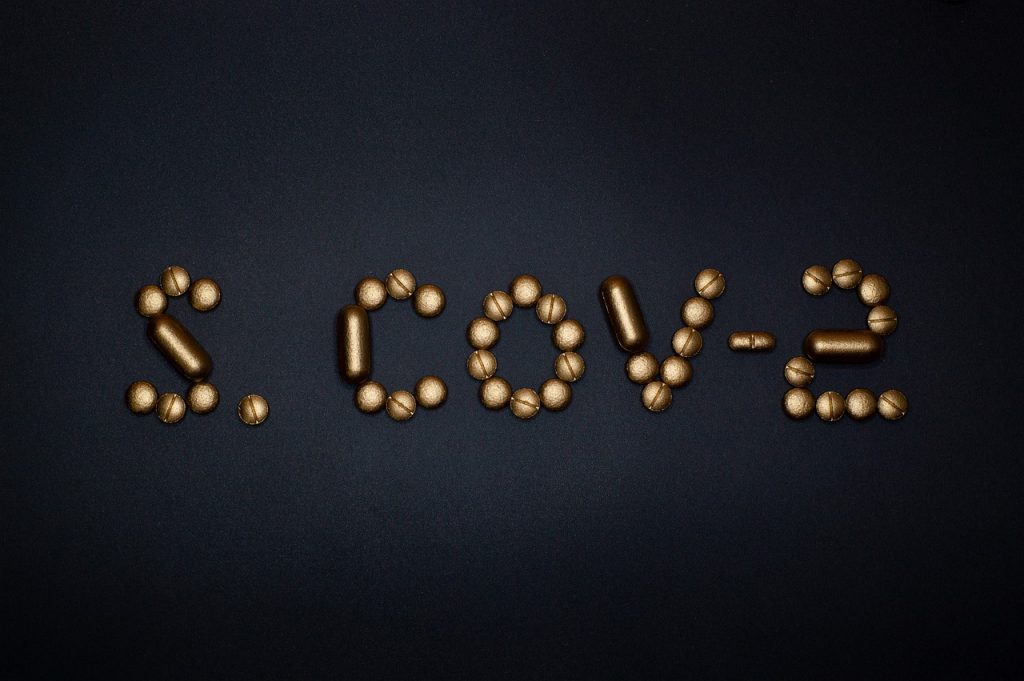
The virus that makes coronavirus virus 2019 (COVID-19) is constant for many hours to days in aerosols and on covers, according to a different library from the National Institutes of Health, Centers for Disease Control and Prevention (CDC), University of California Los Angeles (UCLA), and Princeton University scientists in The New England Journal of Medicine.
The investigators found that critical acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was detectable in aerosols for up to three hours, up to four hours on copper, up to 24 hours on cardboard, and up to two to three days on plastic and stainless steel. The results present significant knowledge about the security of SARS-CoV-2, which causes COVID-19 illness, and suggests that people may get the virus through the air and after moving infected objects.
The study report was publicly shared during the past two weeks after the researchers placed the contents on a preprint server to share their data with partners quickly.
Attempts To Stay Alive
The NIH investigators, from the National Institute of Allergy and Infectious Diseases’ Montana facility at Rocky Mountain Laboratories, compared how the environment affects SARS-CoV-2 and SARS-CoV-1, which causes SARS.
SARS-CoV-1, like its successor now traveling across the globe, emerged from China and infected more than 8,000 people in 2002 and 2003. SARS-CoV-1 was eradicated by intense contact tracing and case isolation measures, and no cases have been identified since 2004.
The NIH research attempted to mimic the virus being transferred from an infected person onto every day covers in a household or hospital setting, such as through coughing or touching objects. The investigators then examined how long the virus remains infectious on these surfaces.
The investigators highlighted supplementary observations from their study:
- If the viability of the two coronaviruses is related, why is SARS-CoV-2 resulting in more predicaments? Emerging indication suggests that people infected with SARS-CoV-2 might be spreading a virus without understanding or before noticing symptoms. This would make infection control devices that were active against SARS-CoV-1 less effective against its replacement.
- In contrast to SARS-CoV-1, most secondary characters of virus transmission of SARS-CoV-2 appear to be occurring in social settings rather than healthcare settings. Nevertheless, healthcare settings are also exposed to the introduction and spread of SARS-CoV-2. The stability of SARS-CoV-2 in aerosols and on surfaces likely adds to the transmission of the virus in healthcare settings.
The solutions affirm the guidance from public health professionals to use precautions similar to those for influenza and other respiratory diseases to prevent the spread of SARS-CoV-2:
- Avoid close communication with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
Wrapping Up
Nowadays every single medical organisation tries to prevent illness spreading, so do your best not to panic and keep reading our news!