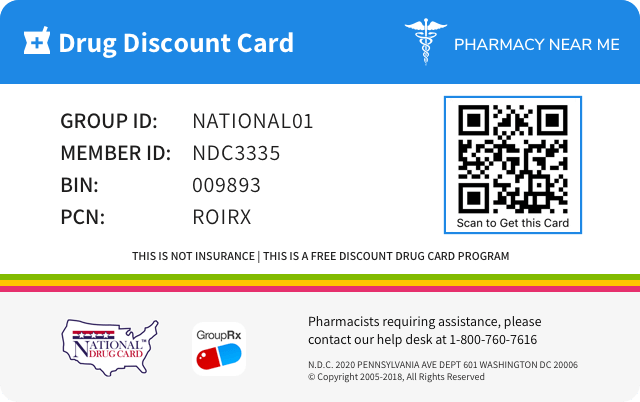
Save up to 80% by drug discount in your pharmacy with "Pharmacy Near Me - National Drug Discount Card"
You can scan QR Code(just open camera on your phone/scan by application) from the image on prescription drug discount card to save it to your mobile phone. Or just click on image if you're on mobile phone.
![]()
![]()
| Product NDC Code | 47783-101 | ||||
|---|---|---|---|---|---|
| Drug Name | Kalbitor |
||||
| Type | Brand | ||||
| Pharm Class | Kallikrein Inhibitors [MoA], Plasma Kallikrein Inhibitor [EPC] |
||||
| Active Ingredients |
|
||||
| Route | SUBCUTANEOUS | ||||
| Dosage Form | INJECTION, SOLUTION | ||||
| RxCUI drug identifier | 884698, 884702 |
||||
| Application Number | BLA125277 | ||||
| Labeler Name | Takeda Pharmaceuticals America, Inc. | ||||
| Packages |
|
||||
| Check if available Online | Get Medication Prices online with Discount |
Overdosage of Kalbitor
Information about signs, symptoms, and laboratory findings of acute ovedosage and the general principles of overdose treatment.10 OVERDOSAGE There have been no reports of overdose with KALBITOR. HAE patients have received single doses up to 90 mg intravenously without evidence of dose-related toxicity.
Adverse reactions
Information about undesirable effects, reasonably associated with use of the drug, that may occur as part of the pharmacological action of the drug or may be unpredictable in its occurrence. Adverse reactions include those that occur with the drug, and if applicable, with drugs in the same pharmacologically active and chemically related class. There is considerable variation in the listing of adverse reactions. They may be categorized by organ system, by severity of reaction, by frequency, by toxicological mechanism, or by a combination of these.6 ADVERSE REACTIONS Hypersensitivity reactions, including anaphylaxis, have occurred in patients treated with KALBITOR [ see Contraindications (4) and Warnings and Precautions (5.1) ]. The most common adverse reactions occurring in ≥3% of KALBITOR-treated patients and greater than placebo are headache, nausea, diarrhea, pyrexia, injection site reactions, and nasopharyngitis. ( 6 ) To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals at 1-800-828-2088 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. 6.1 Clinical Trials Experience Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The safety data described below reflect exposure to KALBITOR in 255 patients with HAE treated with either intravenous or subcutaneous KALBITOR. Of the 255 patients, 66% of patients were female and 86% were Caucasian. Patients treated with KALBITOR were between the ages of 10 and 78 years. Overall, the most common adverse reactions in 255 patients with HAE were headache (16%), nausea (13%), fatigue (12%), diarrhea (11%), upper respiratory tract infection (8%), injection site reactions (7%), nasopharyngitis (6%), vomiting (6%), pruritus (5%), upper abdominal pain (5%), and pyrexia (5%). Anaphylaxis was reported in 4% of patients with HAE. Injection site reactions were characterized by local pruritus, erythema, pain, irritation, urticaria, and/or bruising. The incidence of adverse reactions below is based upon 2 placebo-controlled, clinical trials (EDEMA3 ® and EDEMA4 ® ) in a total of 143 unique patients with HAE. Patients were treated with KALBITOR 30 mg subcutaneous or placebo. Patients were permitted to participate sequentially in both placebo-controlled trials; safety data collected during exposure to KALBITOR was attributed to treatment with KALBITOR, and safety data collected during exposure to placebo was attributed to treatment with placebo. Table 1 shows adverse reactions occurring in ≥3% of KALBITOR-treated patients that also occurred at a higher rate than in the placebo-treated patients in the two controlled trials (EDEMA3 and EDEMA4) of the 30 mg subcutaneous dose. Table 1: Adverse Reactions Occurring at ≥3% and Higher than Placebo in 2 Placebo Controlled Clinical Trials in Patients with HAE Treated with KALBITOR KALBITOR N=100 Placebo N=81 Adverse Reactions n (%) Patients experiencing more than 1 event with the same preferred term are counted only once for that preferred term. n (%) Headache 8 (8%) 6 (7%) Nausea 5 (5%) 1 (1%) Diarrhea 4 (4%) 3 (4%) Pyrexia 4 (4%) 0 Injection site reactions 3 (3%) 1 (1%) Nasopharyngitis 3 (3%) 0 Some patients in EDEMA3 and EDEMA4 received a second, open-label 30 mg subcutaneous dose of KALBITOR within 24 hours following the initial dose. Adverse reactions reported by these patients who received the additional 30 mg subcutaneous dose of KALBITOR were consistent with those reported in the patients receiving a single dose. 6.2 Immunogenicity In the KALBITOR HAE program, patients developed antibodies to KALBITOR. Rates of seroconversion increased with exposure to KALBITOR over time. Overall, 20.2% of patients seroconverted to anti-ecallantide antibodies. Neutralizing antibodies to ecallantide were determined in vitro to be present in 8.8% of patients and were not associated with loss of efficacy. Anti-ecallantide IgE antibodies were detected at a rate of 4.7% for tested patients, and anti- P. pastoris IgE antibodies were also detected at a rate of 20.2%. Patients who seroconvert may be at a higher risk of a hypersensitivity reaction. The long-term effects of antibodies to KALBITOR are not known. The test results for the ecallantide program were determined using one of two assay formats: ELISA and bridging electrochemiluminescence (ECL). As with all therapeutic proteins, there is a potential for immunogenicity with the use of KALBITOR. The incidence of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to KALBITOR with the incidence of antibodies to other products may be misleading. 6.3 Postmarketing Experience Similar adverse reactions have been observed postmarketing as described for clinical trial experience. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate frequency or to establish a causal relationship with drug exposure.
| KALBITOR N=100 | Placebo N=81 | |
|---|---|---|
| Adverse Reactions | n (%) | n (%) |
| Headache | 8 (8%) | 6 (7%) |
| Nausea | 5 (5%) | 1 (1%) |
| Diarrhea | 4 (4%) | 3 (4%) |
| Pyrexia | 4 (4%) | 0 |
| Injection site reactions | 3 (3%) | 1 (1%) |
| Nasopharyngitis | 3 (3%) | 0 |
Kalbitor Drug Interactions
Information about and practical guidance on preventing clinically significant drug/drug and drug/food interactions that may occur in people taking the drug.7 DRUG INTERACTIONS No formal drug interactions studies were performed. No in vitro metabolism studies were performed.
Clinical pharmacology
Information about the clinical pharmacology and actions of the drug in humans.12 CLINICAL PHARMACOLOGY 12.1 Mechanism of Action Hereditary angioedema (HAE) is a rare genetic disorder caused by mutations to C1-esterase-inhibitor (C1-INH) located on Chromosome 11q and inherited as an autosomal dominant trait. HAE is characterized by low levels of C1-INH activity and low levels of C4. C1-INH functions to regulate the activation of the complement and intrinsic coagulation (contact system pathway) and is a major endogenous inhibitor of plasma kallikrein. The kallikrein-kinin system is a complex proteolytic cascade involved in the initiation of both inflammatory and coagulation pathways. One critical aspect of this pathway is the conversion of High Molecular Weight (HMW) kininogen to bradykinin by the protease plasma kallikrein. In HAE, normal regulation of plasma kallikrein activity and the classical complement cascade is therefore not present. During attacks, unregulated activity of plasma kallikrein results in excessive bradykinin generation. Bradykinin is a vasodilator which is thought by some to be responsible for the characteristic HAE symptoms of localized swelling, inflammation, and pain. KALBITOR is a potent (Ki = 25 pM), selective, reversible inhibitor of plasma kallikrein. KALBITOR binds to plasma kallikrein and blocks its binding site, inhibiting the conversion of HMW kininogen to bradykinin. By directly inhibiting plasma kallikrein, KALBITOR reduces the conversion of HMW kininogen to bradykinin and thereby treats symptoms of the disease during acute episodic attacks of HAE. 12.2 Pharmacodynamics No exposure-response relationships for KALBITOR to components of the complement or kallikrein-kinin pathways have been established. The effect of KALBITOR on activated partial thromboplastin time (aPTT) was measured because of potential effect on the intrinsic coagulation pathway. Prolongation of aPTT has been observed following intravenous dosing of KALBITOR at doses ≥20 mg/m 2 . At 80 mg administered intravenously in healthy subjects, aPTT values were prolonged approximately two-fold over baseline values and returned to normal by 4 hours post-dose. For patients taking KALBITOR, no significant QT prolongation has been seen. In a randomized, placebo-controlled trial (EDEMA4) studying the 30 mg subcutaneous dose versus placebo, 12-lead ECGs were obtained at baseline, 2 hours and 4 hours post-dose (covering the time of expected C max ), and at follow-up (day 7). ECGs were evaluated for PR interval, QRS complex, and QTc interval. KALBITOR had no significant effect on the QTc interval, heart rate, or any other components of the ECG. 12.3 Pharmacokinetics Following the administration of a single 30 mg subcutaneous dose of KALBITOR to healthy subjects, a mean (± standard deviation) maximum plasma concentration of 586 ± 106 ng/mL was observed approximately 2 to 3 hours post-dose. The mean area under the concentration-time curve was 3017 ± 402 ng*hr/mL. Following administration, plasma concentration declined with a mean elimination half-life of 2.0 ± 0.5 hours. Plasma clearance was 153 ± 20 mL/min and the volume of distribution was 26.4 ± 7.8 L. Based on a population pharmacokinetic analysis, body weight, age, and gender were not found to affect KALBITOR exposure significantly. Ecallantide is a small protein (7054 Da) and renal elimination in the urine of treated subjects has been demonstrated. No pharmacokinetic data are available in patients or subjects with hepatic or renal impairment.
Mechanism of action
Information about the established mechanism(s) of the drugÕs action in humans at various levels (for example receptor, membrane, tissue, organ, whole body). If the mechanism of action is not known, this field contains a statement about the lack of information.12.1 Mechanism of Action Hereditary angioedema (HAE) is a rare genetic disorder caused by mutations to C1-esterase-inhibitor (C1-INH) located on Chromosome 11q and inherited as an autosomal dominant trait. HAE is characterized by low levels of C1-INH activity and low levels of C4. C1-INH functions to regulate the activation of the complement and intrinsic coagulation (contact system pathway) and is a major endogenous inhibitor of plasma kallikrein. The kallikrein-kinin system is a complex proteolytic cascade involved in the initiation of both inflammatory and coagulation pathways. One critical aspect of this pathway is the conversion of High Molecular Weight (HMW) kininogen to bradykinin by the protease plasma kallikrein. In HAE, normal regulation of plasma kallikrein activity and the classical complement cascade is therefore not present. During attacks, unregulated activity of plasma kallikrein results in excessive bradykinin generation. Bradykinin is a vasodilator which is thought by some to be responsible for the characteristic HAE symptoms of localized swelling, inflammation, and pain. KALBITOR is a potent (Ki = 25 pM), selective, reversible inhibitor of plasma kallikrein. KALBITOR binds to plasma kallikrein and blocks its binding site, inhibiting the conversion of HMW kininogen to bradykinin. By directly inhibiting plasma kallikrein, KALBITOR reduces the conversion of HMW kininogen to bradykinin and thereby treats symptoms of the disease during acute episodic attacks of HAE.
Pharmacodynamics
Information about any biochemical or physiologic pharmacologic effects of the drug or active metabolites related to the drugÕs clinical effect in preventing, diagnosing, mitigating, curing, or treating disease, or those related to adverse effects or toxicity.12.2 Pharmacodynamics No exposure-response relationships for KALBITOR to components of the complement or kallikrein-kinin pathways have been established. The effect of KALBITOR on activated partial thromboplastin time (aPTT) was measured because of potential effect on the intrinsic coagulation pathway. Prolongation of aPTT has been observed following intravenous dosing of KALBITOR at doses ≥20 mg/m 2 . At 80 mg administered intravenously in healthy subjects, aPTT values were prolonged approximately two-fold over baseline values and returned to normal by 4 hours post-dose. For patients taking KALBITOR, no significant QT prolongation has been seen. In a randomized, placebo-controlled trial (EDEMA4) studying the 30 mg subcutaneous dose versus placebo, 12-lead ECGs were obtained at baseline, 2 hours and 4 hours post-dose (covering the time of expected C max ), and at follow-up (day 7). ECGs were evaluated for PR interval, QRS complex, and QTc interval. KALBITOR had no significant effect on the QTc interval, heart rate, or any other components of the ECG.
Pharmacokinetics
Information about the clinically significant pharmacokinetics of a drug or active metabolites, for instance pertinent absorption, distribution, metabolism, and excretion parameters.12.3 Pharmacokinetics Following the administration of a single 30 mg subcutaneous dose of KALBITOR to healthy subjects, a mean (± standard deviation) maximum plasma concentration of 586 ± 106 ng/mL was observed approximately 2 to 3 hours post-dose. The mean area under the concentration-time curve was 3017 ± 402 ng*hr/mL. Following administration, plasma concentration declined with a mean elimination half-life of 2.0 ± 0.5 hours. Plasma clearance was 153 ± 20 mL/min and the volume of distribution was 26.4 ± 7.8 L. Based on a population pharmacokinetic analysis, body weight, age, and gender were not found to affect KALBITOR exposure significantly. Ecallantide is a small protein (7054 Da) and renal elimination in the urine of treated subjects has been demonstrated. No pharmacokinetic data are available in patients or subjects with hepatic or renal impairment.
Contraindications
Information about situations in which the drug product is contraindicated or should not be used because the risk of use clearly outweighs any possible benefit, including the type and nature of reactions that have been reported.4 CONTRAINDICATIONS Do not administer KALBITOR to a patient who has known clinical hypersensitivity to KALBITOR. [ see Warnings and Precautions (5.1) ]. Do not administer KALBITOR to a patient who has known clinical hypersensitivity to KALBITOR. ( 4 )
Description
General information about the drug product, including the proprietary and established name of the drug, the type of dosage form and route of administration to which the label applies, qualitative and quantitative ingredient information, the pharmacologic or therapeutic class of the drug, and the chemical name and structural formula of the drug.11 DESCRIPTION KALBITOR (ecallantide) is a human plasma kallikrein inhibitor for injection for subcutaneous use. Ecallantide is a 60-amino-acid protein produced in Pichia pastoris yeast cells by recombinant DNA technology. KALBITOR is a clear and colorless, sterile, and nonpyrogenic solution. Each vial contains 10 mg ecallantide as the active ingredient, and the following inactive ingredients: 0.76 mg disodium hydrogen orthophosphate (dihydrate), 0.2 mg monopotassium phosphate, 0.2 mg potassium chloride, and 8 mg sodium chloride in water for injection, USP. KALBITOR is preservative free, with a pH of approximately 7.0. A 30 mg dose is supplied as 3 vials each containing 1 mL of 10 mg/mL KALBITOR. Vials are intended for single use.
Dosage and administration
Information about the drug product’s dosage and administration recommendations, including starting dose, dose range, titration regimens, and any other clinically sigificant information that affects dosing recommendations.2 DOSAGE AND ADMINISTRATION 30 mg (3 mL), administered subcutaneously in three 10 mg (1 mL) injections. If an attack persists, an additional dose of 30 mg may be administered within a 24 hour period. ( 2.1 ) KALBITOR should only be administered by a healthcare professional with appropriate medical support to manage anaphylaxis and hereditary angioedema. ( 2.2 ). 2.1 Recommended Dosing The recommended dose of KALBITOR is 30 mg (3 mL), administered subcutaneously in three 10 mg (1 mL) injections. If the attack persists, an additional dose of 30 mg may be administered within a 24 hour period. 2.2 Administration Instructions KALBITOR should only be administered by a healthcare professional with appropriate medical support to manage anaphylaxis and hereditary angioedema. KALBITOR should be refrigerated and protected from the light. KALBITOR is a clear, colorless liquid; visually inspect each vial for particulate matter and discoloration prior to administration. If there is particulate matter or discoloration, the vial should not be used. Using aseptic technique, withdraw 1 mL (10 mg) of KALBITOR from the vial using a large bore needle. Change the needle on the syringe to a needle suitable for subcutaneous injection. The recommended needle size is 27 gauge. Inject KALBITOR into the skin of the abdomen, thigh, or upper arm. Repeat the procedure for each of the 3 vials comprising the KALBITOR dose. The injection site for each of the injections may be in the same or in different anatomic locations (abdomen, thigh, upper arm). There is no need for site rotation. Injection sites should be separated by at least 2 inches (5 cm) and away from the anatomical site of attack. The same instructions apply to an additional dose administered within 24 hours. Different injection sites or the same anatomical location (as used for the first administration) may be used.
Dosage forms and strengths
Information about all available dosage forms and strengths for the drug product to which the labeling applies. This field may contain descriptions of product appearance.3 DOSAGE FORMS AND STRENGTHS KALBITOR is a clear, colorless liquid free of preservatives. Each vial of KALBITOR contains ecallantide at a concentration of 10 mg/mL. Single use glass vial containing 10 mg/mL of ecallantide as a solution for injection. ( 3 )
Indications and usage
A statement of each of the drug products indications for use, such as for the treatment, prevention, mitigation, cure, or diagnosis of a disease or condition, or of a manifestation of a recognized disease or condition, or for the relief of symptoms associated with a recognized disease or condition. This field may also describe any relevant limitations of use.1 INDICATIONS AND USAGE KALBITOR ® (ecallantide) is indicated for treatment of acute attacks of hereditary angioedema (HAE) in patients 12 years of age and older. KALBITOR is a plasma kallikrein inhibitor indicated for treatment of acute attacks of hereditary angioedema (HAE) in patients 12 years of age and older. ( 1 )
Spl product data elements
Usually a list of ingredients in a drug product.Kalbitor Ecallantide Ecallantide Ecallantide SODIUM PHOSPHATE, DIBASIC, DIHYDRATE Monobasic Potassium Phosphate Potassium Chloride Sodium Chloride
Carcinogenesis and mutagenesis and impairment of fertility
Information about carcinogenic, mutagenic, or fertility impairment potential revealed by studies in animals. Information from human data about such potential is part of the warnings field.13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility A two-year study was conducted in rats to assess the carcinogenic potential of KALBITOR. No evidence of tumorigenicity was observed in rats at ecallantide doses up to 10 mg/kg administered subcutaneously every three days (approximately 2-fold greater than the MRHD on an AUC basis). KALBITOR had no effects on fertility and reproductive performance in rats at maternal subcutaneous doses up to 25 mg/kg/day (approximately 2.7 times the MRHD on a mg/m 2 basis).
Nonclinical toxicology
Information about toxicology in non-human subjects.13 NONCLINICAL TOXICOLOGY 13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility A two-year study was conducted in rats to assess the carcinogenic potential of KALBITOR. No evidence of tumorigenicity was observed in rats at ecallantide doses up to 10 mg/kg administered subcutaneously every three days (approximately 2-fold greater than the MRHD on an AUC basis). KALBITOR had no effects on fertility and reproductive performance in rats at maternal subcutaneous doses up to 25 mg/kg/day (approximately 2.7 times the MRHD on a mg/m 2 basis).
Package label principal display panel
The content of the principal display panel of the product package, usually including the product’s name, dosage forms, and other key information about the drug product.PRINCIPAL DISPLAY PANEL - 10 mg/mL Vial Carton ATTENTION: Dispense the enclosed Medication Guide to each patient. NDC# 47783-101-01 KALBITOR ® ecallantide 10 mg/mL Injection For Subcutaneous Use Only Single Use; Discard Unused Portion Net Quantity: 3 Vials Rx Only PRINCIPAL DISPLAY PANEL - 10 mg/mL Vial Carton
Spl unclassified section
Information not classified as belonging to one of the other fields. Approximately 40% of labeling with effective_time between June 2009 and August 2014 have information in this field.Manufactured by: Takeda Pharmaceuticals U.S.A., Inc. Lexington, MA 02421 U.S. License No. 1898 KALBITOR ® is a registered trademark of Dyax Corp., a Takeda company. TAKEDA ® and the TAKEDA Logo ® are registered trademarks of Takeda Pharmaceutical Company Limited. © 2021 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
Kalbitor: Information for patients
Information necessary for patients to use the drug safely and effectively, such as precautions concerning driving or the concomitant use of other substances that may have harmful additive effects.17 PATIENT COUNSELING INFORMATION See FDA-approved patient labeling (Medication Guide) Advise patients that KALBITOR may cause anaphylaxis and other hypersensitivity reactions. Advise patients that KALBITOR should be administered by a healthcare professional with appropriate medical support to manage anaphylaxis and hereditary angioedema. Instruct patients who have known clinical hypersensitivity to KALBITOR not to receive additional doses of KALBITOR. [ see Boxed Warning , Contraindications (4) , and Warnings and Precautions (5.1) ] Advise patients to consult the Medication Guide for additional information regarding the risk of anaphylaxis and other hypersensitivity reactions. For more information, visit www.kalbitor.com or call 1-800-828-2088.
Spl medguide
Information about the patient medication guide that accompanies the drug product. Certain drugs must be dispensed with an accompanying medication guide. This field may contain information about when to consult the medication guide and the contents of the medication guide.Medication Guide KALBITOR ® (KAL-bi-tor) (ecallantide) Read this Medication Guide before you start receiving KALBITOR and before each treatment. There may be new information. This Medication Guide does not take the place of talking to your doctor about your medical condition or your treatment. What is the most important information that I should know about KALBITOR? Serious allergic reactions may happen in some people who receive KALBITOR. These allergic reactions can be life-threatening and usually happen within 1 hour after receiving KALBITOR. KALBITOR should be given to you by a doctor or nurse in a healthcare setting where serious allergic reactions and hereditary angioedema (HAE) can be treated. Symptoms of a serious allergic reaction to KALBITOR can be similar to the symptoms of HAE, the condition that you are being treated for. Your doctor or nurse should watch you for any signs of a serious allergic reaction after treatment with KALBITOR. Tell your doctor or nurse right away if you have any of these symptoms of a serious allergic reaction during or after treatment with KALBITOR: wheezing, shortness of breath, cough, chest tightness, or trouble breathing dizziness, fainting, fast or weak heartbeat, or feeling nervous reddening of the face, itching, hives, or feeling warm swelling of the throat or tongue, throat tightness, hoarse voice, or trouble swallowing runny nose, nasal congestion, or sneezing What is KALBITOR? KALBITOR is a prescription medicine used to treat sudden attacks of hereditary angioedema (HAE) in people 12 years of age and older. KALBITOR is not a cure for HAE. It is not known if KALBITOR is safe and effective in children under 12 years of age. Who should not receive KALBITOR? Do not receive KALBITOR if you are allergic to KALBITOR. What should I tell my doctor before I receive KALBITOR? Before receiving KALBITOR, tell your doctor if you: have ever had an allergic reaction to KALBITOR. See " Who should not receive KALBITOR? " are pregnant or plan to become pregnant. It is not known if KALBITOR will harm your unborn baby. are breast-feeding or plan to breast-feed. It is not known if KALBITOR passes into your breast milk. Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Know the medicines you take. Keep a list of them to show to your doctor and pharmacist when you get a new medicine. How will I receive KALBITOR? For each dose, you will receive 3 injections just under the skin (subcutaneous or SC injections) of your abdomen, thigh, or upper arm. What are the possible side effects? KALBITOR can cause serious allergic reactions. See " What is the most important information I should know about KALBITOR? " Common side effects of KALBITOR include: headache nausea diarrhea fever injection site reactions, such as redness, rash, swelling, itching, or bruising stuffy nose Call your doctor for advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. General information about KALBITOR Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. This Medication Guide gives you the most important information about KALBITOR. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about KALBITOR that is written for health professionals. What are the ingredients of KALBITOR? Active Ingredient: ecallantide Inactive ingredients: disodium hydrogen orthophosphate (dihydrate), monopotassium phosphate, potassium chloride, sodium chloride in water for injection. This Medication Guide has been approved by the U.S. Food and Drug Administration. For more information, visit www.kalbitor.com or call 1-800-828-2088. Manufactured by: Takeda Pharmaceuticals U.S.A., Inc. Lexington, MA 02421 U.S. License No. 1898 KALBITOR ® is a registered trademark of Dyax Corp., a Takeda company. TAKEDA ® and the TAKEDA Logo ® are registered trademarks of Takeda Pharmaceutical Company Limited. © 2021 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved. Revised: 11/2021
Clinical studies
This field may contain references to clinical studies in place of detailed discussion in other sections of the labeling.14 CLINICAL STUDIES The safety and efficacy of KALBITOR to treat acute attacks of hereditary angioedema in adolescents and adults were evaluated in 2 randomized, double-blind, placebo-controlled trials (EDEMA4 and EDEMA3) in 168 patients with HAE. Patients having an attack of hereditary angioedema, at any anatomic location, with at least 1 moderate or severe symptom, were treated with 30 mg subcutaneous KALBITOR or placebo. Because patients could participate in both trials, a total of 143 unique patients participated. Of the 143 patients, 94 were female, 123 were Caucasian, and the mean age was 36 years (range 11-77). There were 64 patients with abdominal attacks, 55 with peripheral attacks, and 24 with laryngeal attacks. In both trials, the effects of KALBITOR were evaluated using the Mean Symptom Complex Severity (MSCS) score and the Treatment Outcome Score (TOS). These endpoints evaluated attack severity (MSCS) and patient response to treatment (TOS) for an acute HAE attack. MSCS score is a point-in-time measure of symptom severity. At baseline, and post-dosing at 4 hours and 24 hours, patients rated the severity of each affected symptom on a categorical scale (0 = normal, 1 = mild, 2 = moderate, 3 = severe). Patient-reported severity was based on each patient's assessment of symptom impact on their ability to perform routine activities. Ratings were averaged to obtain the MSCS score. The endpoint was reported as the change in MSCS score from baseline. A decrease in MSCS score reflected an improvement in symptom severity; the maximum possible change toward improvement was -3. TOS is a measure of symptom response to treatment. At 4 hours and 24 hours post-dosing, patient assessment of response for each anatomic site of attack involvement was recorded on a categorical scale (significant improvement [100], improvement [50], same [0], worsening [-50], significant worsening [-100]). The response at each anatomic site was weighted by baseline severity and then the weighted scores across all involved sites were averaged to calculate the TOS. A TOS value >0 reflected an improvement in symptoms from baseline. The maximum possible score was +100. EDEMA4 EDEMA4 was a randomized, double-blind, placebo-controlled trial in which 96 patients were randomized 1:1 to receive KALBITOR 30 mg subcutaneous or placebo for acute attacks of HAE. The primary endpoint was the change from baseline in MSCS score at 4 hours, and the TOS at 4 hours was a key secondary endpoint. Patients treated with KALBITOR demonstrated a greater decrease from baseline in the MSCS than placebo and a greater TOS than patients with placebo and the results were statistically significant (Table 2). At 24 hours, patients treated with KALBITOR also demonstrated a greater decrease from baseline in the MSCS than placebo (-1.5 vs. -1.1; p = 0.04) and a greater TOS (89 vs. 55, p = 0.03). Table 2: Change in MSCS Score and TOS at 4 Hours EDEMA4 EDEMA3 KALBITOR (N=48) Placebo (N=48) KALBITOR (N=36) Placebo (N=36) MSCS: Mean Symptom Complex Severity TOS: Treatment Outcome Score CI: confidence interval Change in MSCS Score at 4 Hours n 47 42 34 35 Mean -0.8 -0.4 -1.1 -0.6 95% CI -1.0, -0.6 -0.6, -0.1 -1.4, -0.8 -0.8, -0.4 P-value 0.010 0.041 TOS at 4 Hours n 47 42 34 35 Mean 53 8 63 36 95% CI 39, 68 -12, 28 49, 76 17, 54 P-value 0.003 0.045 More patients in the placebo group (24/48, 50%) required medical intervention to treat unresolved symptoms within 24 hours compared to the KALBITOR-treated group (16/48, 33%). Some patients reported improvement following a second 30 mg subcutaneous dose of KALBITOR, administered within 24 hours following the initial dose for symptom persistence or relapse, but efficacy was not systematically assessed for the second dose. EDEMA3 EDEMA3 was a randomized, double-blind, placebo-controlled trial in which 72 patients were randomized 1:1 to receive KALBITOR or placebo for acute attacks of HAE. EDEMA3 was similar in design to EDEMA4 with the exception of the order of the prespecified efficacy endpoints. In EDEMA3, the primary endpoint was the TOS at 4 hours, and the key secondary efficacy endpoint was the change from baseline in MSCS at 4 hours. As in EDEMA4, patients treated with KALBITOR demonstrated a greater decrease from baseline in the MSCS than placebo and a greater TOS than patients treated with placebo and the results were statistically significant (Table 2). In addition, more patients in the placebo group (13/36, 36%) required medical intervention to treat unresolved symptoms within 24 hours compared to the KALBITOR-treated group (5/36, 14%).
| EDEMA4 | EDEMA3 | |||||
|---|---|---|---|---|---|---|
| KALBITOR (N=48) | Placebo (N=48) | KALBITOR (N=36) | Placebo (N=36) | |||
| MSCS: Mean Symptom Complex Severity TOS: Treatment Outcome Score CI: confidence interval | ||||||
| n | 47 | 42 | 34 | 35 | ||
| Mean | -0.8 | -0.4 | -1.1 | -0.6 | ||
| 95% CI | -1.0, -0.6 | -0.6, -0.1 | -1.4, -0.8 | -0.8, -0.4 | ||
| P-value | 0.010 | 0.041 | ||||
| n | 47 | 42 | 34 | 35 | ||
| Mean | 53 | 8 | 63 | 36 | ||
| 95% CI | 39, 68 | -12, 28 | 49, 76 | 17, 54 | ||
| P-value | 0.003 | 0.045 | ||||
Geriatric use
Information about any limitations on any geriatric indications, needs for specific monitoring, hazards associated with use of the drug in the geriatric population.8.5 Geriatric Use Clinical trials of KALBITOR did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Pediatric use
Information about any limitations on any pediatric indications, needs for specific monitoring, hazards associated with use of the drug in any subsets of the pediatric population (such as neonates, infants, children, or adolescents), differences between pediatric and adult responses to the drug, and other information related to the safe and effective pediatric use of the drug.8.4 Pediatric Use The safety and effectiveness of KALBITOR have been established in patients 12 to 17 years of age. The efficacy of KALBITOR in the 12-15 year age group is extrapolated from efficacy in patients 16 years of age and older with support from population pharmacokinetic analyses showing similar drug exposure levels in adults and adolescents [see Clinical Pharmacology (12.3) and Clinical Studies (14) ] . The safety profile observed in pediatric patients 12-17 years of age was similar to the adverse reactions observed in the overall clinical trial population [see Adverse Reactions (6.1) ] . Safety and effectiveness of KALBITOR in patients less than 12 years of age have not been established.
Pregnancy
Information about effects the drug may have on pregnant women or on a fetus. This field may be ommitted if the drug is not absorbed systemically and the drug is not known to have a potential for indirect harm to the fetus. It may contain information about the established pregnancy category classification for the drug. (That information is nominally listed in the teratogenic_effects field, but may be listed here instead.)8.1 Pregnancy Risk Summary The available data from the pharmacovigilance database for Kalbitor have not identified a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. In an animal reproduction study, increased early fetal deaths resulting in decreased live fetuses were observed in rats following treatment during the period of organogenesis at an intravenous dose approximately 1.6 times the maximum recommended human dose (MRHD) in the presence of maternal toxicity. There were no effects on embryofetal survival or structural abnormalities in rats and rabbits following treatment during the period of organogenesis with intravenous doses up to approximately 1.1 and 6 times the MRHD, respectively, or rats treated with subcutaneous doses up to 2.4 times the MRHD. In a pre- and post-natal development study with rats, there were no effects on pup survival and development with subcutaneous doses up to approximately 2.7 times the MRHD. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Data Animal Data In an embryofetal development study with rats, ecallantide administered by the intravenous route during the period of organogenesis from gestation days 7 to 17 at a dose approximately 1.6 times the MRHD (on a mg/m 2 basis at a maternal intravenous dose of 15 mg/kg/day) caused increased numbers of early resorptions and percentages of resorbed conceptuses per litter resulting in decreased numbers of live fetuses in the presence of mild maternal toxicity. No effects on embryofetal survival or structural abnormalities were observed in rats with intravenous doses up to approximately 1.1 times the MRHD (on a mg/m 2 basis with maternal intravenous dose of 10 mg/kg/day). In an embryofetal development study with rats, ecallantide administered by the subcutaneous route during the period of organogenesis from gestation days 7 to 17 at doses up to approximately 2.4 times the MRHD (on an AUC basis with maternal subcutaneous doses up to 20 mg/kg/day) had no effects on embryofetal survival or structural abnormalities. In an embryofetal development study with rabbits, ecallantide administered by the intravenous route during the period of organogenesis from gestation days 7 to 19 at doses up to approximately 6 times the MRHD (on an AUC basis with maternal intravenous doses up to 5 mg/kg/day in rabbits) had no effects on embryofetal survival or structural abnormalities. In a pre- and post-natal development study with rats, ecallantide administered by the subcutaneous route from gestation day 7 through lactation day 20 at doses up to approximately 2.7 times the MRHD (on a mg/m 2 basis with maternal subcutaneous doses up to 25 mg/kg/day) had no effects on pup survival and behavioral or physical development.
Use in specific populations
Information about use of the drug by patients in specific populations, including pregnant women and nursing mothers, pediatric patients, and geriatric patients.8 USE IN SPECIFIC POPULATIONS 8.1 Pregnancy Risk Summary The available data from the pharmacovigilance database for Kalbitor have not identified a drug-associated risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. In an animal reproduction study, increased early fetal deaths resulting in decreased live fetuses were observed in rats following treatment during the period of organogenesis at an intravenous dose approximately 1.6 times the maximum recommended human dose (MRHD) in the presence of maternal toxicity. There were no effects on embryofetal survival or structural abnormalities in rats and rabbits following treatment during the period of organogenesis with intravenous doses up to approximately 1.1 and 6 times the MRHD, respectively, or rats treated with subcutaneous doses up to 2.4 times the MRHD. In a pre- and post-natal development study with rats, there were no effects on pup survival and development with subcutaneous doses up to approximately 2.7 times the MRHD. The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively. Data Animal Data In an embryofetal development study with rats, ecallantide administered by the intravenous route during the period of organogenesis from gestation days 7 to 17 at a dose approximately 1.6 times the MRHD (on a mg/m 2 basis at a maternal intravenous dose of 15 mg/kg/day) caused increased numbers of early resorptions and percentages of resorbed conceptuses per litter resulting in decreased numbers of live fetuses in the presence of mild maternal toxicity. No effects on embryofetal survival or structural abnormalities were observed in rats with intravenous doses up to approximately 1.1 times the MRHD (on a mg/m 2 basis with maternal intravenous dose of 10 mg/kg/day). In an embryofetal development study with rats, ecallantide administered by the subcutaneous route during the period of organogenesis from gestation days 7 to 17 at doses up to approximately 2.4 times the MRHD (on an AUC basis with maternal subcutaneous doses up to 20 mg/kg/day) had no effects on embryofetal survival or structural abnormalities. In an embryofetal development study with rabbits, ecallantide administered by the intravenous route during the period of organogenesis from gestation days 7 to 19 at doses up to approximately 6 times the MRHD (on an AUC basis with maternal intravenous doses up to 5 mg/kg/day in rabbits) had no effects on embryofetal survival or structural abnormalities. In a pre- and post-natal development study with rats, ecallantide administered by the subcutaneous route from gestation day 7 through lactation day 20 at doses up to approximately 2.7 times the MRHD (on a mg/m 2 basis with maternal subcutaneous doses up to 25 mg/kg/day) had no effects on pup survival and behavioral or physical development. 8.2 Lactation Risk Summary There are no data on the presence of ecallantide in human milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for KALBITOR and any potential adverse effects on the breastfed child from KALBITOR or from the underlying maternal condition. 8.4 Pediatric Use The safety and effectiveness of KALBITOR have been established in patients 12 to 17 years of age. The efficacy of KALBITOR in the 12-15 year age group is extrapolated from efficacy in patients 16 years of age and older with support from population pharmacokinetic analyses showing similar drug exposure levels in adults and adolescents [see Clinical Pharmacology (12.3) and Clinical Studies (14) ] . The safety profile observed in pediatric patients 12-17 years of age was similar to the adverse reactions observed in the overall clinical trial population [see Adverse Reactions (6.1) ] . Safety and effectiveness of KALBITOR in patients less than 12 years of age have not been established. 8.5 Geriatric Use Clinical trials of KALBITOR did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
How supplied
Information about the available dosage forms to which the labeling applies, and for which the manufacturer or distributor is responsible. This field ordinarily includes the strength of the dosage form (in metric units), the units in which the dosage form is available for prescribing, appropriate information to facilitate identification of the dosage forms (such as shape, color, coating, scoring, and National Drug Code), and special handling and storage condition information.16 HOW SUPPLIED/STORAGE AND HANDLING KALBITOR (ecallantide) is supplied as three 10 mg/mL single-use vials packaged in a carton. Each vial contains 10 mg of ecallantide. Each vial contains a slight overfill. NDC (47783-101-01): 3 single-use vials in 1 carton KALBITOR should be kept refrigerated (2°C to 8°C/36°F to 46°F). Vials removed from refrigeration should be stored below 86°F/30°C and used within 14 days or returned to refrigeration until use. Protect vials from light until use. Do not use beyond the expiration date.
Storage and handling
Information about safe storage and handling of the drug product.KALBITOR should be kept refrigerated (2°C to 8°C/36°F to 46°F). Vials removed from refrigeration should be stored below 86°F/30°C and used within 14 days or returned to refrigeration until use. Protect vials from light until use. Do not use beyond the expiration date.
Boxed warning
Information about contraindications or serious warnings, particularly those that may lead to death or serious injury.WARNING: ANAPHYLAXIS Anaphylaxis has been reported after administration of KALBITOR. Because of the risk of anaphylaxis, KALBITOR should only be administered by a healthcare professional with appropriate medical support to manage anaphylaxis and hereditary angioedema. Healthcare professionals should be aware of the similarity of symptoms between hypersensitivity reactions and hereditary angioedema and patients should be monitored closely. Do not administer KALBITOR to patients with known clinical hypersensitivity to KALBITOR. [ see Contraindications (4) , Warnings and Precautions (5.1) , and Adverse Reactions (6) ] WARNING: ANAPHYLAXIS See full prescribing information for complete boxed warning Anaphylaxis has been reported after administration of KALBITOR ® . Because of the risk of anaphylaxis, KALBITOR should only be administered by a healthcare professional with appropriate medical support to manage anaphylaxis and hereditary angioedema. Healthcare professionals should be aware of the similarity of symptoms between hypersensitivity reactions and hereditary angioedema and patients should be monitored closely. Do not administer KALBITOR to patients with known clinical hypersensitivity to KALBITOR [ see Contraindications (4) , Warnings and Precautions (5.1) , and Adverse Reactions (6) ].
Disclaimer: Do not rely on openFDA or Phanrmacy Near Me to make decisions regarding medical care. While we make every effort to ensure that data is accurate, you should assume all results are unvalidated. Source: OpenFDA, Healthporta Drugs API