Microbial biofilms offer a kind of healing problems by causing chronic infections, changing host immune answer, affecting therapeutic devices or environments, and supporting the emergence of antimicrobial security.
Researchers at the Lewis Katz School of Medicine at Temple University have confirmed that a unique monoclonal antibody treatment can break apart these fields of harmful bacteria, which could aid being antibiotic medicines in more efficiently clearing out germs. Their examination was announced in Nature Communications.
The researchers observed a human monoclonal antibody with pan-amyloid-binding activity, mAb 3H3, against biofilms produced by Salmonella enterica serovar Typhimurium.
The antibody was separated from a healthy human body. The research team was involved in 3H3’s ability to attach to β-amyloid.
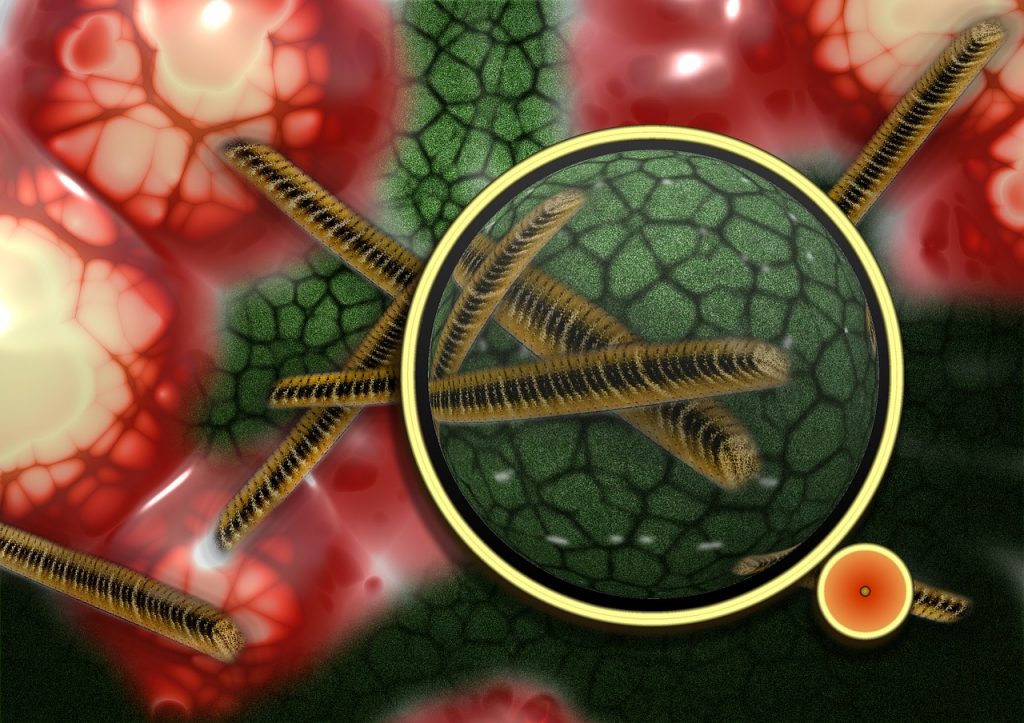
“A form of amyloid termed curli is secreted by bacterial groups and is a major part of biofilms. Bacterial amyloid curli acts like glue, enabling bacterial cells to adhere to one another and form a constant film over a cover,” according to a press release issued by Temple Health.
“The antibody disrupts the biofilm structure, enhancing biofilm eradication by antibiotics and immune cells,” the study authors wrote.
Curli fibrils are the primary component of Enterobacteriaceae biofilms protecting the bacteria from immune cells and antibiotics.
Study author Çagla Tükel, Ph.D., associate professor at the Lewis Katz School of Medicine, explained the mechanism of action to Contagion®.
A Suitable Therapy
“The hope is the antibiotics would be effective since the biofilm is broken. And the plan we chose here is to target the amyloid element that’s very common in the matrix of the enteric biofilm. This is a protein that folds into these beta-sheet structures termed curli. It comprises 85% of the extracellular matrix. If we can block the incorporation of this protein into the biofilm formation, we can open up the small building of the biofilms, and we can do a secondary procedure.”
The mAb 3H3 treatment made the Salmonella typhimurium biofilms less tightly adherent, potentially exposing them to eradication by antibiotics, which work in tandem with the antibody for efficiency that might not otherwise be feasible.
Additionally, 3H3 therapy appeared to prevent bacteria from entering circulation, where they might lead to sepsis. Therefore, the approach may even be able to reduce the risk of sepsis.
The fluoroquinolone, β-lactam, and aminoglycoside class antibiotics showed enhanced cell killing when biofilm extracellular matrices were altered by 3H3. However, more research will be required to continue growing.
“…the effects of biofilm disruption on antibiotic sensitivity will likely depend on whether the mechanism of cell killing is concentration-dependent (fluoroquinolones, aminoglycosides) or time-dependent (β-lactams). Supplementary studies will be required to explore these communications in vitro and in vivo,” research authors wrote.
All In All
Future investigations may also target other microbial biofilms. Other pathogens such as Escherichia coli, Staphylococcus aureus, and Pseudomonas aeruginosa have curli or curli-Esque amyloids in their biofilms.