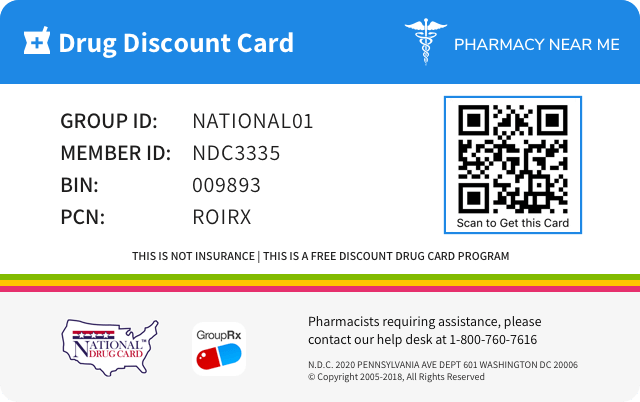
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 70518-3741 | ||||
|---|---|---|---|---|---|
| Drug Name | Risperidone |
||||
| Type | Generic | ||||
| Pharm Class | Atypical Antipsychotic [EPC] | ||||
| Active Ingredients |
|
||||
| Route | ORAL | ||||
| Dosage Form | SOLUTION | ||||
| RxCUI drug identifier | 199387 | ||||
| Application Number | ANDA079059 | ||||
| Labeler Name | REMEDYREPACK INC. | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Abuse
Information about the types of abuse that can occur with the drug and adverse reactions pertinent to those types of abuse, primarily based on human data. May include descriptions of particularly susceptible patient populations.9.2 Abuse Risperidone has not been systematically studied in animals or humans for its potential for abuse. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of risperidone misuse or abuse (e.g., development of tolerance, increases in dose, drug-seeking behavior).
Controlled substance
Information about the schedule in which the drug is controlled by the Drug Enforcement Administration, if applicable.9.1 Controlled Substance Risperidone oral solution is not a controlled substance.
Dependence
Information about characteristic effects resulting from both psychological and physical dependence that occur with the drug, the quantity of drug over a period of time that may lead to tolerance or dependence, details of adverse effects related to chronic abuse and the effects of abrupt withdrawl, procedures necessary to diagnose the dependent state, and principles of treating the effects of abrupt withdrawal.9.3 Dependence Risperidone has not been systematically studied in animals or humans for its potential for tolerance or physical dependence.
Drug abuse and dependence
Information about whether the drug is a controlled substance, the types of abuse that can occur with the drug, and adverse reactions pertinent to those types of abuse.9 DRUG ABUSE AND DEPENDENCE 9.1 Controlled Substance Risperidone oral solution is not a controlled substance. 9.2 Abuse Risperidone has not been systematically studied in animals or humans for its potential for abuse. While the clinical trials did not reveal any tendency for any drug-seeking behavior, these observations were not systematic and it is not possible to predict on the basis of this limited experience the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed. Consequently, patients should be evaluated carefully for a history of drug abuse, and such patients should be observed closely for signs of risperidone misuse or abuse (e.g., development of tolerance, increases in dose, drug-seeking behavior). 9.3 Dependence Risperidone has not been systematically studied in animals or humans for its potential for tolerance or physical dependence.
Overdosage of Risperidone
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE 10.1 Human Experience Premarketing experience included eight reports of acute risperidone overdosage with estimated doses ranging from 20 to 300 mg and no fatalities. In general, reported signs and symptoms were those resulting from an exaggeration of the drug's known pharmacological effects, i.e., drowsiness and sedation, tachycardia and hypotension, and extrapyramidal symptoms. One case, involving an estimated overdose of 240 mg, was associated with hyponatremia, hypokalemia, prolonged QT, and widened QRS. Another case, involving an estimated overdose of 36 mg, was associated with a seizure. Postmarketing experience includes reports of acute risperidone overdosage, with estimated doses of up to 360 mg. In general, the most frequently reported signs and symptoms are those resulting from an exaggeration of the drug's known pharmacological effects, i.e., drowsiness, sedation, tachycardia, hypotension, and extrapyramidal symptoms. Other adverse reactions reported since market introduction related to risperidone overdose include prolonged QT interval and convulsions. Torsade de pointes has been reported in association with combined overdose of risperidone and paroxetine. 10.2 Management of Overdosage For the most up to date information on the management of risperidone overdosage, contact a certified poison control center (1-800-222-1222 or www.poison.org). Provide supportive care including close medical supervision and monitoring. Treatment should consist of general measures employed in the management of overdosage with any drug. Consider the possibility of multiple drug overdosage. Ensure an adequate airway, oxygenation, and ventilation. Monitor cardiac rhythm and vital signs. Use supportive and symptomatic measures. There is no specific antidote to risperidone.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS The following are discussed in more detail in other sections of the labeling:; Increased mortality in elderly patients with dementia-related psychosis [ see Boxed Warning and Warnings and Precautions; ( 5.1 ) ] Cerebrovascular adverse events, including stroke, in elderly patients with dementia-related psychosis [ see Warnings and Precautions; ( 5.2 ) ] Neuroleptic malignant syndrome [ see Warnings and Precautions; ( 5.3 ) ] Tardive dyskinesia [ see Warnings and Precautions; ( 5.4 ) ] Metabolic Changes (Hyperglycemia and diabetes mellitus, Dyslipidemia, and Weight Gain) [ see Warnings and Precautions; ( 5.5 ) ] Hyperprolactinemia [ see Warnings and Precautions; ( 5.6 ) ] Orthostatic hypotension [ see Warnings and Precautions; ( 5.7 ) ] Falls [ see Warnings and Precautions ; ( 5.9 ) ] Potential for cognitive and motor impairment [ see Warnings and Precautions-732c-4032-b401-1fea4ee2cff0">( 5.11 ) ] Dysphagia [ see Warnings and Precautions; ( 5.12 ) ] Priapism [ see Warnings and Precautions; ( 5.13 ) ] Disruption of body temperature regulation [ see Warnings and Precautions; ( 5.14 ) ]; The most common adverse reactions in clinical trials (>5% and twice placebo) were parkinsonism, akathisia, dystonia, tremor, sedation, dizziness, anxiety, blurred vision, nausea, vomiting, upper abdominal pain, stomach discomfort, dyspepsia, diarrhea, salivary hypersecretion, constipation, dry mouth, increased appetite, increased weight, fatigue, rash, nasal congestion, upper respiratory tract infection, nasopharyngitis, and pharyngolaryngeal pain. The most common adverse reactions that were associated with discontinuation from clinical trials (causing discontinuation in >1% of adults and/or >2% of pediatrics) were nausea, somnolence, sedation, vomiting, dizziness, and akathisia [ see Adverse Reactions , Discontinuations Due to Adverse Reactions ( 6.1 )]. The data described in this section are derived from a clinical trial database consisting of 9803 adult and pediatric patients exposed to one or more doses of risperidone for the treatment of schizophrenia, bipolar mania, autistic disorder, and other psychiatric disorders in pediatrics and elderly patients with dementia. Of these 9803 patients, 2687 were patients who received risperidone while participating in double-blind, placebo-controlled trials. The conditions and duration of treatment with risperidone varied greatly and included (in overlapping categories) double-blind, fixed- and flexible-dose, placebo- or active-controlled studies and open-label phases of studies, inpatients and outpatients, and short-term (up to 12 weeks) and longer-term (up to 3 years) exposures. Safety was assessed by collecting adverse events and performing physical examinations, vital signs, body weights, laboratory analyses, and ECGs. The most common adverse reactions in clinical trials (≥ 5% and twice placebo) were parkinsonism, akathisia, dystonia, tremor, sedation, dizziness, anxiety, blurred vision, nausea, vomiting, upper abdominal pain, stomach discomfort, dyspepsia, diarrhea, salivary hypersecretion, constipation, dry mouth, increased appetite, increased weight, fatigue, rash, nasal congestion, upper respiratory tract infection, nasopharyngitis, and pharyngolaryngeal pain. ( 6) To report SUSPECTED ADVERSE REACTIONS, contact Tris Pharma, Inc. (1-732-940-0358) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch
Risperidone Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS Carbamazepine and other enzyme inducers decrease plasma concentrations of risperidone. Increase the risperidone dose up to double the patient’s usual dose. Titrate slowly. ( 7.1) Fluoxetine, paroxetine, and other CYP 2D6 enzyme inhibitors increase plasma concentrations of risperidone. Reduce the initial dose. Do not exceed a final dose of 8 mg per day of risperidone. ( 7.1)
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action The mechanism of action of risperidone in schizophrenia is unclear. The drug's therapeutic activity in schizophrenia could be mediated through a combination of dopamine Type 2 (D 2 ) and serotonin Type 2 (5HT 2 ) receptor antagonism. The clinical effect from risperidone results from the combined concentrations of risperidone and its major metabolite, 9-hydroxyrisperidone (paliperidone) [ see Clinical Pharmacology (12.3) ]. Antagonism at receptors other than D 2 and 5HT 2 may explain some of the other effects of risperidone [ see Clinical Pharmacology (12.1) ]. 12.2 Pharmacodynamics Risperidone is a monoaminergic antagonist with high affinity (Ki of 0.12 to 7.3 nM) for the serotonin Type 2 (5HT 2 ), dopamine Type 2 (D 2 ), α 1 and α 2 adrenergic, and H 1 histaminergic receptors. Risperidone showed low to moderate affinity (Ki of 47 to 253 nM) for the serotonin 5HT 1C , 5HT 1D , and 5HT 1A receptors, weak affinity (Ki of 620 to 800 nM) for the dopamine D 1 and haloperidol-sensitive sigma site, and no affinity (when tested at concentrations >10 -5 M) for cholinergic muscarinic or β 1 and β 2 adrenergic receptors. 12.3 Pharmacokinetics Absorption Risperidone is well absorbed. The absolute oral bioavailability of risperidone is 70% (CV = 25%). The relative oral bioavailability of risperidone from a tablet is 94% (CV = 10%) when compared to a solution. Pharmacokinetic studies showed that Risperidone Orally Disintegrating Tablets and Risperidone Oral Solution are bioequivalent to Risperidone Tablets. Plasma concentrations of risperidone, its major metabolite, 9-hydroxyrisperidone, and risperidone plus 9-hydroxyrisperidone are dose proportional over the dosing range of 1 to 16 mg daily (0.5 to 8 mg twice daily). Following oral administration of solution or tablet, mean peak plasma concentrations of risperidone occurred at about 1 hour. Peak concentrations of 9-hydroxyrisperidone occurred at about 3 hours in extensive metabolizers, and 17 hours in poor metabolizers. Steady-state concentrations of risperidone are reached in 1 day in extensive metabolizers and would be expected to reach steady-state in about 5 days in poor metabolizers. Steady-state concentrations of 9-hydroxyrisperidone are reached in 5 to 6 days (measured in extensive metabolizers). Food Effect Food does not affect either the rate or extent of absorption of risperidone. Thus, risperidone oral solution can be given with or without meals. Distribution Risperidone is rapidly distributed. The volume of distribution is 1 to 2 L/kg. In plasma, risperidone is bound to albumin and α 1 -acid glycoprotein. The plasma protein binding of risperidone is approximately 90%, and that of its major metabolite, 9-hydroxyrisperidone, is 77%. Neither risperidone nor 9-hydroxyrisperidone displaces each other from plasma binding sites. High therapeutic concentrations of sulfamethazine (100 mcg/mL), warfarin (10 mcg/mL), and carbamazepine (10 mcg/mL) caused only a slight increase in the free fraction of risperidone at 10 ng/mL and 9-hydroxyrisperidone at 50 ng/mL, changes of unknown clinical significance. Elimination Metabolism Risperidone is extensively metabolized in the liver. The main metabolic pathway is through hydroxylation of risperidone to 9-hydroxyrisperidone by the enzyme, CYP 2D6. A minor metabolic pathway is through N -dealkylation. The main metabolite, 9-hydroxyrisperidone, has similar pharmacological activity as risperidone. Consequently, the clinical effect of the drug results from the combined concentrations of risperidone plus 9-hydroxyrisperidone. CYP 2D6, also called debrisoquin hydroxylase, is the enzyme responsible for metabolism of many neuroleptics, antidepressants, antiarrhythmics, and other drugs. CYP 2D6 is subject to genetic polymorphism (about 6% to 8% of Caucasians, and a very low percentage of Asians, have little or no activity and are “poor metabolizers”) and to inhibition by a variety of substrates and some non-substrates, notably quinidine. Extensive CYP 2D6 metabolizers convert risperidone rapidly into 9-hydroxyrisperidone, whereas poor CYP 2D6 metabolizers convert it much more slowly. Although extensive metabolizers have lower risperidone and higher 9-hydroxyrisperidone concentrations than poor metabolizers, the pharmacokinetics of risperidone and 9-hydroxyrisperidone combined, after single and multiple doses, are similar in extensive and poor metabolizers. Excretion Risperidone and its metabolites are eliminated via the urine and, to a much lesser extent, via the feces. As illustrated by a mass balance study of a single 1 mg oral dose of 14 C-risperidone administered as solution to three healthy male volunteers, total recovery of radioactivity at 1 week was 84%, including 70% in the urine and 14% in the feces. The apparent half-life of risperidone was 3 hours (CV = 30%) in extensive metabolizers and 20 hours (CV = 40%) in poor metabolizers. The apparent half-life of 9-hydroxyrisperidone was about 21 hours (CV = 20%) in extensive metabolizers and 30 hours (CV = 25%) in poor metabolizers. The pharmacokinetics of risperidone and 9-hydroxyrisperidone combined, after single and multiple doses, were similar in extensive and poor metabolizers, with an overall mean elimination half-life of about 20 hours. Drug Interaction Studies Risperidone could be subject to two kinds of drug-drug interactions. First, inhibitors of CYP 2D6 interfere with conversion of risperidone to 9-hydroxyrisperidone [ see Drug Interactions (7) ]. This occurs with quinidine, giving essentially all recipients a risperidone pharmacokinetic profile typical of poor metabolizers. The therapeutic benefits and adverse effects of risperidone in patients receiving quinidine have not been evaluated, but observations in a modest number (n≅70) of poor metabolizers given risperidone do not suggest important differences between poor and extensive metabolizers. Second, co-administration of known enzyme inducers (e.g., carbamazepine, phenytoin, rifampin, and phenobarbital) with risperidone may cause a decrease in the combined plasma concentrations of risperidone and 9-hydroxyrisperidone [ see Drug Interactions (7) ]. It would also be possible for risperidone to interfere with metabolism of other drugs metabolized by CYP 2D6. Relatively weak binding of risperidone to the enzyme suggests this is unlikely [ see Drug Interactions (7) ]. In vitro studies indicate that risperidone is a relatively weak inhibitor of CYP 2D6. Therefore, risperidone is not expected to substantially inhibit the clearance of drugs that are metabolized by this enzymatic pathway. In drug interaction studies, risperidone did not significantly affect the pharmacokinetics of donepezil and galantamine, which are metabolized by CYP 2D6. In vitro studies demonstrated that drugs metabolized by other CYP isozymes, including 1A1, 1A2, 2C9, 2C19, and 3A4, are only weak inhibitors of risperidone metabolism. Specific Populations Renal and Hepatic Impairment [ See Use in Specific Populations (8.6 ; and 8.7 ) ]. Elderly In healthy elderly subjects, renal clearance of both risperidone and 9-hydroxyrisperidone was decreased, and elimination half-lives were prolonged compared to young healthy subjects. Dosing should be modified accordingly in the elderly patients [ see Use in Specific Populations (8.5) ]. Pediatric The pharmacokinetics of risperidone and 9-hydroxyrisperidone in children were similar to those in adults after correcting for the difference in body weight. Race and Gender Effects No specific pharmacokinetic study was conducted to investigate race and gender effects, but a population pharmacokinetic analysis did not identify important differences in the disposition of risperidone due to gender (whether corrected for body weight or not) or race.
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action The mechanism of action of risperidone in schizophrenia is unclear. The drug's therapeutic activity in schizophrenia could be mediated through a combination of dopamine Type 2 (D 2 ) and serotonin Type 2 (5HT 2 ) receptor antagonism. The clinical effect from risperidone results from the combined concentrations of risperidone and its major metabolite, 9-hydroxyrisperidone (paliperidone) [ see Clinical Pharmacology (12.3) ]. Antagonism at receptors other than D 2 and 5HT 2 may explain some of the other effects of risperidone [ see Clinical Pharmacology (12.1) ].
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics Risperidone is a monoaminergic antagonist with high affinity (Ki of 0.12 to 7.3 nM) for the serotonin Type 2 (5HT 2 ), dopamine Type 2 (D 2 ), α 1 and α 2 adrenergic, and H 1 histaminergic receptors. Risperidone showed low to moderate affinity (Ki of 47 to 253 nM) for the serotonin 5HT 1C , 5HT 1D , and 5HT 1A receptors, weak affinity (Ki of 620 to 800 nM) for the dopamine D 1 and haloperidol-sensitive sigma site, and no affinity (when tested at concentrations >10 -5 M) for cholinergic muscarinic or β 1 and β 2 adrenergic receptors.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Absorption Risperidone is well absorbed. The absolute oral bioavailability of risperidone is 70% (CV = 25%). The relative oral bioavailability of risperidone from a tablet is 94% (CV = 10%) when compared to a solution. Pharmacokinetic studies showed that Risperidone Orally Disintegrating Tablets and Risperidone Oral Solution are bioequivalent to Risperidone Tablets. Plasma concentrations of risperidone, its major metabolite, 9-hydroxyrisperidone, and risperidone plus 9-hydroxyrisperidone are dose proportional over the dosing range of 1 to 16 mg daily (0.5 to 8 mg twice daily). Following oral administration of solution or tablet, mean peak plasma concentrations of risperidone occurred at about 1 hour. Peak concentrations of 9-hydroxyrisperidone occurred at about 3 hours in extensive metabolizers, and 17 hours in poor metabolizers. Steady-state concentrations of risperidone are reached in 1 day in extensive metabolizers and would be expected to reach steady-state in about 5 days in poor metabolizers. Steady-state concentrations of 9-hydroxyrisperidone are reached in 5 to 6 days (measured in extensive metabolizers). Food Effect Food does not affect either the rate or extent of absorption of risperidone. Thus, risperidone oral solution can be given with or without meals. Distribution Risperidone is rapidly distributed. The volume of distribution is 1 to 2 L/kg. In plasma, risperidone is bound to albumin and α 1 -acid glycoprotein. The plasma protein binding of risperidone is approximately 90%, and that of its major metabolite, 9-hydroxyrisperidone, is 77%. Neither risperidone nor 9-hydroxyrisperidone displaces each other from plasma binding sites. High therapeutic concentrations of sulfamethazine (100 mcg/mL), warfarin (10 mcg/mL), and carbamazepine (10 mcg/mL) caused only a slight increase in the free fraction of risperidone at 10 ng/mL and 9-hydroxyrisperidone at 50 ng/mL, changes of unknown clinical significance. Elimination Metabolism Risperidone is extensively metabolized in the liver. The main metabolic pathway is through hydroxylation of risperidone to 9-hydroxyrisperidone by the enzyme, CYP 2D6. A minor metabolic pathway is through N -dealkylation. The main metabolite, 9-hydroxyrisperidone, has similar pharmacological activity as risperidone. Consequently, the clinical effect of the drug results from the combined concentrations of risperidone plus 9-hydroxyrisperidone. CYP 2D6, also called debrisoquin hydroxylase, is the enzyme responsible for metabolism of many neuroleptics, antidepressants, antiarrhythmics, and other drugs. CYP 2D6 is subject to genetic polymorphism (about 6% to 8% of Caucasians, and a very low percentage of Asians, have little or no activity and are “poor metabolizers”) and to inhibition by a variety of substrates and some non-substrates, notably quinidine. Extensive CYP 2D6 metabolizers convert risperidone rapidly into 9-hydroxyrisperidone, whereas poor CYP 2D6 metabolizers convert it much more slowly. Although extensive metabolizers have lower risperidone and higher 9-hydroxyrisperidone concentrations than poor metabolizers, the pharmacokinetics of risperidone and 9-hydroxyrisperidone combined, after single and multiple doses, are similar in extensive and poor metabolizers. Excretion Risperidone and its metabolites are eliminated via the urine and, to a much lesser extent, via the feces. As illustrated by a mass balance study of a single 1 mg oral dose of 14 C-risperidone administered as solution to three healthy male volunteers, total recovery of radioactivity at 1 week was 84%, including 70% in the urine and 14% in the feces. The apparent half-life of risperidone was 3 hours (CV = 30%) in extensive metabolizers and 20 hours (CV = 40%) in poor metabolizers. The apparent half-life of 9-hydroxyrisperidone was about 21 hours (CV = 20%) in extensive metabolizers and 30 hours (CV = 25%) in poor metabolizers. The pharmacokinetics of risperidone and 9-hydroxyrisperidone combined, after single and multiple doses, were similar in extensive and poor metabolizers, with an overall mean elimination half-life of about 20 hours. Drug Interaction Studies Risperidone could be subject to two kinds of drug-drug interactions. First, inhibitors of CYP 2D6 interfere with conversion of risperidone to 9-hydroxyrisperidone [ see Drug Interactions (7) ]. This occurs with quinidine, giving essentially all recipients a risperidone pharmacokinetic profile typical of poor metabolizers. The therapeutic benefits and adverse effects of risperidone in patients receiving quinidine have not been evaluated, but observations in a modest number (n≅70) of poor metabolizers given risperidone do not suggest important differences between poor and extensive metabolizers. Second, co-administration of known enzyme inducers (e.g., carbamazepine, phenytoin, rifampin, and phenobarbital) with risperidone may cause a decrease in the combined plasma concentrations of risperidone and 9-hydroxyrisperidone [ see Drug Interactions (7) ]. It would also be possible for risperidone to interfere with metabolism of other drugs metabolized by CYP 2D6. Relatively weak binding of risperidone to the enzyme suggests this is unlikely [ see Drug Interactions (7) ]. In vitro studies indicate that risperidone is a relatively weak inhibitor of CYP 2D6. Therefore, risperidone is not expected to substantially inhibit the clearance of drugs that are metabolized by this enzymatic pathway. In drug interaction studies, risperidone did not significantly affect the pharmacokinetics of donepezil and galantamine, which are metabolized by CYP 2D6. In vitro studies demonstrated that drugs metabolized by other CYP isozymes, including 1A1, 1A2, 2C9, 2C19, and 3A4, are only weak inhibitors of risperidone metabolism. Specific Populations Renal and Hepatic Impairment [ See Use in Specific Populations (8.6 ; and 8.7 ) ]. Elderly In healthy elderly subjects, renal clearance of both risperidone and 9-hydroxyrisperidone was decreased, and elimination half-lives were prolonged compared to young healthy subjects. Dosing should be modified accordingly in the elderly patients [ see Use in Specific Populations (8.5) ]. Pediatric The pharmacokinetics of risperidone and 9-hydroxyrisperidone in children were similar to those in adults after correcting for the difference in body weight. Race and Gender Effects No specific pharmacokinetic study was conducted to investigate race and gender effects, but a population pharmacokinetic analysis did not identify important differences in the disposition of risperidone due to gender (whether corrected for body weight or not) or race.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS Risperidone oral solution is contraindicated in patients with a known hypersensitivity to either risperidone or paliperidone, or to any of the excipients in the risperidone formulation. Hypersensitivity reactions, including anaphylactic reactions and angioedema, have been reported in patients treated with risperidone and in patients treated with paliperidone. Paliperidone is a metabolite of risperidone. Known hypersensitivity to risperidone, paliperidone, or to any excipients in risperidone oral solution ( 4)
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION Risperidone oral solution contains risperidone, an atypical antipsychotic belonging to the chemical class of benzisoxazole derivatives. The chemical designation is 3-[2-[4-(6-fluoro-1,2-benzisoxazol-3-yl)- 1-piperidinyl]ethyl]-6,7,8,9-tetrahydro-2-methyl-4H-pyrido[1,2-a]pyrimidin-4-one. Its molecular formula is C 23 H 27 FN 4 O 2 and its molecular weight is 410.49. The structural formula is: ; Risperidone is a white to slightly beige powder. It is practically insoluble in water, freely soluble in methylene chloride, and soluble in methanol and 0.1 N HCl. Risperidone is also available as a 1 mg/mL oral solution. Risperidone Oral Solution contains the following inactive ingredients: benzoic acid, sodium hydroxide, sorbitol solution, tartaric acid, and purified water. Figure 1
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.DOSAGE AND ADMINISTRATION Recommended daily dosage: Initial Dose Target Dose Effective Dose Range Schizophrenia: adults ( 2.1) 2 mg 4 to 8 mg 4 to 16 mg Schizophrenia: adolescents ( 2.1) 0.5 mg 3 mg 1 to 6 mg Bipolar mania: adults ( 2.2) 2 to 3 mg 1 to 6 mg 1 to 6 mg Bipolar mania: in children and adolescents ( 2.2) 0.5 mg 1 to 2.5 mg 1 to 6 mg Irritability associated;with autistic disorder ( 2.3) 0.25 mg (Weight < 20 kg) 0.5 mg (Weight ≥ 20 kg) 0.5 mg (< 20 kg) 1 mg (≥ 20 kg) ;0.5 to 3 mg Severe Renal or Hepatic Impairment in Adults: Use a lower starting dose of 0.5 mg twice daily. May increase to dosages above 1.5 mg twice daily at intervals of at least one week. ( 2.4) Oral Solution: Can be administered directly from calibrated oral dosing syringe or mixed with beverage (water, coffee, orange juice, or low-fat milk). ( 2.6) Table 1; Recommended Daily Dosage by Indication ; Initial Dose Titration (Increments) ; ; Target Dose ; Effective Dose Range Schizophrenia: adults ( 2.1) ;2 mg ;1 to 2 mg ;4 to 8 mg ;4 to 16 mg Schizophrenia:; adolescents ( 2.1) ;0.5 mg ;0.5 to 1 mg ;3 mg ;1 to 6 mg Bipolar mania: adults ( 2.2) ;2 to 3 mg ;1 mg ;1 to 6 mg ;1 to 6 mg Bipolar mania: children and adolescents ( 2.2) ;0.5 mg ;0.5 to 1 mg ;1 to 2.5 mg ;1 to 6 mg Irritability in autistic disorder ( 2.3) 0.25 mg;Can increase to 0.5 mg by Day 4: (body weight less than 20 kg) 0.5 mg Can increase to 1 mg by Day 4: (body weight greater than or equal to 20 kg) After Day 4, at intervals of > 2 weeks: 0.25 mg (body weight less than 20 kg) 0.5 mg (body weight greater than or equal to 20 kg) 0.5 mg: (body weight less than 20 kg) 1 mg: (body weight greater than or equal to 20 kg) ;0.5 to 3 mg Severe Renal and Hepatic Impairment in Adults: use a lower starting dose of 0.5 mg twice daily. May increase to dosages above 1.5 mg twice daily at intervals of one week or longer.
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS Risperidone oral solution is available in a 1 mg/mL strength. Oral solution: 1 mg per mL ;( 3);
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.INDICATIONS AND USAGE 1.1 Schizophrenia Risperidone oral solution is indicated for the treatment of schizophrenia. Efficacy was established in 4 short-term trials in adults, 2 short-term trials in adolescents (ages 13 to 17 years), and one long-term maintenance trial in adults [see CLINICAL STUDIES (14.1)]. 1.2 Bipolar Mania Monotherapy Risperidone oral solution is indicated for the treatment of acute manic or mixed episodes associated with Bipolar I Disorder. Efficacy was established in 2 short-term trials in adults and one short-term trial in children and adolescents (ages 10 to 17 years) [see CLINICAL STUDIES (14.2)]. Adjunctive Therapy Risperidone oral solution adjunctive therapy with lithium or valproate is indicated for the treatment of acute manic or mixed episodes associated with Bipolar I Disorder. Efficacy was established in one short-term trial in adults [see CLINICAL STUDIES (14.3)]. 1.3 Irritability Associated with Autistic Disorder Risperidone oral solution is indicated for the treatment of irritability associated with autistic disorder, including symptoms of aggression towards others, deliberate self-injuriousness, temper tantrums, and quickly changing moods. Efficacy was established in 3 short-term trials in children and adolescents (ages 5 to 17 years) [see CLINICAL STUDIES (14.4)].
Spl product data elements
Usually a list of ingredients in a drug product.Risperidone Risperidone BENZOIC ACID SODIUM HYDROXIDE SORBITOL SOLUTION TARTARIC ACID WATER RISPERIDONE RISPERIDONE colorless
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis Risperidone was administered in the diet at doses of 0.63, 2.5, and 10 mg/kg for 18 months to mice and for 25 months to rats. These doses are equivalent to approximately 0.2, 0.75, and 3 times (mice) and 0.4, 1.5, and 6 times (rats) the MRHD of 16 mg/day, based on mg/m 2 body surface area. A maximum tolerated dose was not achieved in male mice. There were statistically significant increases in pituitary gland adenomas, endocrine pancreas adenomas, and mammary gland adenocarcinomas. The table below summarizes the multiples of the human dose on a mg/m 2 (mg/kg) basis at which these tumors occurred. ; Multiples of Maximum Human Dose in mg/m 2 (mg/kg) ; Tumor Type ; Species ; Sex ; Lowest Effect Level ; Highest No-Effect Level ;Pituitary adenomas ;mouse ;Female ;0.75 (9.4) ;0.2 (2.4) ;Endocrine pancreas adenomas ;rat ;Male ;1.5 (9.4) ;0.4 (2.4) ;Mammary gland adenocarcinomas ;mouse ;Female ;0.2 (2.4) ;none ;rat ;Female ;0.4 (2.4) ;none ;rat ;Male ;6 (37.5) ;1.5 (9.4) ;Mammary gland neoplasm, Total ;rat ;Male ;1.5 (9.4) ;0.4 (2.4) Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the risperidone carcinogenicity studies; however, measurements during subchronic toxicity studies showed that risperidone elevated serum prolactin levels 5 to 6 fold in mice and rats at the same doses used in the carcinogenicity studies. An increase in mammary, pituitary, and endocrine pancreas neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin-mediated. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unclear [ see Warnings and Precautions (5.6) ]. Mutagenesis No evidence of mutagenic or clastogenic potential for risperidone was found in the in vitro tests of Ames gene mutation, the mouse lymphoma assay, rat hepatocyte DNA-repair assay, the chromosomal aberration test in human lymphocytes, Chinese hamster ovary cells, or in the in vivo oral micronucleus test in mice and the sex-linked recessive lethal test in Drosophila . Impairment of Fertility Oral risperidone (0.16 to 5 mg/kg) impaired mating, but not fertility, in rat reproductive studies at doses 0.1 to 3 times the MRHD of 16 mg/day based;on mg/m 2 body surface area. The effect appeared to be in females, since impaired mating behavior was not noted in the male fertility study. In a subchronic study in Beagle dogs in which risperidone was administered orally at doses of 0.31 to 5 mg/kg, sperm motility and concentration were decreased at doses 0.6 to 10 times the MRHD based on mg/m 2 body surface area. Dose-related decreases were also noted in serum testosterone at the same doses. Serum testosterone and sperm parameters partially recovered, but remained decreased after treatment was discontinued. A no-effect dose could not be determined in either rat or dog.
| ;Pituitary adenomas | ;mouse | ;Female | ;0.75 (9.4) | ;0.2 (2.4) |
| ;Endocrine pancreas adenomas | ;rat | ;Male | ;1.5 (9.4) | ;0.4 (2.4) |
| ;Mammary gland adenocarcinomas | ;mouse | ;Female | ;0.2 (2.4) | ;none |
| ;rat | ;Female | ;0.4 (2.4) | ;none | |
| ;rat | ;Male | ;6 (37.5) | ;1.5 (9.4) | |
| ;Mammary gland neoplasm, Total | ;rat | ;Male | ;1.5 (9.4) | ;0.4 (2.4) |
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility Carcinogenesis Risperidone was administered in the diet at doses of 0.63, 2.5, and 10 mg/kg for 18 months to mice and for 25 months to rats. These doses are equivalent to approximately 0.2, 0.75, and 3 times (mice) and 0.4, 1.5, and 6 times (rats) the MRHD of 16 mg/day, based on mg/m 2 body surface area. A maximum tolerated dose was not achieved in male mice. There were statistically significant increases in pituitary gland adenomas, endocrine pancreas adenomas, and mammary gland adenocarcinomas. The table below summarizes the multiples of the human dose on a mg/m 2 (mg/kg) basis at which these tumors occurred. ; Multiples of Maximum Human Dose in mg/m 2 (mg/kg) ; Tumor Type ; Species ; Sex ; Lowest Effect Level ; Highest No-Effect Level ;Pituitary adenomas ;mouse ;Female ;0.75 (9.4) ;0.2 (2.4) ;Endocrine pancreas adenomas ;rat ;Male ;1.5 (9.4) ;0.4 (2.4) ;Mammary gland adenocarcinomas ;mouse ;Female ;0.2 (2.4) ;none ;rat ;Female ;0.4 (2.4) ;none ;rat ;Male ;6 (37.5) ;1.5 (9.4) ;Mammary gland neoplasm, Total ;rat ;Male ;1.5 (9.4) ;0.4 (2.4) Antipsychotic drugs have been shown to chronically elevate prolactin levels in rodents. Serum prolactin levels were not measured during the risperidone carcinogenicity studies; however, measurements during subchronic toxicity studies showed that risperidone elevated serum prolactin levels 5 to 6 fold in mice and rats at the same doses used in the carcinogenicity studies. An increase in mammary, pituitary, and endocrine pancreas neoplasms has been found in rodents after chronic administration of other antipsychotic drugs and is considered to be prolactin-mediated. The relevance for human risk of the findings of prolactin-mediated endocrine tumors in rodents is unclear [ see Warnings and Precautions (5.6) ]. Mutagenesis No evidence of mutagenic or clastogenic potential for risperidone was found in the in vitro tests of Ames gene mutation, the mouse lymphoma assay, rat hepatocyte DNA-repair assay, the chromosomal aberration test in human lymphocytes, Chinese hamster ovary cells, or in the in vivo oral micronucleus test in mice and the sex-linked recessive lethal test in Drosophila . Impairment of Fertility Oral risperidone (0.16 to 5 mg/kg) impaired mating, but not fertility, in rat reproductive studies at doses 0.1 to 3 times the MRHD of 16 mg/day based;on mg/m 2 body surface area. The effect appeared to be in females, since impaired mating behavior was not noted in the male fertility study. In a subchronic study in Beagle dogs in which risperidone was administered orally at doses of 0.31 to 5 mg/kg, sperm motility and concentration were decreased at doses 0.6 to 10 times the MRHD based on mg/m 2 body surface area. Dose-related decreases were also noted in serum testosterone at the same doses. Serum testosterone and sperm parameters partially recovered, but remained decreased after treatment was discontinued. A no-effect dose could not be determined in either rat or dog.
| ;Pituitary adenomas | ;mouse | ;Female | ;0.75 (9.4) | ;0.2 (2.4) |
| ;Endocrine pancreas adenomas | ;rat | ;Male | ;1.5 (9.4) | ;0.4 (2.4) |
| ;Mammary gland adenocarcinomas | ;mouse | ;Female | ;0.2 (2.4) | ;none |
| ;rat | ;Female | ;0.4 (2.4) | ;none | |
| ;rat | ;Male | ;6 (37.5) | ;1.5 (9.4) | |
| ;Mammary gland neoplasm, Total | ;rat | ;Male | ;1.5 (9.4) | ;0.4 (2.4) |
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.DRUG: Risperidone GENERIC: Risperidone DOSAGE: SOLUTION ADMINSTRATION: ORAL NDC: 70518-3741-0 NDC: 70518-3741-1 COLOR: white PACKAGING: 2 mL in 1 CUP, UNIT-DOSE OUTER PACKAGING: 10 in 1 BOX ACTIVE INGREDIENT(S): RISPERIDONE 1mg in 1mL INACTIVE INGREDIENT(S): BENZOIC ACID SODIUM HYDROXIDE SORBITOL SOLUTION TARTARIC ACID WATER Remedy_Label MM2
Recent major changes
A list of the section(s) that contain substantive changes that have been approved by FDA in the product labeling. The headings and subheadings, if appropriate, affected by the change are listed together with each section’s identifying number and the month and year on which the change was incorporated in the labeling.Warnings and Precautions ( 5.3, 5.4) 2/2021 Dosage and Administration ( 2.6) 3/2022
Spl unclassified section
Information not classified as belonging to one of the other fields. Approximately 40% of labeling with effective_time between June 2009 and August 2014 have information in this field.5.5 Metabolic Changes Atypical antipsychotic drugs have been associated with metabolic changes that may increase cardiovascular/cerebrovascular risk. These metabolic changes include hyperglycemia, dyslipidemia, and body weight gain. While all of the drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile. Hyperglycemia and Diabetes Mellitus Hyperglycemia and diabetes mellitus, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, have been reported in patients treated with atypical antipsychotics including risperidone. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of treatment-emergent hyperglycemia-related adverse events in patients treated with the atypical antipsychotics. Precise risk estimates for hyperglycemia-related adverse events in patients treated with atypical antipsychotics are not available. Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics, including risperidone, should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics, including risperidone, should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics, including risperidone, should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics, including risperidone, should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic, including risperidone, was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of risperidone. Pooled data from three double-blind, placebo-controlled schizophrenia studies and four double-blind, placebo-controlled bipolar monotherapy studies are presented in Table 2. Table 2.; Change in Random Glucose from Seven Placebo-Controlled, 3- to 8-Week, Fixed- or Flexible-Dose Studies in Adult Subjects with Schizophrenia or Bipolar Mania ;Risperidone ; 1 to 8 mg/day ; >8 to 16 mg/day ; Mean change from baseline (mg/dL) &; n = 748 ; n = 164 ;Serum Glucose ;-1.4 ;0.8 ;0.6 ; Proportion of patients with shifts ;Serum Glucose (<140 mg/dL to ≥ 200 mg/dL) ;0.6% (3/525) 0.4% (3/702) 0% (0/158) In longer-term, controlled and uncontrolled studies, risperidone was associated with a mean change in glucose of +2.8 mg/dL at Week 24 (n = 151) and +4.1 mg/dL at Week 48 (n = 50). Data from the placebo-controlled 3- to 6-week study in children and adolescents with schizophrenia (13 to 17 years of age), bipolar mania (10 to 17 years of age), or autistic disorder (5 to 17 years of age) are presented in Table 3. Table 3.; Change in Fasting Glucose from Three Placebo-Controlled, 3- to 6-Week, Fixed-Dose Studies in Children and Adolescents with Schizophrenia (13 to 17 years of age), Bipolar Mania (10 to 17 years of age), or Autistic Disorder (5 to 17 years of age) ; ; Risperidone ; mg/day ; Mean change from baseline (mg/dL) ; n = 76 ; n = 135 ;Serum Glucose ;-1.3 ;2.6 ; Proportion of patients with shifts ;Serum Glucose (<100 mg/dL to ≥126 mg/dL) ;0% (0/64) ;0.8% (1/120) In longer-term, uncontrolled, open-label extension pediatric studies, risperidone was associated with a mean change in fasting glucose of +5.2 mg/dL at Week 24 (n = 119). Dyslipidemia Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics. Pooled data from 7 placebo-controlled, 3- to 8- week, fixed- or flexible-dose studies in adult subjects with schizophrenia or bipolar mania are presented in Table 4. Table 4.; Change in Random Lipids from Seven Placebo-Controlled, 3- to 8-Week, Fixed- or Flexible-Dose Studies in Adult Subjects with Schizophrenia or Bipolar Mania ; Risperidone ; ; Placebo ; 1 to 8 mg/day ; >8 to16 mg/day ; Mean change from baseline (mg/dL) Cholesterol ;Change from baseline ; n = 559 ;0.6 ; n = 742 ;6.9 ; n = 156 ;1.8 Triglycerides ;Change from baseline ; n = 183 ;-17.4 ; n = 307 ;-4.9 ; n = 123 ;-8.3 Proportion of patients with shifts Cholesterol ;(<200 mg/dL to ≥240 mg/dL) ;2.7% (10/368) ;4.3% (22/516) ;6.3% (6/96) Triglycerides ;(<500 mg/dL to ≥500 mg/dL) ;1.1% (2/180) ;2.7% (8/301) ;2.5% (3/121) In longer-term, controlled and uncontrolled studies, risperidone was associated with a mean change in (a) non-fasting cholesterol of +4.4 mg/dL at Week 24 (n = 231) and +5.5 mg/dL at Week 48 (n = 86); and (b) non-fasting triglycerides of +19.9 mg/dL at Week 24 (n = 52). Pooled data from 3 placebo-controlled, 3- to 6-week, fixed-dose studies in children and adolescents with schizophrenia (13 to 17 years of age), bipolar mania (10 to 17 years of age), or autistic disorder (5 to 17 years of age) are presented in Table 5. Table 5.; Change in Fasting Lipids from Three Placebo-Controlled, 3- to 6-Week, Fixed-Dose Studies in Children and Adolescents with Schizophrenia (13 to 17 Years of Age), Bipolar Mania (10 to 17 Years of Age), or Autistic Disorder (5 to 17 Years of Age) Placebo; ; Risperidone 0.5 to 6 mg/day ; Mean change from baseline (mg/dL) Cholesterol ;Change from baseline ; n = 74 ;0.3 ; n = 133 ;-0.3 LDL ;Change from baseline ; n = 22 ;3.7 ; n = 22 ;0.5 HDL ;Change from baseline ; n = 22 ;1.6 ; n = 22 ;-1.9 Triglycerides Change from baseline ; n;= 77 ;-9 ; n = 138 ;-2.6 ; Proportion of patients with shifts Cholesterol ;(<170 mg/dL to ≥200 mg/dL) ;2.4% (1/42) ;3.8% (3/80) LDL ;(<110 mg/dL to ≥130 mg/dL) ;0% (0/16) ;0% (0/16) HDL ;(≥40 mg/dL to <40 mg/dL) ;0% (0/19) ;10% (2/20) Triglycerides ;(<150 mg/dL to ≥200 mg/dL) ;1.5% (1/65) ;7.1% (8/113) In longer-term, uncontrolled, open-label extension pediatric studies, risperidone was associated with a mean change in (a) fasting cholesterol of +2.1 mg/dL at Week 24 (n = 114); (b) fasting LDL of -0.2 mg/dL at Week 24 (n = 103); (c) fasting HDL of +0.4 mg/dL at Week 24 (n = 103); and (d) fasting triglycerides of +6.8 mg/dL at Week 24 (n = 120). Weight Gain Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended. Data on mean changes in body weight and the proportion of subjects meeting a weight gain criterion of 7% or greater of body weight from 7 placebo-controlled, 3- to 8- week, fixed- or flexible-dose studies in adult subjects with schizophrenia or bipolar mania are presented in Table 6. Table 6.; Mean Change in Body Weight (kg) and the Proportion of Subjects with ≥ 7% Gain in Body Weight From Seven Placebo-Controlled, 3- to 8-Week, Fixed- or Flexible-Dose Studies in Adult Subjects With Schizophrenia or Bipolar Mania ; Risperidone ; ;Placebo (n = 597) ; 1 to 8 mg/day (n = 769) ; >8 to16 mg/day (n = 158) ; Weight (kg) ;Change from baseline ;-0.3 ;0.7 ;2.2 ; Weight Gain ;≥7% increase from baseline ;2.9% ;8.7% ;20.9% In longer-term, controlled and uncontrolled studies, risperidone was associated with a mean change in weight of +4.3 kg at Week 24 (n = 395) and +5.3 kg at Week 48 (n = 203). Data on mean changes in body weight and the proportion of subjects meeting the criterion of ≥7% gain in body weight from nine placebo-controlled, 3- to 8-week, fixed-dose studies in children and adolescents with schizophrenia (13 to 17 years of age), bipolar mania (10 to 17 years of age), autistic disorder (5 to 17 years of age), or other psychiatric disorders (5 to 17 years of age) are presented in Table 7. Table 7.; Mean Change in Body Weight (kg) and the Proportion of Subjects With ≥7% Gain in Body Weight From Nine Placebo-Controlled, 3- to 8-Week, Fixed-Dose Studies in Children and Adolescents With Schizophrenia (13 to 17 Years of Age), Bipolar Mania (10 to 17 Years of Age), Autistic Disorder (5 to 17 Years of Age) or Other Psychiatric Disorders (5 to 17 Years of Age) ; Placebo (n = 375) ; Risperidone 0.5 to 6 mg/day (n = 448) ; Weight (kg) ;Change from baseline ;0.6% ;2% ; Weight Gain ;≥7% increase from baseline ;6.9% ;32.6% In longer-term, uncontrolled, open-label extension pediatric studies, risperidone was associated with a mean change in weight of +5.5 kg at Week 24 (n = 748) and +8 kg at Week 48 (n=242). In a long-term, open-label extension study in adolescent patients with schizophrenia, weight increase was reported as a treatment-emergent adverse event in 14% of patients. In 103 adolescent patients with schizophrenia, a mean increase of 9 kg was observed after 8 months of risperidone treatment. The majority of that increase was observed within the first 6 months. The average percentiles at baseline and 8 months, respectively, were 56 and 72 for weight, 55 and 58 for height, and 51 and 71 for body mass index. In long-term, open-label trials (studies in patients with autistic disorder or other psychiatric disorders), a mean increase of 7.5 kg after 12 months of risperidone treatment was observed, which was higher than the expected normal weight gain (approximately 3 to 3.5 kg per year adjusted for age, based on Centers for Disease Control and Prevention normative data). The majority of that increase occurred within the first 6 months of exposure to risperidone. The average percentiles at baseline and 12 months, respectively, were 49 and 60 for weight, 48 and 53 for height, and 50 and 62 for body mass index. In one 3-week, placebo-controlled trial in children and adolescent patients with acute manic or mixed episodes of bipolar I disorder, increases in body weight were higher in the risperidone groups than the placebo group, but not dose related (1.90 kg in the risperidone 0.5 to 2.5 mg group, 1.44 kg in the risperidone 3 to 6 mg group, and 0.65 kg in the placebo group). A similar trend was observed in the mean change from baseline in body mass index. When treating pediatric patients with risperidone for any indication, weight gain should be assessed against that expected with normal growth.
Risperidone: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION Advise patients using Risperidone oral solution to read the FDA-approved patient labeling (Instructions for Use) for Risperidone oral solution. Physicians are advised to discuss the following issues with patients for whom they prescribe risperidone. Neuroleptic Malignant Syndrome (NMS) Counsel patients about a potentially fatal adverse reaction, Neuroleptic Malignant Syndrome (NMS), that has been reported in association with administration of antipsychotic drugs. Advise patients, family members, or caregivers to contact the healthcare provider or report to the emergency room if they experience signs and symptoms of NMS, including hyperpyrexia, muscle rigidity, altered mental status including delirium, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia) [ see Warnings and Precautions (5.3) ]. Tardive Dyskinesia Counsel patients on the signs and symptoms of tardive dyskinesia and to contact their healthcare provider if these abnormal movements occur [ see Warnings and Precautions (5.4) ]. Metabolic Changes Educate patients about the risk of metabolic changes, how to recognize symptoms of hyperglycemia and diabetes mellitus, and the need for specific monitoring, including blood glucose, lipids, and weight [ see W arnings and Precautions (5.5) ]. Orthostatic Hypotension Educate patients about the risk of orthostatic hypotension and syncope, particularly at the time of initiating treatment, re-initiating treatment, or increasing the dose [ see Warnings and Precautions (5.7) ]. Leukopenia/Neutropenia Advise patients with a pre-existing low WBC or a history of drug induced leukopenia/neutropenia they should have their CBC monitored while taking risperidone [ see Wa rnings and Precautions (5.9) ]. Hyperprolactinemia Counsel patients on signs and symptoms of hyperprolactinemia that may be associated with chronic use of risperidone. Advise them to seek medical attention if they experience any of the following: amenorrhea or galactorrhea in females, erectile dysfunction or gynecomastia in males. [See Warnings and Precautions (5.6) ] . Interference with Cognitive and Motor Performance Caution patients about performing activities requiring mental alertness, such as operating hazardous machinery, or operating a motor vehicle until they are reasonably certain that risperidone therapy does not affect them adversely [ see Warnings and Precautions (5.10) ]. Priapism Advise patients of the possibility of painful or prolonged penile erections (priapism). Instruct the patient to seek immediate medical attention in the event of priapism [see Warnings and Precautions (5.13) ]. Heat Exposure and Dehydration Counsel patients regarding appropriate care in avoiding overheating and dehydration [ see Warnings and Precautions (5.14) ]. Concomitant Medication Advise patients to inform their healthcare providers if they are taking, or plan to take any prescription or over-the-counter drugs, as a potential for interactions [ see Drug Interactions (7) ]. Alcohol Advise patients to avoid alcohol while taking risperidone [ see Drug Interactions (7.2) ]. Pregnancy Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during treatment with risperidone. Advise patients that risperidone may cause extrapyramidal and/or withdrawal symptoms in a neonate. Advise patients that there is a pregnancy registry that monitors pregnancy outcomes in women exposed to risperidone during pregnancy [ see Use in Specific Populations (8.1) ]. Lactation Advise breastfeeding women using risperidone to monitor infants for somnolence, failure to thrive, jitteriness, and extrapyramidal symptoms (tremors and abnormal muscle movements) and to seek medical care if they notice these signs [ see Use in Specific Populations (8.2) ]. Infertility Advise females of reproductive potential that risperidone may impair fertility due to an increase in serum prolactin levels. The effects on fertility are reversible [ see Use in Specific Populations (8.3) ]. Repackaged By / Distributed By: RemedyRepack Inc. 625 Kolter Drive, Indiana, PA 15701 (724) 465-8762
Spl patient package insert
Information necessary for patients to use the drug safely and effectively.INSTRUCTIONS FOR USE RISPERIDONE ORAL SOLUTION, USP Read these Instructions for Use before you start using Risperidone Oral Solution and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. Important information you need to know before taking Risperidone Oral Solution: Take Risperidone Oral Solution exactly as your healthcare provider tells you to take it. Each 1 mL contains 1 mg of Risperidone Oral Solution. Ask your healthcare provider or pharmacist to show you how to measure your prescribed dose using the oral dosing syringe. Always use the oral dosing syringe that comes with Risperidone Oral Solution. Contact your healthcare provider or pharmacist if you lose or damage the oral dosing syringe, or if your carton does not come with one. Risperidone Oral Solution can be taken directly from the oral dosing syringe or mixed with water, coffee, orange juice, or low-fat milk. Do not mix Risperidone Oral Solution with cola or tea. Each Risperidone Oral Solution carton contains: 1 bottle of Risperidone Oral Solution 1 oral dosing syringe Gather and check supplies: Gather the Risperidone Oral Solution bottle and oral dosing syringe. Check the expiration date on the bottle. Do not use the bottle of Risperidone Oral Solution if the expiration date has passed. Check your dose in mLs as prescribed by your healthcare provider. Find this mL marking on the plunger of the oral dosing syringe. If your dose is more than 3 mL, you will need to divide your dose. Follow the instructions given to you by your healthcare provider or pharmacist on how to divide your dose. Preparing a dose of Risperidone Oral Solution: Step 1. Place the Risperidone Oral Solution bottle on a flat surface. Push down on the cap while turning it to the left (counterclockwise) to open the bottle. Step 2. Push the plunger of the oral dosing syringe all the way down. Step 3. With the bottle in an upright position, fully insert the oral dosing syringe into the opening of the bottle. Step 4. Withdraw the prescribed dose of Risperidone Oral Solution from the bottle. Hold down the barrel of the oral dosing syringe with one hand. With your other hand, slowly pull the plunger up until you reach the mL markings on the barrel for the prescribed dose. Step 5. Remove the oral dosing syringe from the bottle by holding the outer barrel and pulling straight up. Be careful not to push down on the plunger during this step. Check the oral dosing syringe for air bubbles. If you see air bubbles, slowly push the plunger all the way down to return the oral solution into the bottle. Then repeat Step 4 to withdraw the prescribed dose. Step 6. Risperidone Oral Solution can be mixed with a drink or taken directly from the oral dosing syringe. Mix the dose of Risperidone Oral Solution with water, coffee, orange juice, or low-fat milk. Stir well and drink all of the mixture right away to ensure the full dose is taken. See Figure 6a . Do not mix Risperidone Oral Solution with cola or tea. Or To take the Risperidone Oral Solution dose directly from the oral dosing syringe, place the tip of the oral dosing syringe into the mouth and toward the cheek. Slowly push the plunger all the way down to gently release all of the medicine in the oral dosing syringe. Do not squirt or forcefully push the medicine into the back of the throat. See Figure 6b . Step 7. Place the cap back on the Risperidone Oral Solution bottle and turn the cap to the right (clockwise) to close the bottle. Step 8. Rinse the oral dosing syringe with water after each use. Remove the plunger from the oral dosing syringe barrel. Rinse the oral dosing syringe barrel and plunger with water and let them air dry. When the oral dosing syringe barrel and plunger are dry, put the plunger back into the oral dosing syringe barrel for the next use. Do not throw away the oral dosing syringe. Storing Risperidone Oral Solution: Store Risperidone Oral Solution at controlled room temperature 20° to 25°C (68° to 77°F). Do not freeze Risperidone Oral Solution. Protect from light. Keep Risperidone Oral Solution and all medicines out of the reach of children. This Instructions for Use has been approved by the U.S. Food and Drug Administration. Revised: 04/2023 Repackaged and Distributed By: Remedy Repack, Inc. 625 Kolter Dr. Suite #4 Indiana, PA 1-724-465-8762 New Image Step1 New Image Step 3 Step 4 Step 5 Step 6a Step 6b Step 7 Step 8
|
| |
|
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES 14.1 Schizophrenia Adults Short-Term Efficacy The efficacy of risperidone in the treatment of schizophrenia was established in four short-term (4- to 8-week) controlled trials of psychotic inpatients who met DSM-III-R criteria for schizophrenia. Several instruments were used for assessing psychiatric signs and symptoms in these studies, among them the Brief Psychiatric Rating Scale (BPRS), a multi-item inventory of general psychopathology traditionally used to evaluate the effects of drug treatment in schizophrenia. The BPRS psychosis cluster (conceptual disorganization, hallucinatory behavior, suspiciousness, and unusual thought content) is considered a particularly useful subset for assessing actively psychotic schizophrenic patients. A second traditional assessment, the Clinical Global Impression (CGI), reflects the impression of a skilled observer, fully familiar with the manifestations of schizophrenia, about the overall clinical state of the patient. In addition, the Positive and Negative Syndrome Scale (PANSS) and the Scale for Assessing Negative Symptoms (SANS) were employed. The results of the trials follow: (1) In a 6-week, placebo-controlled trial (n = 160) involving titration of risperidone in doses up to 10 mg/day (twice-daily schedule), risperidone was generally superior to placebo on the BPRS total score, on the BPRS psychosis cluster, and marginally superior to placebo on the SANS. (2) In an 8-week, placebo-controlled trial (n = 513) involving 4 fixed doses of risperidone (2 mg/day, 6 mg/day, 10 mg/day, and 16 mg/day, on a twice-daily schedule), all 4 risperidone groups were generally superior to placebo on the BPRS total score, BPRS psychosis cluster, and CGI severity score; the 3 highest risperidone dose groups were generally superior to placebo on the PANSS negative subscale. The most consistently positive responses on all measures were seen for the 6 mg dose group, and there was no suggestion of increased benefit from larger doses. (3) In an 8-week, dose comparison trial (n = 1356) involving 5 fixed doses of risperidone (1 mg/day, 4 mg/day, 8 mg/day, 12 mg/day, and 16 mg/day, on a twice-daily schedule), the four highest risperidone dose groups were generally superior to the 1 mg risperidone dose group on BPRS total score, BPRS psychosis cluster, and CGI severity score. None of the dose groups were superior to the 1 mg group on the PANSS negative subscale. The most consistently positive responses were seen for the 4 mg dose group. (4) In a 4-week, placebo-controlled dose comparison trial (n = 246) involving 2 fixed doses of risperidone (4 and 8 mg/day on a once-daily schedule), both risperidone dose groups were generally superior to placebo on several PANSS measures, including a response measure (>20% reduction in PANSS total score), PANSS total score, and the BPRS psychosis cluster (derived from PANSS). The results were generally stronger for the 8 mg than for the 4 mg dose group. Long-Term Efficacy In a longer-term trial, 365 adult outpatients predominantly meeting DSM-IV criteria for schizophrenia and who had been clinically stable for at least 4 weeks on an antipsychotic medication were randomized to risperidone (2 to 8 mg/day) or to an active comparator, for 1 to 2 years of observation for relapse. Patients receiving risperidone experienced a significantly longer time to relapse over this time period compared to those receiving the active comparator. Pediatrics The efficacy of risperidone in the treatment of schizophrenia in adolescents aged 13 to 17 years was demonstrated in two short-term (6 and 8 weeks), double-blind controlled trials. All patients met DSM-IV diagnostic criteria for schizophrenia and were experiencing an acute episode at time of enrollment. In the first trial (study #1), patients were randomized into one of three treatment groups: risperidone 1 to 3 mg/day (n = 55, mean modal dose = 2.6 mg), risperidone 4 to 6 mg/day (n = 51, mean modal dose = 5.3 mg), or placebo (n = 54). In the second trial (study #2), patients were randomized to either risperidone 0.15 to 0.6 mg/day (n = 132, mean modal dose = 0.5 mg) or risperidone 1.5 to 6 mg/day (n = 125, mean modal dose = 4 mg). In all cases, study medication was initiated at 0.5 mg/day (with the exception of the 0.15 to 0.6 mg/day group in study #2, where the initial dose was 0.05 mg/day) and titrated to the target dosage range by approximately Day 7. Subsequently, dosage was increased to the maximum tolerated dose within the target dose range by Day 14. The primary efficacy variable in all studies was the mean change from baseline in total PANSS score. Results of the studies demonstrated efficacy of risperidone in all dose groups from 1 to 6 mg/day compared to placebo, as measured by significant reduction of total PANSS score. The efficacy on the primary parameter in the 1 to 3 mg/day group was comparable to the 4 to 6 mg/day group in study #1, and similar to the efficacy demonstrated in the 1.5 to 6 mg/day group in study #2. In study #2, the efficacy in the 1.5 to 6 mg/day group was statistically significantly greater than that in the 0.15 to 0.6 mg/day group. Doses higher than 3 mg/day did not reveal any trend towards greater efficacy. 14.2 Bipolar Mania - Monotherapy Adults The efficacy of risperidone in the treatment of acute manic or mixed episodes was established in two short-term (3-week) placebo-controlled trials in patients who met the DSM-IV criteria for Bipolar I Disorder with manic or mixed episodes. These trials included patients with or without psychotic features. The primary rating instrument used for assessing manic symptoms in these trials was the Young Mania Rating Scale (YMRS), an 11-item clinician-rated scale traditionally used to assess the degree of manic symptomatology (irritability, disruptive/aggressive behavior, sleep, elevated mood, speech, increased activity, sexual interest, language/thought disorder, thought content, appearance, and insight) in a range from 0 (no manic features) to 60 (maximum score). The primary outcome in these trials was change from baseline in the YMRS total score. The results of the trials follow: (1) In one 3-week placebo-controlled trial (n = 246), limited to patients with manic episodes,; which involved a dose range of risperidone 1 to 6 mg/day, once daily, starting at 3 mg/day; (mean modal dose was 4.1 mg/day), risperidone was superior to placebo in the reduction; of YMRS total score. (2) In another 3-week placebo-controlled trial (n = 286), which involved a dose range of 1 to 6 mg/day, once daily, starting at 3 mg/day (mean modal dose was 5.6 mg/day), risperidone was superior to placebo in the reduction of YMRS total score. Pediatrics; The efficacy of risperidone in the treatment of mania in children or adolescents with Bipolar I; disorder was demonstrated in a 3-week, randomized, double-blind, placebo-controlled,; multicenter trial including patients ranging in ages from 10 to 17 years who were experiencing a; manic or mixed episode of bipolar I disorder. Patients were randomized into one of three treatment groups: risperidone 0.5 to 2.5 mg/day (n = 50, mean modal dose = 1.9 mg), risperidone 3 to 6 mg/day (n = 61, mean modal dose = 4.7 mg), or placebo (n = 58). In all cases, study medication was initiated at 0.5 mg/day and titrated to the target dosage range by Day 7, with further increases in dosage to the maximum tolerated dose within the targeted dose range by Day 10. The primary rating instrument used for assessing efficacy in this study was the mean change from baseline in the total YMRS score. Results of this study demonstrated efficacy of risperidone in both dose groups compared with placebo, as measured by significant reduction of total YMRS score. The efficacy on the primary parameter in the 3 to 6 mg/day dose group was comparable to the 0.5 to 2.5 mg/day dose group.; Doses higher than 2.5 mg/day did not reveal any trend towards greater efficacy. 14.3 Bipolar Mania – Adjunctive Therapy with Lithium or Valproate The efficacy of risperidone with concomitant lithium or valproate in the treatment of acute manic or mixed episodes was established in one controlled trial in adult patients who met the DSM-IV criteria for Bipolar I Disorder. This trial included patients with or without psychotic features and with or without a rapid-cycling course. (1) In this 3-week placebo-controlled combination trial, 148 in- or outpatients on lithium or valproate therapy with inadequately controlled manic or mixed symptoms were randomized to receive risperidone, placebo, or an active comparator, in combination with their original therapy. Risperidone, in a dose range of 1 to 6 mg/day, once daily, starting at 2 mg/day (mean modal dose of 3.8 mg/day), combined with lithium or valproate (in a therapeutic range of 0.6 mEq/L to 1.4 mEq/L or 50 mcg/mL to 120 mcg/mL, respectively) was superior to lithium or valproate alone in the reduction of YMRS total score. (2) In a second 3-week placebo-controlled combination trial, 142 in- or outpatients on lithium, valproate, or carbamazepine therapy with inadequately controlled manic or mixed symptoms were randomized to receive risperidone or placebo, in combination with their original therapy. Risperidone, in a dose range of 1 to 6 mg/day, once daily, starting at 2 mg/day (mean modal dose of 3.7 mg/day), combined with lithium, valproate, or carbamazepine (in therapeutic ranges of 0.6 mEq/L to 1.4 mEq/L for lithium, 50 mcg/mL to 125 mcg/mL for valproate, or 4 to 12 mcg/mL for carbamazepine, respectively) was not superior to lithium, valproate, or carbamazepine alone in the reduction of YMRS total score. A possible explanation for the failure of this trial was induction of risperidone and 9-hydroxyrisperidone clearance by carbamazepine, leading to subtherapeutic levels of risperidone and 9-hydroxyrisperidone. 14.4 Irritability Associated with Autistic Disorder Short-Term Efficacy The efficacy of risperidone in the treatment of irritability associated with autistic disorder was established in two 8-week, placebo-controlled trials in children and adolescents (aged 5 to 16 years) who met the DSM-IV criteria for autistic disorder. Over 90% of these subjects were under 12 years of age and most weighed over 20 kg (16 to 104.3 kg). Efficacy was evaluated using two assessment scales: the Aberrant Behavior Checklist (ABC) and the Clinical Global Impression - Change (CGI-C) scale. The primary outcome measure in both trials was the change from baseline to endpoint in the Irritability subscale of the ABC (ABC-I).; The ABC-I subscale measured the emotional and behavioral symptoms of autism, including; aggression towards others, deliberate self-injuriousness, temper tantrums, and quickly changing; moods. The CGI-C rating at endpoint was a co-primary outcome measure in one of the studies. The results of these trials are as follows: (1) In one of the 8-week, placebo-controlled trials, children and adolescents with autistic disorder (n = 101), aged 5 to 16 years, received twice daily doses of placebo or risperidone 0.5 to 3.5 mg/day on a weight-adjusted basis. Risperidone, starting at 0.25 mg/day or 0.5 mg/day depending on baseline weight (< 20 kg and ≥ 20 kg, respectively) and titrated to clinical response (mean modal dose of 1.9 mg/day, equivalent to 0.06 mg/kg/day), significantly improved scores on the ABC-I subscale and on the CGI-C scale compared with placebo. (2) In the other 8-week, placebo-controlled trial in children with autistic disorder (n = 55), aged 5 to 12 years, risperidone 0.02 to 0.06 mg/kg/day given once or twice daily, starting at 0.01 mg/kg/day and titrated to clinical response (mean modal dose of 0.05 mg/kg/day, equivalent to 1.4 mg/day), significantly improved scores on the ABC-I subscale compared with placebo. A third trial was a 6-week, multicenter, randomized, double-blind, placebo-controlled, fixed-dose study to evaluate the efficacy and safety of a lower than recommended dose of risperidone in subjects (N = 96) 5 to 17 years of age with autistic disorder (defined by DSM-IV criteria) and associated irritability and related behavioral symptoms. Approximately 77% of patients were younger than 12 years of age (mean age = 9), and 88% were male. Most patients (73%) weighed less than 45 kg (mean weight = 40 kg). Approximately 90% of patients were antipsychotic-naïve before entering the study. There were two weight-based, fixed doses of risperidone (high-dose and low-dose). The high dose was 1.25 mg per day for patients weighing 20 to < 45 kg, and it was 1.75 mg per day for patients weighing ≥ 45 kg. The low dose was 0.125 mg per day for patients weighing 20 to < 45 kg, and it was 0.175 mg per day for patients weighing ≥ 45 kg. The dose was administered once daily in the morning, or in the evening if sedation occurred. The primary efficacy endpoint was the mean change in the Aberrant Behavior Checklist – Irritability subscale (ABC-I) score from baseline to the end of Week 6. The study demonstrated the efficacy of high-dose risperidone, as measured by the mean change in ABC-I score. It did not demonstrate efficacy for low-dose risperidone. The mean baseline ABC-I scores were 29 in the placebo group (n = 35), 27 in the risperidone low-dose group (n = 30), and 28 in the risperidone high-dose group (n = 31). The mean changes in ABC-I scores were -3.5, -7.4, and -12.4 in the placebo, low-dose, and high-dose group respectively. The results in the high-dose group were statistically significant (p< 0.001) but not in the low-dose group (p = 0.164). Long-Term Efficacy Following completion of the first 8-week double-blind study, 63 patients entered an open-label study extension where they were treated with risperidone for 4 or 6 months (depending on whether they received risperidone or placebo in the double-blind study). During this open-label treatment period, patients were maintained on a mean modal dose of risperidone of 1.8 to 2.1 mg/day (equivalent to 0.05 - 0.07 mg/kg/day). Patients who maintained their positive response to risperidone (response was defined as ≥ 25% improvement on the ABC-I subscale and a CGI-C rating of ‘much improved’ or ‘very much improved’) during the 4 to 6 month open-label treatment phase for about 140 days, on average, were randomized to receive risperidone or placebo during an 8-week, double-blind withdrawal study (n = 39 of the 63 patients). A pre-planned interim analysis of data from patients who completed the withdrawal study (n = 32), undertaken by an independent Data Safety Monitoring Board, demonstrated a significantly lower relapse rate in the risperidone group compared with the placebo group. Based on the interim analysis results, the study was terminated due to demonstration of a statistically significant effect on relapse prevention. Relapse was defined as ≥ 25% worsening on the most recent assessment of the ABC-I subscale (in relation to baseline of the randomized withdrawal phase).
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS Pregnancy: May cause extrapyramidal and/or withdrawal symptoms in neonates with third trimester exposure.;( 8.1)
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.Risperidone Oral Solution, USP;1 mg/mL;is supplied in NDC: 70518-3741-00 NDC: 70518-3741-01 PACKAGING: 10 in 1 BOX PACKAGING: 2 mL in 1 CUP, UNIT DOSE Risperidone Oral Solution, USP;1 mg/mL;should be stored at controlled room temperature;20° to 25°C (68° to 77°F) [see USP Controlled Room Temperature]. Protect from light and freezing. Light Sensitive:;Store in carton, away from direct sunlight. Keep out of reach of children. Repackaged and Distributed By: Remedy Repack, Inc. 625 Kolter Dr. Suite #4 Indiana, PA 1-724-465-8762
Boxed warning
Information about contraindications or serious warnings, particularly those that may lead to death or serious injury.WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Risperidone is not approved for the treatment of patients with dementia-related psychosis [ see Warnings and Precautions (5.1 ) ]. WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS See full prescribing information for complete boxed warning. Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Risperidone is not approved for use in patients with dementia-related psychosis. ( 5.1 )
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API