is approximately equal to an adult human daily dose of 600 mg based on body surface area. In a pre-and postnatal development study, azithromycin was administered orally to pregnant rats from day 6 of pregnancy until weaning at doses of 50 or 200 mg/kg/day. Maternal toxicity (reduced food consumption and body weight gain; increased stress at parturition) was observed at the higher dose. Effects in the offspring were noted at 200 mg/kg/day during the postnatal development period (decreased viability, delayed developmental landmarks). These effects were not observed in a pre-and postnatal rat study when up to 200 mg/kg/day of azithromycin was given orally beginning on day 15 of pregnancy until weaning. 8.2 Lactation Risk Summary Azithromycin is present in human milk (see Data) . Non-serious adverse reactions have been reported in breastfed infants after maternal administration of azithromycin (see Clinical Considerations) . There are no available data on the effects of azithromycin on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for azithromycin and any potential adverse effects on the breastfed infant from azithromycin or from the underlying maternal condition. Clinical Considerations Advise women to monitor the breastfed infant for diarrhea, vomiting, or rash. Data Azithromycin breastmilk concentrations were measured in 20 women after receiving a single 2 g oral dose of azithromycin during labor. Breastmilk samples collected on days 3 and 6 postpartum as well as 2 and 4 weeks postpartum revealed the presence of azithromycin in breastmilk up to 4 weeks after dosing. In another study, a single dose of azithromycin 500 mg was administered intravenously to 8 women prior to incision for cesarean section. Breastmilk (colostrum) samples obtained between 12 and 48 hours after dosing revealed that azithromycin persisted in breastmilk up to 48 hours. 8.4 Pediatric Use In controlled clinical studies, azithromycin has been administered to pediatric patients ranging in age from 6 months to 12 years. For information regarding the use of azithromycin for oral suspension in the treatment of pediatric patients, [see INDICATIONS AND USAGE ( 1 ) and DOSAGE AND ADMINISTRATION ( 2 )] of the prescribing information for azithromycin for oral suspension 100 mg/5 mL and 200 mg/5 mL bottles. HIV-Infected Pediatric Patients The safety and efficacy of azithromycin for the prevention or treatment of MAC in HIV-infected children have not been established. Safety data are available for 72 children 5 months to 18 years of age (mean 7 years) who received azithromycin for treatment of opportunistic infections. The mean duration of therapy was 242 days (range 3 to 2004 days) at doses of <1 to 52 mg/kg/day (mean 12 mg/kg/day). Adverse reactions were similar to those observed in the adult population, most of which involved the gastrointestinal tract. Treatment - related reversible hearing impairment in children was observed in 4 subjects (5.6%). Two (2.8%) children prematurely discontinued treatment due to adverse reactions: one due to back pain and one due to abdominal pain, hot and cold flushes, dizziness, headache, and numbness. A third child discontinued due to a laboratory abnormality (eosinophilia). The protocols upon which these data are based specified a daily dose of 10 to 20 mg/kg/day (oral and/or IV) of azithromycin. 8.5 Geriatric Use In multiple-dose clinical trials of oral azithromycin, 9% of patients were at least 65 years of age (458/4949) and 3% of patients (144/4949) were at least 75 years of age. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Elderly patients may be more susceptible to development of torsades de pointes arrhythmias than younger patients. [see WARNINGS AND PRECAUTIONS ( 5.4 )] Azithromycin 600 mg tablets contain 1.5 mg of sodium per tablet. Geriatric Patients with Opportunistic Infections, Including (MAC) Disease Safety data are available for 30 patients (65 to 94 years old) treated with azithromycin at doses >300 mg/day for a mean of 207 days. These patients were treated for a variety of opportunistic infections, including MAC. The adverse reaction were generally similar to that seen in younger patients, except for a higher incidence of adverse reactions relating to the gastrointestinal system and to reversible impairment of hearing. [see DOSAGE AND ADMINISTRATION ( 2 )]
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING Azithromycin Tablets USP, 600 mg are supplied as white, oval shaped film-coated tablets, engraved with "LU" on one side and "L06" on the other side containing azithromycin dihydrate equivalent to 600 mg of azithromycin USP. These are packaged in bottles of 30 tablets as follows: Bottles of 30 Tablets: NDC 68180-863-06 Tablets should be stored at 25°C (77°F); excursions permitted to 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API